To examine the factors that influence informed participation in a Colorectal Cancer Screening Programme (CRCSP) from a gender perspective.
MethodsCross-sectional telephone survey directed to men and women invited to participate (2009-2010) in the Valencian Community CRCSP (Spain). Sample size: 785 subjects. Outcome variables: participation in CRCSP and being informed. Bivariate and multivariate analysis using logistic regression models (95% confidence interval [95%CI], p <0.05).
ResultsBeing a woman (odds ratio [OR]: 1.52; 95%CI: 1.06-2.19), receiving information from a general practitioner (OR: 1.64; 95%CI: 1.05-2.55) and being informed (OR: 1.54; 95%CI: 1.08-2.21) are related to participation. Men are more likely to participate if they live with a partner (OR: 6.26; 95%CI: 1.82-21.49); and are more informed if they have family responsibilities (OR: 2.53; 95%CI: 1.39-4.63).
ConclusionInformation about CRCSP, involving primary health care professionals and including specific actions directed at men and at women, could contribute to improve informed participation with a gender equity perspective.
Examinar los factores que influyen en la participación informada en un Programa de Prevención del Cáncer Colorrectal (PPCCR) desde una perspectiva de género.
MétodosEstudio transversal mediante encuesta telefónica a hombres y mujeres invitados a participar (2009-2010) en el PPCCR de la Comunidad Valenciana. Tamaño muestral: 785 sujetos. Variables resultado: participación en el PPCCR y estar informado/a. Análisis bivariado y multivariado mediante modelos de regresión logística (intervalo de confianza del 95% [IC95%], p <0,05).
ResultadosSer mujer (odds ratio [OR]: 1,52; IC95%: 1,06-2,19), recibir información del médico/a de atención primaria (OR: 1,64; IC95%: 1,05-2,55) y estar informado/a (OR: 1,54; IC95%: 1,08-2,21) está relacionado con la participación en el PPCCR. Los hombres tienen más probabilidad de participar en el PPCCR si viven en pareja (OR: 6,26; IC95%: 1,82-21,49), y están más informados si tienen responsabilidades familiares (OR: 2,53; IC95%: 1,39-4,63).
ConclusiónInformar sobre el PPCCR, con implicación de los profesionales de atención primaria, mediante acciones específicas para hombres y mujeres, puede contribuir a mejorar la participación informada desde una perspectiva de equidad de género.
Participation in colorectal cancer screening programmes (CRCSP) has been shown to have benefits for health but also adverse effects.1 Informing the population of both benefits and harms of screening helps to encourage informed decision-making, however the foundations for doing so are yet to be established.2
Informed decision-making in health has been defined by several authors3,4 and despite the fact that no validated measurement exists,5 the majority agree that it must be based on accessible, up-to-date, relevant and unbiased information about the disease and the benefits and risks of making the decision.
Informed participation is considered in this study as the relationship between participation in CRCSP and the level of knowledge of the benefits and harms of participating in such programmes. In order to increase both participation and informed decision-making in these programmes (from now on informed participation), on the basis of European recommendations6 knowledge of the factors that influence both participation and knowledge is of the utmost importance. There is much evidence supporting that men participate less than women in such programmes7 but little is known about if they are also less informed and if this influences their participation.
Within the context of the Valencian Community (VC, Spain) Colorectal Cancer Screening Programme (CRCSP) a study was performed to evaluate the factors influencing participation. Gender inequalities in the reasons for participating in that programme have been identified.8 This paper aims to further examine the factors that influence informed participation in the VC CRCSP from a gender perspective.
MethodsDesign and subjectsCross-sectional survey by means of a telephone questionnaire was performed. The population study were men and women aged from 50 to 74 years old invited to participate, including initial and successive invitations, in the VC CRCSP between October 2009 and September 2010.
A 23 question ad hoc questionnaire was designed (available at Annex I, online supplementary material).
Stratified random sampling was conducted by simple allocation depending on participation or not in the programme (5% error, 5% accuracy, 50% proportion), and sampling by quotas for sex and age. A total of 785 (401 CRCSP participants and 384 non-participants) questionnaires were administered and the response rate was 59.61%
A more detailed description of the study methodology and the invitation process of the VC CRCSP may be found in the study by Molina-Barceló et al.8
VariablesThe outcome variables are participation in the CRCSP and being informed (both of the CRC disease as well as the CRCSP). Participation refers to previous performance of the fecal occult blood test (according to the information included in the programme's database); and being informed is defined according to the questionnaire responses by having a medium/high knowledge level (KL) (from 3 to 5 correct answers) on each of the specific dimensions: CRC risk factors (from question 11a to 11e), CRC symptoms (from 12a to 12e), CRCSP organizational issues (from 19a to 19e), CRCSP benefits (from 19f to 19g) and harms (from 19h to 19i) (Annex I, online supplementary material). The potential maximum score of being informed was 10 points and subjects were considered to be informed when scoring 5 or over, with the requirement that at least one correct answer must be obtained in questions related to the CRCSP benefits and harms (from 19f to 19i). Other variables related to information were: access to CRC and CRCSP information (questions 10 and 16 respectively) and general practitioner (GP) information (question 17d).
Explanatory variables are of socio-economic characteristics, relatives and friends with cancer and prevention practices, perceptions, beliefs and attitudes, and information access and KL. The construction of social class variable was made taking into account the abbreviated classification system of the Spanish Society of Epidemiology9 and integrating the concept of dominant social class.10
Data collectionData was collected in 2011. Verbal informed consent was obtained from all participants in the study. The study was approved by the Clinical Research Ethics Committee of the General Directorate of Public Health of VC.
Data analysisA descriptive analysis of the participation in CRCSP and of being informed was performed, using the chi-squared test, in order to identify the independent association with the explanatory variables.
Logistic regression models were adjusted for participation in CRCSP and for being informed, stratifying by sex, including the explanatory variables that showed statically association in the bivariate analysis and those that provided a model with greater prediction.
The results of the chi-squared analysis were shown in terms of p-value, and the logistical regression analysis in terms of odds ratios (OR) and 95% confidence interval (95%CI). The level of significance considered was of 0.05.
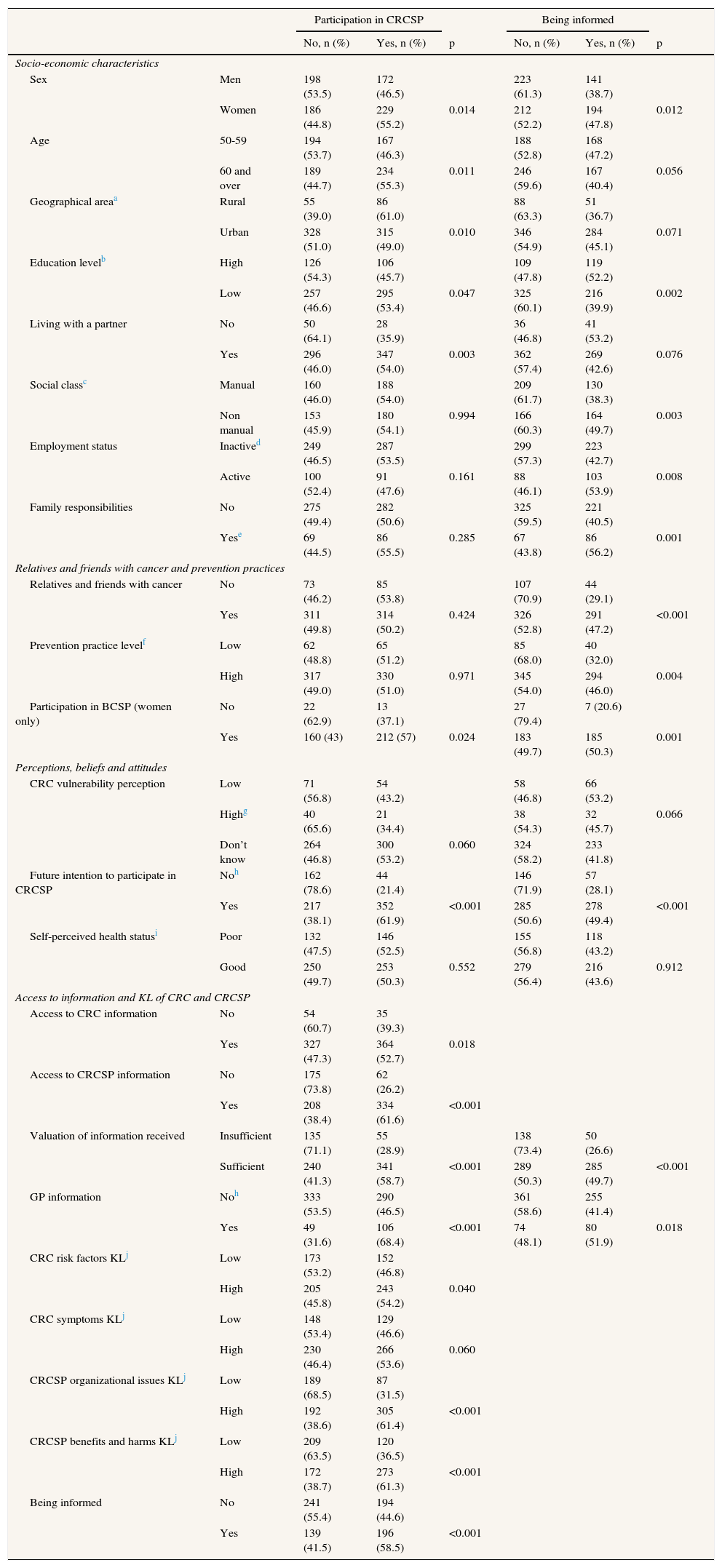
ResultsThe majority of the study subjects were participants in the CRCSP (51.1%, n=401), 55.2% of whom were women (n=229) and 46.5% men (n=172). The majority were uninformed (56.5%, n=435), 52.2% of whom were women (n=212) and 61.3% men (n=223).
Table 1 shows that both participating in CRCSP along with being informed are statistically related (p <0.05). The variables sex, education level, participation in the Breast Cancer Screening Programme (BCSP) (women only), future intention to participate, valuation of the information received and GP information are related both to participation as well as to being informed.
Descriptive and bivariate analysis of the explanatory variables by participation in CRCSP and being informed. Valencian Community, 2009-2010.
| Participation in CRCSP | Being informed | ||||||
|---|---|---|---|---|---|---|---|
| No, n (%) | Yes, n (%) | p | No, n (%) | Yes, n (%) | p | ||
| Socio-economic characteristics | |||||||
| Sex | Men | 198 (53.5) | 172 (46.5) | 223 (61.3) | 141 (38.7) | ||
| Women | 186 (44.8) | 229 (55.2) | 0.014 | 212 (52.2) | 194 (47.8) | 0.012 | |
| Age | 50-59 | 194 (53.7) | 167 (46.3) | 188 (52.8) | 168 (47.2) | ||
| 60 and over | 189 (44.7) | 234 (55.3) | 0.011 | 246 (59.6) | 167 (40.4) | 0.056 | |
| Geographical areaa | Rural | 55 (39.0) | 86 (61.0) | 88 (63.3) | 51 (36.7) | ||
| Urban | 328 (51.0) | 315 (49.0) | 0.010 | 346 (54.9) | 284 (45.1) | 0.071 | |
| Education levelb | High | 126 (54.3) | 106 (45.7) | 109 (47.8) | 119 (52.2) | ||
| Low | 257 (46.6) | 295 (53.4) | 0.047 | 325 (60.1) | 216 (39.9) | 0.002 | |
| Living with a partner | No | 50 (64.1) | 28 (35.9) | 36 (46.8) | 41 (53.2) | ||
| Yes | 296 (46.0) | 347 (54.0) | 0.003 | 362 (57.4) | 269 (42.6) | 0.076 | |
| Social classc | Manual | 160 (46.0) | 188 (54.0) | 209 (61.7) | 130 (38.3) | ||
| Non manual | 153 (45.9) | 180 (54.1) | 0.994 | 166 (60.3) | 164 (49.7) | 0.003 | |
| Employment status | Inactived | 249 (46.5) | 287 (53.5) | 299 (57.3) | 223 (42.7) | ||
| Active | 100 (52.4) | 91 (47.6) | 0.161 | 88 (46.1) | 103 (53.9) | 0.008 | |
| Family responsibilities | No | 275 (49.4) | 282 (50.6) | 325 (59.5) | 221 (40.5) | ||
| Yese | 69 (44.5) | 86 (55.5) | 0.285 | 67 (43.8) | 86 (56.2) | 0.001 | |
| Relatives and friends with cancer and prevention practices | |||||||
| Relatives and friends with cancer | No | 73 (46.2) | 85 (53.8) | 107 (70.9) | 44 (29.1) | ||
| Yes | 311 (49.8) | 314 (50.2) | 0.424 | 326 (52.8) | 291 (47.2) | <0.001 | |
| Prevention practice levelf | Low | 62 (48.8) | 65 (51.2) | 85 (68.0) | 40 (32.0) | ||
| High | 317 (49.0) | 330 (51.0) | 0.971 | 345 (54.0) | 294 (46.0) | 0.004 | |
| Participation in BCSP (women only) | No | 22 (62.9) | 13 (37.1) | 27 (79.4) | 7 (20.6) | ||
| Yes | 160 (43) | 212 (57) | 0.024 | 183 (49.7) | 185 (50.3) | 0.001 | |
| Perceptions, beliefs and attitudes | |||||||
| CRC vulnerability perception | Low | 71 (56.8) | 54 (43.2) | 58 (46.8) | 66 (53.2) | ||
| Highg | 40 (65.6) | 21 (34.4) | 38 (54.3) | 32 (45.7) | 0.066 | ||
| Don’t know | 264 (46.8) | 300 (53.2) | 0.060 | 324 (58.2) | 233 (41.8) | ||
| Future intention to participate in CRCSP | Noh | 162 (78.6) | 44 (21.4) | 146 (71.9) | 57 (28.1) | ||
| Yes | 217 (38.1) | 352 (61.9) | <0.001 | 285 (50.6) | 278 (49.4) | <0.001 | |
| Self-perceived health statusi | Poor | 132 (47.5) | 146 (52.5) | 155 (56.8) | 118 (43.2) | ||
| Good | 250 (49.7) | 253 (50.3) | 0.552 | 279 (56.4) | 216 (43.6) | 0.912 | |
| Access to information and KL of CRC and CRCSP | |||||||
| Access to CRC information | No | 54 (60.7) | 35 (39.3) | ||||
| Yes | 327 (47.3) | 364 (52.7) | 0.018 | ||||
| Access to CRCSP information | No | 175 (73.8) | 62 (26.2) | ||||
| Yes | 208 (38.4) | 334 (61.6) | <0.001 | ||||
| Valuation of information received | Insufficient | 135 (71.1) | 55 (28.9) | 138 (73.4) | 50 (26.6) | ||
| Sufficient | 240 (41.3) | 341 (58.7) | <0.001 | 289 (50.3) | 285 (49.7) | <0.001 | |
| GP information | Noh | 333 (53.5) | 290 (46.5) | 361 (58.6) | 255 (41.4) | ||
| Yes | 49 (31.6) | 106 (68.4) | <0.001 | 74 (48.1) | 80 (51.9) | 0.018 | |
| CRC risk factors KLj | Low | 173 (53.2) | 152 (46.8) | ||||
| High | 205 (45.8) | 243 (54.2) | 0.040 | ||||
| CRC symptoms KLj | Low | 148 (53.4) | 129 (46.6) | ||||
| High | 230 (46.4) | 266 (53.6) | 0.060 | ||||
| CRCSP organizational issues KLj | Low | 189 (68.5) | 87 (31.5) | ||||
| High | 192 (38.6) | 305 (61.4) | <0.001 | ||||
| CRCSP benefits and harms KLj | Low | 209 (63.5) | 120 (36.5) | ||||
| High | 172 (38.7) | 273 (61.3) | <0.001 | ||||
| Being informed | No | 241 (55.4) | 194 (44.6) | ||||
| Yes | 139 (41.5) | 196 (58.5) | <0.001 | ||||
BCSP: breast cancer screening programme; CRC: colorectal cancer; CRCSP: colorectal cancer screening programme; GP: general practitioner; KL: knowledge level.
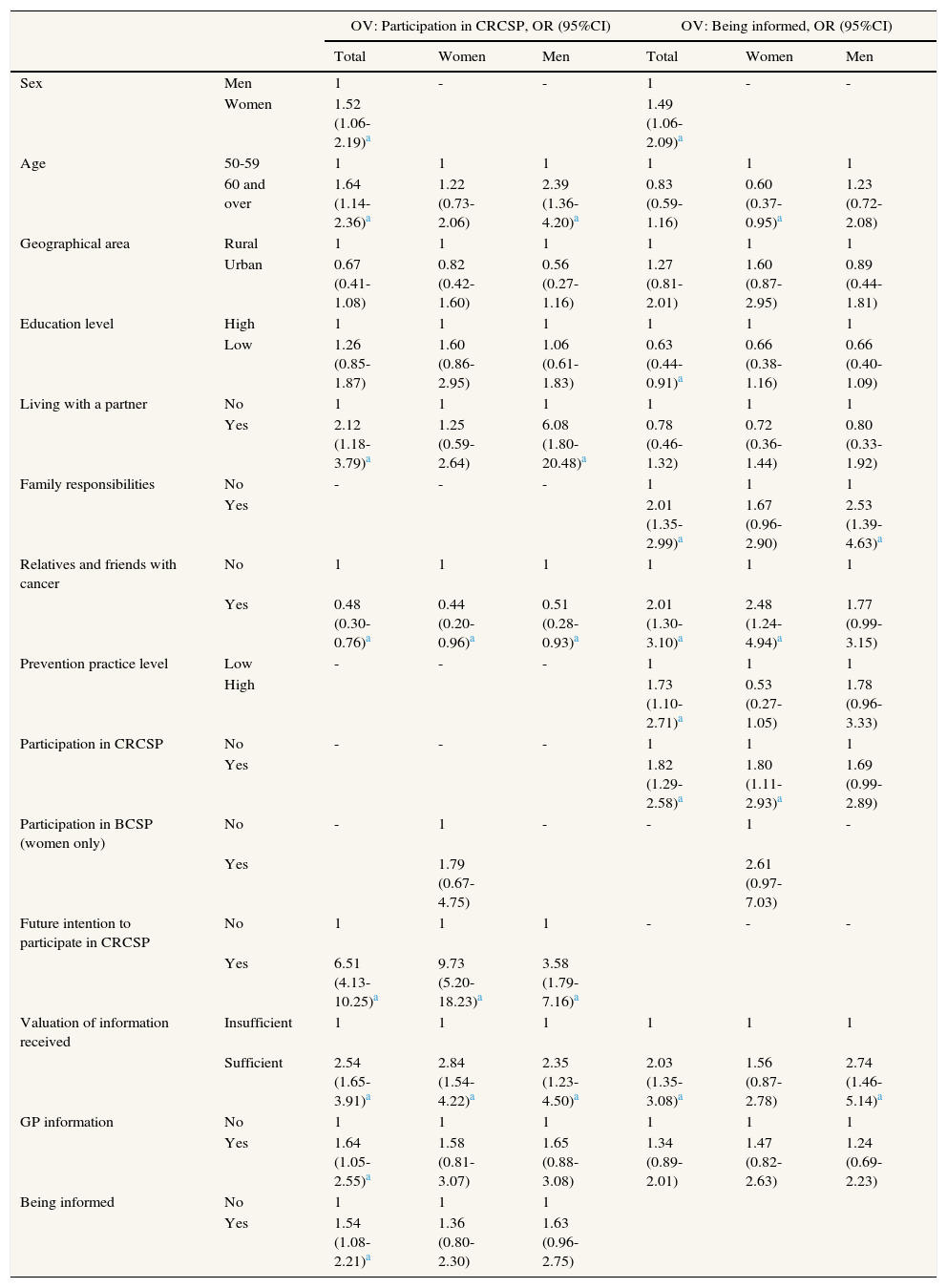
The multivariate analysis (Table 2) shows that there is a greater probability of participation by women (OR: 1.52; 95%CI: 1.06-2.19), being 60 and over (OR: 1.64; 95%CI: 1.14-2.36), living with a partner (OR: 2.12; 95%CI: 1.18-3.79), with future intention to participate in CRCSP (OR: 6.51; 95%CI: 4.13-10.25), considering information to be sufficient (OR: 2.54; 95%CI: 1.65-3.91), receiving GP information (OR:1.64; 95%CI: 1.05-2.55) and being informed (OR: 1.54; 95%CI: 1.08-2.21). Analyses stratified by sex show that men, unlike women, are more likely to take part in screening if they are 60 and over (OR: 2.39; 95%CI: 1.36-4.20) and live with a partner (OR: 6.08; 95%CI: 1.80-20.48). With regards being informed, the probability increases in the case of women (OR: 1.49; 95%CI: 1.06-2.09), people with family responsibilities (OR: 2.01; 95%CI: 1.35-2.99), having relatives and friends with cancer (OR: 2.01; 95%CI: 1.30-3.10), high level of prevention practices (OR: 1.73; 95%CI: 1.10-2.71), had participated in CRCSP (OR: 1.82; 95%CI: 1.29-2.58) and of the opinion that the information conveyed is sufficient (OR: 2.03; 95%CI: 1.35-3.08); and decreased if people have low education level (OR: 0.63; 95%CI: 0.44-0.91). Men, unlike women, are more informed if they have family responsibilities (OR: 2.53; 95%CI: 1.39-4.63) and consider the information conveyed to be sufficient (OR: 2.74; 95%CI: 1.46-5.14).
Multivariate logistic regression models of response variables Participation in CRCSP and Being informed for the total sample and by sex. Valencian Community, 2009-2010.
| OV: Participation in CRCSP, OR (95%CI) | OV: Being informed, OR (95%CI) | ||||||
|---|---|---|---|---|---|---|---|
| Total | Women | Men | Total | Women | Men | ||
| Sex | Men | 1 | - | - | 1 | - | - |
| Women | 1.52 (1.06-2.19)a | 1.49 (1.06-2.09)a | |||||
| Age | 50-59 | 1 | 1 | 1 | 1 | 1 | 1 |
| 60 and over | 1.64 (1.14-2.36)a | 1.22 (0.73-2.06) | 2.39 (1.36-4.20)a | 0.83 (0.59-1.16) | 0.60 (0.37-0.95)a | 1.23 (0.72-2.08) | |
| Geographical area | Rural | 1 | 1 | 1 | 1 | 1 | 1 |
| Urban | 0.67 (0.41-1.08) | 0.82 (0.42-1.60) | 0.56 (0.27-1.16) | 1.27 (0.81-2.01) | 1.60 (0.87-2.95) | 0.89 (0.44-1.81) | |
| Education level | High | 1 | 1 | 1 | 1 | 1 | 1 |
| Low | 1.26 (0.85-1.87) | 1.60 (0.86-2.95) | 1.06 (0.61-1.83) | 0.63 (0.44-0.91)a | 0.66 (0.38-1.16) | 0.66 (0.40-1.09) | |
| Living with a partner | No | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 2.12 (1.18-3.79)a | 1.25 (0.59-2.64) | 6.08 (1.80-20.48)a | 0.78 (0.46-1.32) | 0.72 (0.36-1.44) | 0.80 (0.33-1.92) | |
| Family responsibilities | No | - | - | - | 1 | 1 | 1 |
| Yes | 2.01 (1.35-2.99)a | 1.67 (0.96-2.90) | 2.53 (1.39-4.63)a | ||||
| Relatives and friends with cancer | No | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 0.48 (0.30-0.76)a | 0.44 (0.20-0.96)a | 0.51 (0.28-0.93)a | 2.01 (1.30-3.10)a | 2.48 (1.24-4.94)a | 1.77 (0.99-3.15) | |
| Prevention practice level | Low | - | - | - | 1 | 1 | 1 |
| High | 1.73 (1.10-2.71)a | 0.53 (0.27-1.05) | 1.78 (0.96-3.33) | ||||
| Participation in CRCSP | No | - | - | - | 1 | 1 | 1 |
| Yes | 1.82 (1.29-2.58)a | 1.80 (1.11-2.93)a | 1.69 (0.99-2.89) | ||||
| Participation in BCSP (women only) | No | - | 1 | - | - | 1 | - |
| Yes | 1.79 (0.67-4.75) | 2.61 (0.97-7.03) | |||||
| Future intention to participate in CRCSP | No | 1 | 1 | 1 | - | - | - |
| Yes | 6.51 (4.13-10.25)a | 9.73 (5.20-18.23)a | 3.58 (1.79-7.16)a | ||||
| Valuation of information received | Insufficient | 1 | 1 | 1 | 1 | 1 | 1 |
| Sufficient | 2.54 (1.65-3.91)a | 2.84 (1.54-4.22)a | 2.35 (1.23-4.50)a | 2.03 (1.35-3.08)a | 1.56 (0.87-2.78) | 2.74 (1.46-5.14)a | |
| GP information | No | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 1.64 (1.05-2.55)a | 1.58 (0.81-3.07) | 1.65 (0.88-3.08) | 1.34 (0.89-2.01) | 1.47 (0.82-2.63) | 1.24 (0.69-2.23) | |
| Being informed | No | 1 | 1 | 1 | |||
| Yes | 1.54 (1.08-2.21)a | 1.36 (0.80-2.30) | 1.63 (0.96-2.75) | ||||
BCSP: breast cancer screening programme; 95%CI: 95% confidence interval; CRCSP: colorectal cancer screening programme; GP: general practitioner; OR: odds ratio; OV: outcome variable.
Being a woman, receiving information from a general practitioner and being informed of the disease and the programme are related to participation in CRCSP.
The gender analysis shows that women participate more in CRCSP than men, with similar results in the majority of studies.7,11 Therefore “inverse prevention”12 is taking place in the VC CRCSP, since there is greater incidence and mortality from CRC among men.13 The influence of traditional gender roles in health, such as greater self-care in women and poorer perception of vulnerability among men,14 could be an explanation of these gender inequalities in participation.
This study contributes to improving knowledge about gender differences in the factors related to participation in CRCSP programmes. Men are more likely to participate if they live with a partner, according to the results of other studies that point out the dependence of men on their female partners when carrying out the cancer screening tests.15. And women tend to participate more if they have previously attended BCSP, in line with other studies.16 A positive experience in BCSP and the characteristics of these women may be possible explanations of this relationship. Collaboration between both cancer screening programmes to enhance participation of women and men would be advisable.
The results of this study show a relationship between knowledge about the disease and the programme, and participation in CRCSP. Whereas some studies had not found this relationship17 others had underlined low knowledge as one of the obstacles to participation.18 This relationship should be interpreted with caution as knowledge was measured after participation in the programme and could be conditioned by this. But, in any case, it supports the importance of promoting informed participation. This study also shows that receiving GP information increase participation, highlighting the importance of primary health care involvement in promoting such programmes.19
Finally, the study shows that women, people with high educational level, and having family responsibilities are better informed of CRCSP, with the latter situation statically significant only for men. Gender equity in family care responsibilities could contribute to increasing CRCSP knowledge among men, and therefore to enhancing informed participation in such programmes.
Unbiased information about the CRC and screening programmes involving primary health care professionals, considering specific strategies directed at men and women could enhance informed participation with a gender equity perspective.
Editor in chargeMª José López.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
There is much evidence that men participate less than women in colorectal cancer screening programmes but little is known about if they are also less informed and if this influences their participation. Knowledge of the factors that influence informed participation from a gender perspective is not yet well known and therefore is of the utmost importance.
What does this study add to the literature?Information and participation in colorectal cancer screening programs are interrelated. There are gender inequalities in participation as well as in the access of information, in general showing men to be in an unequal position. Information strategies considering specific actions directed at men and women, could contribute to improving informed participation with a gender equity perspective.
A. Molina-Barceló, R. Peiró-Pérez and D. Salas designed the study. The data was collected by L. Guaita. M. Vanaclocha and G. Vallés performed the analysis of the data. A. Molina-Barceló drafted the manuscript and all the authors contributed to the interpretation of the result, critically revised the work and approved the final version to be published.
FundingThis study has received a grant of 4,950 € from the Regional Health Authorities of the Valencian Community through the call for Grants for the Fomento de la Investigación Sanitaria en la Comunitat Valenciana (Ref. number: 053/2010).
Conflicts of interestNone.