On August 2020, National Institute of Statistics and Information updated population data (32,625,948 citizens)1 in which Peru became the second country with the highest mortality rate from coronavirus disease 2019 (COVID-19) around the world with 91.5 deaths per 100,000 people and a case fatality rate (CFR) of 4.32%.2 It is known public health system deficiencies could contribute to high mortality rates but sociodemographic features of individuals over 60 years old (older adult) are also matter factors which may explain the impact of the disease.
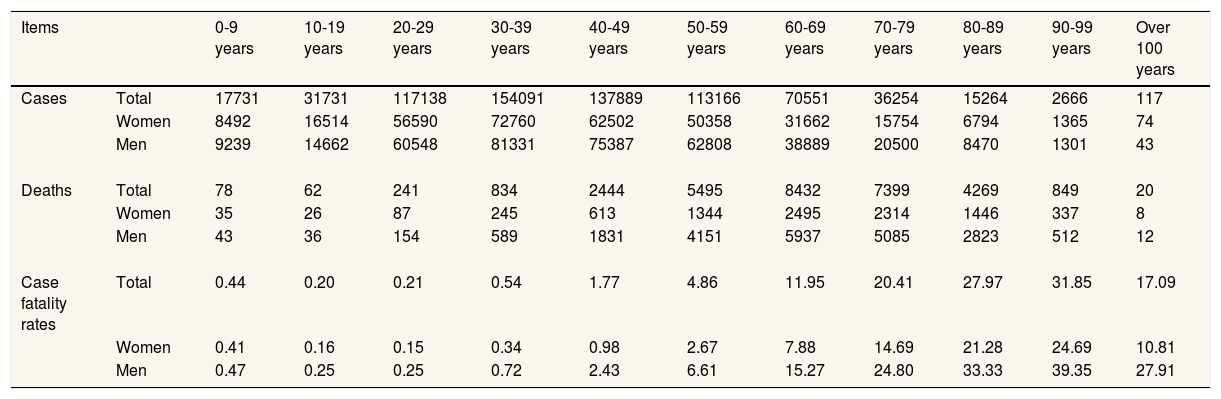
First of all, older adults are a risk group for severe COVID-19 and represent 12.7% of the national population1. In fact, almost 70% of COVID-19 deaths have been of this group age in Peru. We did not have access to the quantity data of stratified age groups but present CFRs by age and sex in Table 1. Our findings determined that males between 90-99 years was the most affected age group (CFR=39.35%). In accordance with the current evidence,3,4 we corroborated older adults and men were the most affected groups.
Cases, deaths by COVID-19 and case fatality rates (data updated September 9, 2020).
| Items | 0-9 years | 10-19 years | 20-29 years | 30-39 years | 40-49 years | 50-59 years | 60-69 years | 70-79 years | 80-89 years | 90-99 years | Over 100 years | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Total | 17731 | 31731 | 117138 | 154091 | 137889 | 113166 | 70551 | 36254 | 15264 | 2666 | 117 |
| Women | 8492 | 16514 | 56590 | 72760 | 62502 | 50358 | 31662 | 15754 | 6794 | 1365 | 74 | |
| Men | 9239 | 14662 | 60548 | 81331 | 75387 | 62808 | 38889 | 20500 | 8470 | 1301 | 43 | |
| Deaths | Total | 78 | 62 | 241 | 834 | 2444 | 5495 | 8432 | 7399 | 4269 | 849 | 20 |
| Women | 35 | 26 | 87 | 245 | 613 | 1344 | 2495 | 2314 | 1446 | 337 | 8 | |
| Men | 43 | 36 | 154 | 589 | 1831 | 4151 | 5937 | 5085 | 2823 | 512 | 12 | |
| Case fatality rates | Total | 0.44 | 0.20 | 0.21 | 0.54 | 1.77 | 4.86 | 11.95 | 20.41 | 27.97 | 31.85 | 17.09 |
| Women | 0.41 | 0.16 | 0.15 | 0.34 | 0.98 | 2.67 | 7.88 | 14.69 | 21.28 | 24.69 | 10.81 | |
| Men | 0.47 | 0.25 | 0.25 | 0.72 | 2.43 | 6.61 | 15.27 | 24.80 | 33.33 | 39.35 | 27.91 |
On the other hand, 42% and 29.5% of nuclear and extended families had at least one older adult respectively; and 19.6% were one-older adult households1, so they might be exposed to potential cases. In order to contain COVID-19, Peruvian government has implemented several strategies and diffuse mainly precautionary measures through the media. Nevertheless, 66.3% and 61.1% of households with at least one older adult do not have internet service and cable television, respectively and almost 17 out of every 100 older adults are illiterate at the national level1. These conditions may make it difficult the access to preventive information.
Staying at home has also been recommended but this is unlikely because 14.9% of older adults are in poverty, more than half who work (53.5%) are independent and 63% does not have any retirement system3. Furthermore, 63% of the national population, with at least one older adult, do not have a refrigerator.1 These characteristics influence this group in order to go out street or to work in informal jobs, exposing themselves to contagion risk and possible adverse outcomes.
Finally, another recommendation to avoid COVID-19 is frequent hand washing. Indeed, it has been recognized as the most efficient form of prevention among Peruvian general population (98.2%).5 Although, 10% of households, with at least one older adult, still do not have a public water supply network.1
COVID-19 pandemic affected Peru in a vulnerability context for the older population. This letter suggests sociodemographic components, including age, sex, type of household, the situation of internet service and cable television, illiteracy, economic situation, job category, the state of retirement system, the possession of refrigerator and the condition of water service, are potential key factors in shaping the pattern of COVID-19 deaths across the country. It is necessary to find a suitable way to support and reach this risk population.
Availability of dataThe data of COVID-19 cases and deaths used in this letter are freely available online in Spanish at National Open Data Platform: https://www.datosabiertos.gob.pe/search/field_topic/covid-19-917?sort_by=changed.
Authorship contributionsJ.D. Mendoza-Saldaña and J.E. Viton-Rubio contributed to conceptualization, data curation, formal analysis, writing-original draft, writing-review and editing. Authors guarantee the precision, transparency and honesty of the data and information contained in the letter; no relevant information has been omitted; and that all discrepancies between authors have been adequately resolved.
FundingNone.
Conflicts of interestNone.