To examine changes in hospital workers’ interventions before and after online training.
MethodPre-post evaluation of the self-reported performance of the 5A's by hospital workers from the three organizations involved. We assessed individual, behavioural, and organisational-level factors through a questionnaire that included 43 items (0 = none to 10 = most possible) completed before and 6 months after the training. Medians and interquartile ranges were calculated. To examine changes, the non-parametric test for paired data (Wilcoxon) was used.
Results202 professionals (76 in Bolivia, 79 in Guatemala, and 47 in Paraguay) finished the course, of these 99 (28, 42, and 29 respectively) completed both questionnaires before and after the training. Overall, there was an increase in the performance of each of the 5A components [Ask (7 to 9): Advise (7 to 9); Assess (6 to 8); Assist (2 to 7); and Arrange a follow up (0.52 to 5); all p <0.001]. Doctors, former smokers, and those from Paraguay obtained higher scores. The level of perception of the participants degree of preparedness, level of competence and familiarity with resources increased (p <0.001).
ConclusionThe online training had a positive impact on the implementation of the brief intervention. Online education on smoking cessation is feasible and effective in improving smoking cessation interventions in these countries.
Examinar los cambios en las intervenciones de los trabajadores antes y después de la formación.
MétodoEvaluación pre-post de la intervención breve autorreportada para dejar de fumar (5A). Se evaluaron factores individuales, de comportamiento y de nivel organizativo mediante un cuestionario de 43 ítems (de 0 = nada a 10 = completamente). Los cuestionarios se completaron antes y 6 meses después de la formación. Se calcularon medianas y rangos intercuartílicos. Para examinar los cambios se utilizó la prueba no paramétrica para datos apareados (Wilcoxon).
Resultados202 profesionales (76 en Bolivia, 79 en Guatemala y 47 en Paraguay) finalizaron el curso; de ellos, 99 (28, 42 y 29, respectivamente) completaron ambos cuestionarios. Hubo un aumento en el desempeño de cada uno de los componentes de las 5A [Averiguar (7,5 a 9); Asesorar (7 a 9); Analizar (6 a 8); Ayudar (2 a 7); y Acordar un seguimiento (0,5 a 5); p <0,001]. Los médicos, los exfumadores y los profesionales de Paraguay obtuvieron puntuaciones más altas. El grado de preparación, el nivel de competencia y la familiaridad con los recursos aumentó entre los participantes (p <0,001).
ConclusiónEl curso tuvo un impacto positivo en la implementación de la intervención breve. La formación online en cesación tabáquica es factible y eficaz en estos países.
Tobacco use remains a global public health concern; annually it causes 6 million preventable deaths.1 The tobacco consumption epidemic is shifting to low- and medium-income countries such as some countries in the Latin American and Caribbean region.2 Currently, more than 120 million smokers live in these countries;3 half of them will develop a tobacco-related disease, and consequently, they will require medical care.4
Smokers are frequent users of health care services, and their contact with the health system might be an ideal teachable moment to encourage quitting.5 Thus, hospitalization provides a unique opportunity to identify and engage smokers, initiate cessation treatments, and facilitate appropriate follow-up and support.6 The brief smoking cessation intervention is recommended by several evidence-based guidelines and has been adopted internationally.7,8 This model known as the “5A's intervention” is based on five stepwise strategies to guide clinicians in how to provide smoking cessation services. It consists of the following actions: 1) Ask patients about smoking at every visit; 2) Advise all tobacco users to quit; 3) Assess smokers’ willingness to try to quit; 4) Assist smokers’ efforts with treatment and referrals; and 5) Arrange follow-up contacts to support cessation efforts.7,8 However, deficiencies persist in implementing the brief smoking cessation interventions in hospital settings.9,10 In particular, smoking cessation services in the Latin American and Caribbean region are scarce4 mainly because the lack of knowledge and skills of health providers, the difficulty to ground tobacco cessation interventions in healthcare organizations, and the lack of working groups and leaders on this topic.11
However, previous works indicate that training healthcare providers could increase in the performance of the 5A's smoking cessation intervention.12–14 In addition, online courses have proven to be more cost-efficient, reinforce counseling skills that often can be difficult to convey in the traditional classroom setting, and allow distance learning when local training opportunities and resources are scarce.15,16 Although previous online tobacco cessation training courses have demonstrated an increase in the health providers’ skills to counsel patients on tobacco cessation17,18 most of them have been developed and evaluated in Anglo-Saxon countries.19
Given the lack of training opportunities in Latin American and Caribbean countries, the Fruitful Study adapted an online smoking cessation training program designed at the Catalan Institute of Oncology (ICO, Barcelona, Spain) to the reality of three Spanish-speaking low and middle income countries (Bolivia, Guatemala, and Paraguay).20 The aim of this study is to examine the changes in health workers’ smoking cessation interventions in Bolivia, Guatemala and Paraguay after the online training and to identify changes in cognitive, behavioral factors and in the perception of organizational support.
MethodsDesignPre-post design was used.
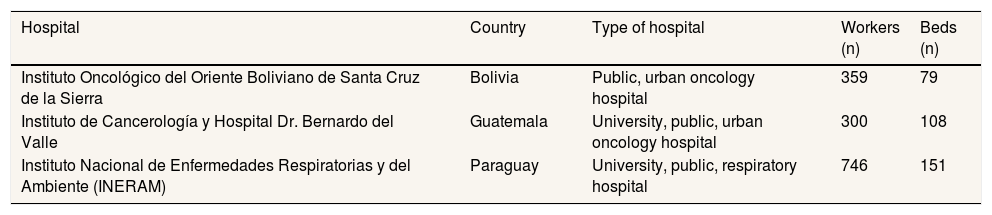
ParticipantsThe participant hospitals were selected at convenience because they had previously collaborated with the Training Unit of the ICO in training their health professionals in either electronic learning (e-learning) or in-person courses. The selected hospitals and their characteristics are shown in Table 1.
Characteristics of the selected hospitals.
| Hospital | Country | Type of hospital | Workers (n) | Beds (n) |
|---|---|---|---|---|
| Instituto Oncológico del Oriente Boliviano de Santa Cruz de la Sierra | Bolivia | Public, urban oncology hospital | 359 | 79 |
| Instituto de Cancerología y Hospital Dr. Bernardo del Valle | Guatemala | University, public, urban oncology hospital | 300 | 108 |
| Instituto Nacional de Enfermedades Respiratorias y del Ambiente (INERAM) | Paraguay | University, public, respiratory hospital | 746 | 151 |
Each local coordinator recruited hospital workers from all units and departments over 6 months (from September 2015 to March 2016) through informative sessions, leaflets and posters (designed to inform about the training program), and personalized emails. Inclusion criteria were being a hospital worker and having an email account.
The online training programThe original training program was developed by the online platform e-oncologia (http://www.e-oncologia.org/en/) based on the in-person courses offered during the last 10 years by the Tobacco Control Unit of the ICO. The Catalan and Spanish version of this course has been taken by almost 1000 workers before its adaptation to the Fruitful study. The final curriculum content of the “Brief Intervention for Smoking Cessation Training Program” is composed of four modules, and it is customized with specific data for each country:
- •
Module 1 describes the tobacco epidemic with specific data for each country.
- •
Module 2 provides orientation on how to assess tobacco dependence.
- •
Module 3 explains in detail the 5A's intervention model.
- •
Module 4 explains the different tobacco cessation treatments available (nicotine replacement, bupropion, varenicline, and other treatments), how to deal with relapses, and so on for each of the countries.
This online training includes: a) slides, b) review exercises, c) practical cases, and d) problem solving exercises. The training provides several materials including slides, online tutorials with an expert tutor, recommended readings, patient cessation brochures, and pharmaceutical pocket guideline, and an organizational recommendation model to facilitate the implementation of tobacco cessation services in the hospital setting. The course has been accredited by the Council of Oncology in Europe (ACOE, www.acoe.be) in support of Continuing Medical Education with 10hours20. The adaptation of the online course was done by local partners and other stakeholders. Extensive information of this process is described elsewhere20, however the main mismatches included: a) language background and literacy level in some of the terms used; b) description of the epidemiology smoking to the reality of Bolivia, Guatemala and Paraguay; c) current tobacco cessation resources in each country; d) simulations and demonstrations were modified to the cultural characteristics of each country; and e) questions and answers of the assessment and evaluation.20
Survey measureAfter registering, hospital workers had access to the baseline survey which was compulsory to complete before accessing into the course. All participants were required to provide an e-mail address to receive an invitation to complete the evaluation survey. Only participants, who finished the training successfully, received an invitation to complete the evaluation survey after 6 months. A maximum of five reminders were sent. Besides, local coordinators personally reminded the need to participate in the post-training evaluation.
The pre- and post-evaluation was a 43-item online questionnaire based on an instrument developed by Sheffer et al.21 to measure cognitive, and some behavioral, factors: 1) motivation, 2) knowledge about tobacco cessation, 3) self-efficacy, 4) importance of providing tobacco use interventions, 5) effectiveness of interventions, 6) importance of barriers, and 7) preparedness.
The survey also assessed the self-reported level of performance according to the 5A'S (Ask, Advise, Assess, Assist, and Arrange follow-up) and included questions about responders’ individual characteristics, including sex, professional group (doctors, registered nurses, nurse assistants, others), tobacco use history, previous tobacco cessation education, and characteristics of their organization (public or private, hospital or other). In addition, we included questions identified previously in the literature and suggested by a panel of experts to explore behavioral factors such as: frequency in seeing tobacco-related diseases, using additional resources to intervene, having previous positive experience, and organizational-level characteristics: having records, systematic protocols, access to tobacco cessation pharmacological aids, among others (Cronbach's α = 0.77).22–24 All 43 items were assessed on a discrete scale of 0-10, with 0 being “none or not at all” and 10 being “the most possible”.
Ethical considerationsAll participants were informed about the main objectives of the study and provided informed consent for their voluntary participation. This study protocol was approved by the Ethics Committee of the Hospital Universitari de Bellvitge (PR338/15).
Statistical analysisBased on literature regarding gains of training,21,22 we anticipated an increase of 40% in health professionals’ level of knowledge, attitudes, and perception in tobacco cessation from baseline to 6 months. Given this estimate, we would need a minimum of 39 participants per hospital (total 117, α = 0.05, β = 0.2, and 10% dropouts).
Descriptive analyses were conducted on the demographic data. Main outcome variables (performance of 5A's and barriers and opportunities of their performance) did not follow normal distribution in all cases, so we conducted medians and interquartile ranges to describe pre- and post-results. Changes in the frequency of the smoking cessation intervention by each component of the 5A's brief intervention in smoking cessation model (Ask, Advise, Assess, Assist, and Arrange) were analyzed using the non-parametric Wilcoxon rank-sum test for paired samples. As, well as changes in cognitive, behavioral and organizational factors, which support or hamper the smoking cessation intervention, which were also tested using the Wilcoxon rank-sum test. The significant level for all the tests was 0.05.
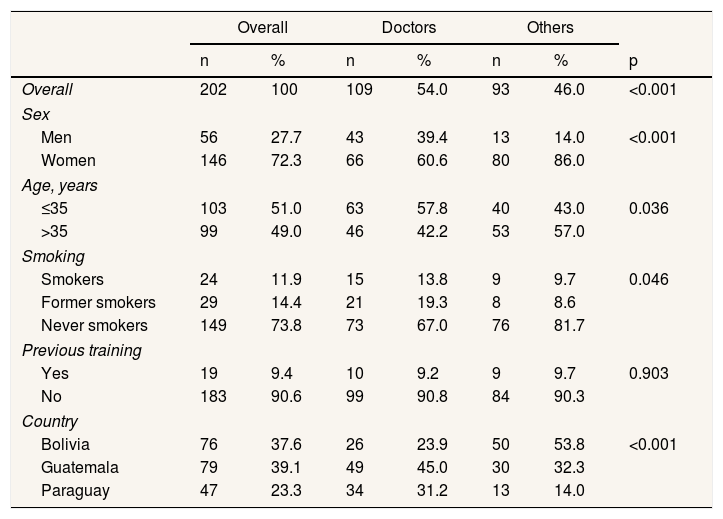
ResultsParticipant characteristicsOverall 202 health workers who finished the course, half of them were doctors (54.0%), and the rest were other health professionals (including nurses, psychologists, and technicians) (Table 2). The majority of them were women (72.3%), equally distributed by age groups (≤35 years old and or >35 years/old). Most reported they had never smoked (73.8%) and 11.9% were current smokers. Overall, 9.4% had previous training in smoking cessation. There were 76 participants in Bolivia, 79 in Guatemala and 47 in Paraguay who finished the training. We observed differences between the profiles of the participants by country: in Guatemala and Paraguay participants were mainly doctors; while in Bolivia other professionals were more prevalent (p <0.001) (Table 2).
Descriptive table of participants according to health working groups (n = 202).
| Overall | Doctors | Others | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p | |
| Overall | 202 | 100 | 109 | 54.0 | 93 | 46.0 | <0.001 |
| Sex | |||||||
| Men | 56 | 27.7 | 43 | 39.4 | 13 | 14.0 | <0.001 |
| Women | 146 | 72.3 | 66 | 60.6 | 80 | 86.0 | |
| Age, years | |||||||
| ≤35 | 103 | 51.0 | 63 | 57.8 | 40 | 43.0 | 0.036 |
| >35 | 99 | 49.0 | 46 | 42.2 | 53 | 57.0 | |
| Smoking | |||||||
| Smokers | 24 | 11.9 | 15 | 13.8 | 9 | 9.7 | 0.046 |
| Former smokers | 29 | 14.4 | 21 | 19.3 | 8 | 8.6 | |
| Never smokers | 149 | 73.8 | 73 | 67.0 | 76 | 81.7 | |
| Previous training | |||||||
| Yes | 19 | 9.4 | 10 | 9.2 | 9 | 9.7 | 0.903 |
| No | 183 | 90.6 | 99 | 90.8 | 84 | 90.3 | |
| Country | |||||||
| Bolivia | 76 | 37.6 | 26 | 23.9 | 50 | 53.8 | <0.001 |
| Guatemala | 79 | 39.1 | 49 | 45.0 | 30 | 32.3 | |
| Paraguay | 47 | 23.3 | 34 | 31.2 | 13 | 14.0 | |
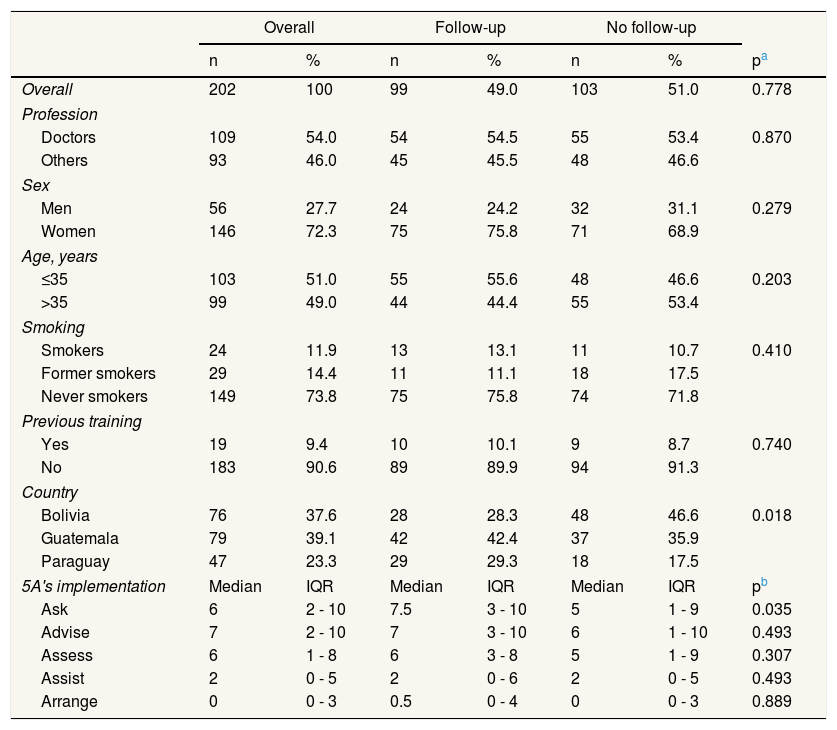
From all the participants, we selected those who completed both pre- and post-evaluation (n = 99). Those that completed the two evaluations were similar to those who did not complete them except for country, thus hospital workers from Bolivia participated less in the pre-post evaluation than those from Guatemala and Paraguay (p = 0.018). In addition, we observed that those who completed the pre- and post- evaluations were more likely to Ask than those who did not completed both evaluations, but performed similarly in the rest of the 5A's model (Table 3).
Descriptive table of participants according to follow-up (n = 202).
| Overall | Follow-up | No follow-up | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | pa | |
| Overall | 202 | 100 | 99 | 49.0 | 103 | 51.0 | 0.778 |
| Profession | |||||||
| Doctors | 109 | 54.0 | 54 | 54.5 | 55 | 53.4 | 0.870 |
| Others | 93 | 46.0 | 45 | 45.5 | 48 | 46.6 | |
| Sex | |||||||
| Men | 56 | 27.7 | 24 | 24.2 | 32 | 31.1 | 0.279 |
| Women | 146 | 72.3 | 75 | 75.8 | 71 | 68.9 | |
| Age, years | |||||||
| ≤35 | 103 | 51.0 | 55 | 55.6 | 48 | 46.6 | 0.203 |
| >35 | 99 | 49.0 | 44 | 44.4 | 55 | 53.4 | |
| Smoking | |||||||
| Smokers | 24 | 11.9 | 13 | 13.1 | 11 | 10.7 | 0.410 |
| Former smokers | 29 | 14.4 | 11 | 11.1 | 18 | 17.5 | |
| Never smokers | 149 | 73.8 | 75 | 75.8 | 74 | 71.8 | |
| Previous training | |||||||
| Yes | 19 | 9.4 | 10 | 10.1 | 9 | 8.7 | 0.740 |
| No | 183 | 90.6 | 89 | 89.9 | 94 | 91.3 | |
| Country | |||||||
| Bolivia | 76 | 37.6 | 28 | 28.3 | 48 | 46.6 | 0.018 |
| Guatemala | 79 | 39.1 | 42 | 42.4 | 37 | 35.9 | |
| Paraguay | 47 | 23.3 | 29 | 29.3 | 18 | 17.5 | |
| 5A's implementation | Median | IQR | Median | IQR | Median | IQR | pb |
| Ask | 6 | 2 - 10 | 7.5 | 3 - 10 | 5 | 1 - 9 | 0.035 |
| Advise | 7 | 2 - 10 | 7 | 3 - 10 | 6 | 1 - 10 | 0.493 |
| Assess | 6 | 1 - 8 | 6 | 3 - 8 | 5 | 1 - 9 | 0.307 |
| Assist | 2 | 0 - 5 | 2 | 0 - 6 | 2 | 0 - 5 | 0.493 |
| Arrange | 0 | 0 - 3 | 0.5 | 0 - 4 | 0 | 0 - 3 | 0.889 |
IQR: interquartile range.
Finally, taking into account the participation level (54.0% were doctors and 46% other health professionals) we decided to perform bivariate analysis between these two groups.
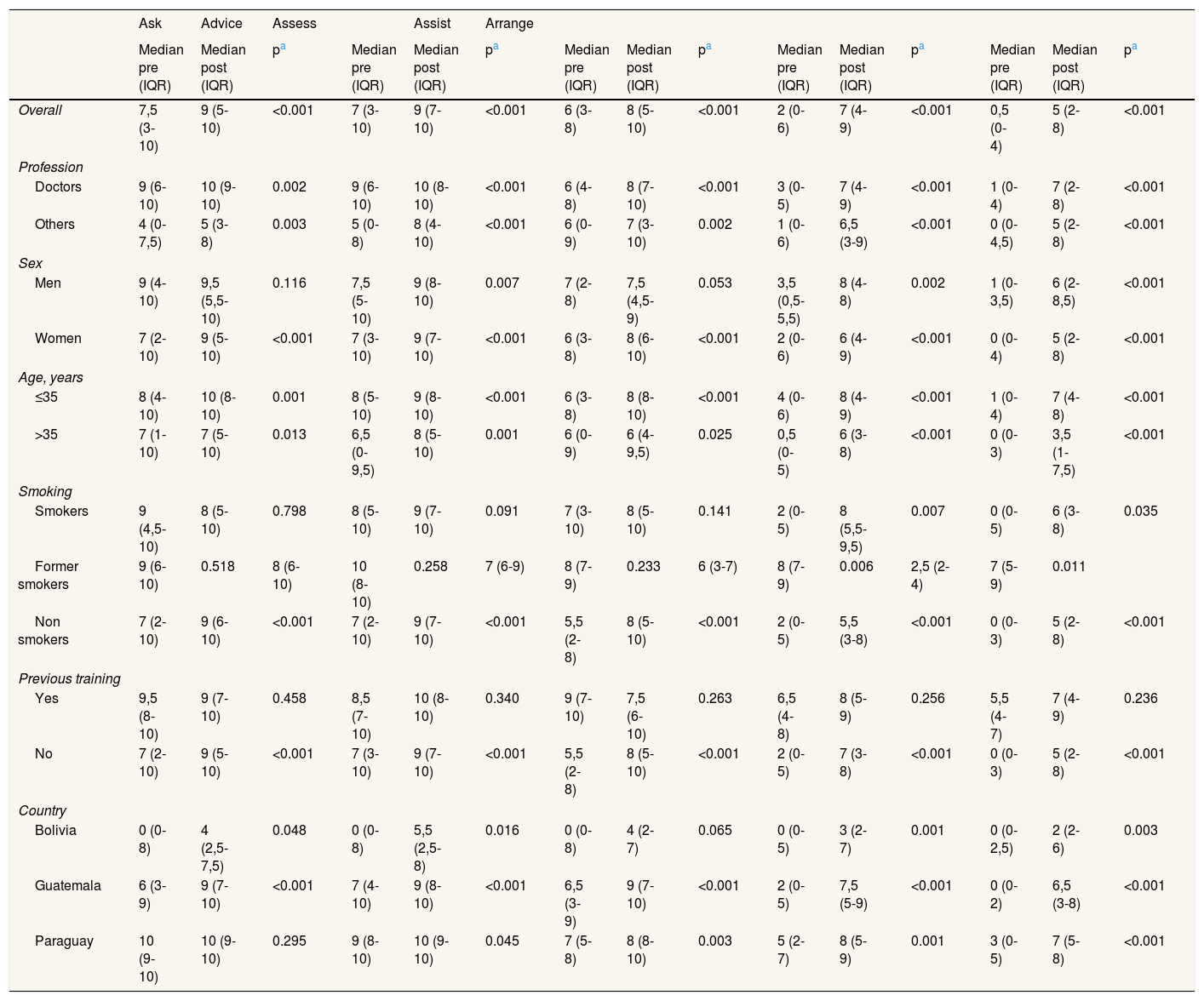
Differences in self-reported performance of the 5A's model before and after the trainingTable 4 displays the self-reported frequency of providing the 5A's smoking cessation intervention to patients before and after the training, overall and by independent variables.
Self-reported performance of the 5A's intervention before and after (6 month) the training (n = 99).
| Ask | Advice | Assess | Assist | Arrange | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median pre (IQR) | Median post (IQR) | pa | Median pre (IQR) | Median post (IQR) | pa | Median pre (IQR) | Median post (IQR) | pa | Median pre (IQR) | Median post (IQR) | pa | Median pre (IQR) | Median post (IQR) | pa | |
| Overall | 7,5 (3-10) | 9 (5-10) | <0.001 | 7 (3-10) | 9 (7-10) | <0.001 | 6 (3-8) | 8 (5-10) | <0.001 | 2 (0-6) | 7 (4-9) | <0.001 | 0,5 (0-4) | 5 (2-8) | <0.001 |
| Profession | |||||||||||||||
| Doctors | 9 (6-10) | 10 (9-10) | 0.002 | 9 (6-10) | 10 (8-10) | <0.001 | 6 (4-8) | 8 (7-10) | <0.001 | 3 (0-5) | 7 (4-9) | <0.001 | 1 (0-4) | 7 (2-8) | <0.001 |
| Others | 4 (0-7,5) | 5 (3-8) | 0.003 | 5 (0-8) | 8 (4-10) | <0.001 | 6 (0-9) | 7 (3-10) | 0.002 | 1 (0-6) | 6,5 (3-9) | <0.001 | 0 (0-4,5) | 5 (2-8) | <0.001 |
| Sex | |||||||||||||||
| Men | 9 (4-10) | 9,5 (5,5-10) | 0.116 | 7,5 (5-10) | 9 (8-10) | 0.007 | 7 (2-8) | 7,5 (4,5-9) | 0.053 | 3,5 (0,5-5,5) | 8 (4-8) | 0.002 | 1 (0-3,5) | 6 (2-8,5) | <0.001 |
| Women | 7 (2-10) | 9 (5-10) | <0.001 | 7 (3-10) | 9 (7-10) | <0.001 | 6 (3-8) | 8 (6-10) | <0.001 | 2 (0-6) | 6 (4-9) | <0.001 | 0 (0-4) | 5 (2-8) | <0.001 |
| Age, years | |||||||||||||||
| ≤35 | 8 (4-10) | 10 (8-10) | 0.001 | 8 (5-10) | 9 (8-10) | <0.001 | 6 (3-8) | 8 (8-10) | <0.001 | 4 (0-6) | 8 (4-9) | <0.001 | 1 (0-4) | 7 (4-8) | <0.001 |
| >35 | 7 (1-10) | 7 (5-10) | 0.013 | 6,5 (0-9,5) | 8 (5-10) | 0.001 | 6 (0-9) | 6 (4-9,5) | 0.025 | 0,5 (0-5) | 6 (3-8) | <0.001 | 0 (0-3) | 3,5 (1-7,5) | <0.001 |
| Smoking | |||||||||||||||
| Smokers | 9 (4,5-10) | 8 (5-10) | 0.798 | 8 (5-10) | 9 (7-10) | 0.091 | 7 (3-10) | 8 (5-10) | 0.141 | 2 (0-5) | 8 (5,5-9,5) | 0.007 | 0 (0-5) | 6 (3-8) | 0.035 |
| Former smokers | 9 (6-10) | 0.518 | 8 (6-10) | 10 (8-10) | 0.258 | 7 (6-9) | 8 (7-9) | 0.233 | 6 (3-7) | 8 (7-9) | 0.006 | 2,5 (2-4) | 7 (5-9) | 0.011 | |
| Non smokers | 7 (2-10) | 9 (6-10) | <0.001 | 7 (2-10) | 9 (7-10) | <0.001 | 5,5 (2-8) | 8 (5-10) | <0.001 | 2 (0-5) | 5,5 (3-8) | <0.001 | 0 (0-3) | 5 (2-8) | <0.001 |
| Previous training | |||||||||||||||
| Yes | 9,5 (8-10) | 9 (7-10) | 0.458 | 8,5 (7-10) | 10 (8-10) | 0.340 | 9 (7-10) | 7,5 (6-10) | 0.263 | 6,5 (4-8) | 8 (5-9) | 0.256 | 5,5 (4-7) | 7 (4-9) | 0.236 |
| No | 7 (2-10) | 9 (5-10) | <0.001 | 7 (3-10) | 9 (7-10) | <0.001 | 5,5 (2-8) | 8 (5-10) | <0.001 | 2 (0-5) | 7 (3-8) | <0.001 | 0 (0-3) | 5 (2-8) | <0.001 |
| Country | |||||||||||||||
| Bolivia | 0 (0-8) | 4 (2,5-7,5) | 0.048 | 0 (0-8) | 5,5 (2,5-8) | 0.016 | 0 (0-8) | 4 (2-7) | 0.065 | 0 (0-5) | 3 (2-7) | 0.001 | 0 (0-2,5) | 2 (2-6) | 0.003 |
| Guatemala | 6 (3-9) | 9 (7-10) | <0.001 | 7 (4-10) | 9 (8-10) | <0.001 | 6,5 (3-9) | 9 (7-10) | <0.001 | 2 (0-5) | 7,5 (5-9) | <0.001 | 0 (0-2) | 6,5 (3-8) | <0.001 |
| Paraguay | 10 (9-10) | 10 (9-10) | 0.295 | 9 (8-10) | 10 (9-10) | 0.045 | 7 (5-8) | 8 (8-10) | 0.003 | 5 (2-7) | 8 (5-9) | 0.001 | 3 (0-5) | 7 (5-8) | <0.001 |
IQR: interquartile range.
Prior to the training the most frequent intervention performed by overall participants was Ask (median score of 7.5 out of 10) and the less frequent Arrange (median score of 0.5 out of 10). Generally, doctors reported higher frequency of performance of the three first components of the 5A's intervention model (Ask, Advise and Assess) than other health professional group (Table 4).
Six months after the training, participants reported higher and statistically significant performance scores in each of the 5A's components of the brief smoking cessation intervention model (p <0.001). The scores of doctors were on all cases higher before and after the training (Table 4). Former smokers obtained higher scores after the training in each of the 5A's components compared to smokers and non-smokers. However, never-smokers were the ones who gained more level of performance after the training compared to baseline (all 5A's components; p <0.001). In addition, those with previous smoking cessation training scored higher after the training but these changes were not statistically significant. Participants without previous training increased the most in the performance of each of the 5A's after the training (p <0.001).
By country, participants from Paraguay scored the highest in each of the 5A's both at the baseline and after the training compared to those from Bolivia and Guatemala. However, the difference in the performance of the 5A's was notorious between Ask, Advise and Assess compared to the scores obtained in Assist and Arrange (Table 4). In spite of this, there was a rise in the performance of all components by country (except for participants from Paraguay who already had high scores in Ask at baseline and the increase was not statistically significant after the training).
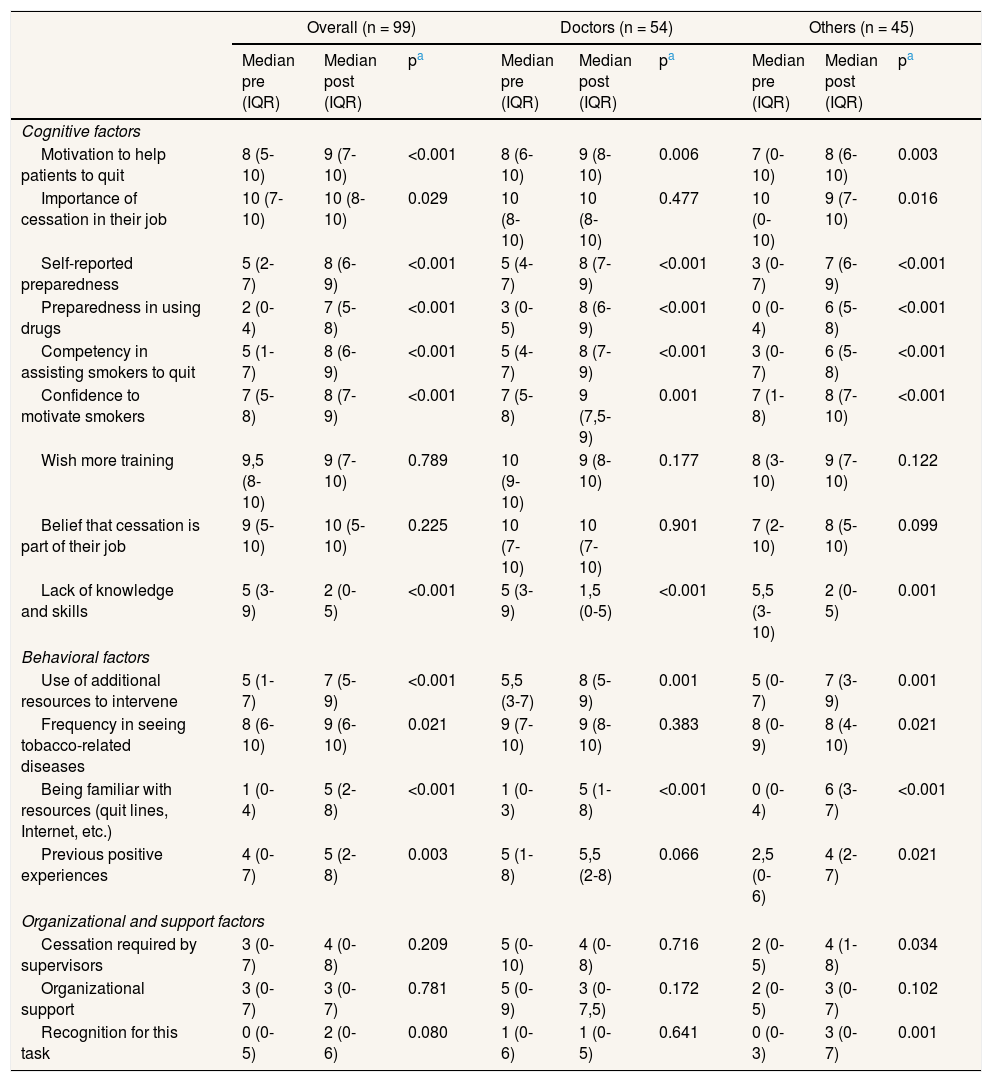
Barriers and opportunities of performing the components of the 5As’ modelTable 5 summarizes some of the cognitive, behavioral and organizational factors that literature report to influence in the performance of the 5A's before and after the training.
Barriers and opportunities in the performance the components of the 5A's model.
| Overall (n = 99) | Doctors (n = 54) | Others (n = 45) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Median pre (IQR) | Median post (IQR) | pa | Median pre (IQR) | Median post (IQR) | pa | Median pre (IQR) | Median post (IQR) | pa | |
| Cognitive factors | |||||||||
| Motivation to help patients to quit | 8 (5-10) | 9 (7-10) | <0.001 | 8 (6-10) | 9 (8-10) | 0.006 | 7 (0-10) | 8 (6-10) | 0.003 |
| Importance of cessation in their job | 10 (7-10) | 10 (8-10) | 0.029 | 10 (8-10) | 10 (8-10) | 0.477 | 10 (0-10) | 9 (7-10) | 0.016 |
| Self-reported preparedness | 5 (2-7) | 8 (6-9) | <0.001 | 5 (4-7) | 8 (7-9) | <0.001 | 3 (0-7) | 7 (6-9) | <0.001 |
| Preparedness in using drugs | 2 (0-4) | 7 (5-8) | <0.001 | 3 (0-5) | 8 (6-9) | <0.001 | 0 (0-4) | 6 (5-8) | <0.001 |
| Competency in assisting smokers to quit | 5 (1-7) | 8 (6-9) | <0.001 | 5 (4-7) | 8 (7-9) | <0.001 | 3 (0-7) | 6 (5-8) | <0.001 |
| Confidence to motivate smokers | 7 (5-8) | 8 (7-9) | <0.001 | 7 (5-8) | 9 (7,5-9) | 0.001 | 7 (1-8) | 8 (7-10) | <0.001 |
| Wish more training | 9,5 (8-10) | 9 (7-10) | 0.789 | 10 (9-10) | 9 (8-10) | 0.177 | 8 (3-10) | 9 (7-10) | 0.122 |
| Belief that cessation is part of their job | 9 (5-10) | 10 (5-10) | 0.225 | 10 (7-10) | 10 (7-10) | 0.901 | 7 (2-10) | 8 (5-10) | 0.099 |
| Lack of knowledge and skills | 5 (3-9) | 2 (0-5) | <0.001 | 5 (3-9) | 1,5 (0-5) | <0.001 | 5,5 (3-10) | 2 (0-5) | 0.001 |
| Behavioral factors | |||||||||
| Use of additional resources to intervene | 5 (1-7) | 7 (5-9) | <0.001 | 5,5 (3-7) | 8 (5-9) | 0.001 | 5 (0-7) | 7 (3-9) | 0.001 |
| Frequency in seeing tobacco-related diseases | 8 (6-10) | 9 (6-10) | 0.021 | 9 (7-10) | 9 (8-10) | 0.383 | 8 (0-9) | 8 (4-10) | 0.021 |
| Being familiar with resources (quit lines, Internet, etc.) | 1 (0-4) | 5 (2-8) | <0.001 | 1 (0-3) | 5 (1-8) | <0.001 | 0 (0-4) | 6 (3-7) | <0.001 |
| Previous positive experiences | 4 (0-7) | 5 (2-8) | 0.003 | 5 (1-8) | 5,5 (2-8) | 0.066 | 2,5 (0-6) | 4 (2-7) | 0.021 |
| Organizational and support factors | |||||||||
| Cessation required by supervisors | 3 (0-7) | 4 (0-8) | 0.209 | 5 (0-10) | 4 (0-8) | 0.716 | 2 (0-5) | 4 (1-8) | 0.034 |
| Organizational support | 3 (0-7) | 3 (0-7) | 0.781 | 5 (0-9) | 3 (0-7,5) | 0.172 | 2 (0-5) | 3 (0-7) | 0.102 |
| Recognition for this task | 0 (0-5) | 2 (0-6) | 0.080 | 1 (0-6) | 1 (0-5) | 0.641 | 0 (0-3) | 3 (0-7) | 0.001 |
IQR: interquartile range.
At baseline, several factors scored ≤5, being identified as barriers. These were self-reported preparedness, preparedness in using drugs, competency in assisting patients, lack of knowledge and skills, use of resources, familiarity with resources, previous positive experiences and the three variables explored for assessing organizational and support factors (Table 5). On the other hand, there were a number of other factors scored over ≥7, identified as opportunities, such as having motivation to help patients to quit, reporting that smoking cessation is important in their job, desiring more training, believing that smoking cessation is part of their job, and seeing patients with tobacco-related diseases.
After the training, five of the identified barriers improved and showed statistically significant changes, all related to cognitive and behavioral factors (p <0.001) (Table 5). Thus, participants reported having gained preparedness, drug preparedness, competency in assisting smokers to quit, using additional resources and having positive experience (p <0.05). However, it was not observed a change in any of the organizational and support factors explored (Table 5).
After the training some factors identified as opportunities (scored ≥7) improved. Hence, participants reported being motivated to quit help patients to quit, thinking that smoking cessation is important for their job and seeing tobacco-related diseases patients more frequently (p <0.001).
By groups, we observed differences among doctors and other professionals (Table 5). The scores were higher among doctors in all the factors explored except for lack of knowledge and organizational and support factors. In addition, only other health professional group expressed a gain in their perception of having more recognition in their task after the training (from 0 to 3; p = 0.001).
DiscussionOur study shows that an online “Brief Intervention for Smoking Cessation Training Program”, which was adapted and offered to hospitals workers from Bolivia, Guatemala and Paraguay improved the performance of all the components of the 5A's model.
Doctors and former smokers presented higher scores in the performance of the 5A's components after the training. The difference in the performance of the 5A's model by professional groups could be consequence of their different education level and responsibilities. Tong et. al25 also identified differences among the seven health professional groups, showing that primary care physicians performed more frequently smoking cessation interventions which is consistent with our results. At the same time, the difference in the effectiveness by country and professional groups should be interpreted taking into account the characteristics of the Fruitful Study (an implementation research project) performed in a low and middle income countries in the Latin American region.20 Furthermore, the scores in Paraguay were higher than in Bolivia and Guatemala, due to the more prevalent presence of doctors in that country (data not shown).
The most recent meta-analysis about the effectiveness of smoking cessation training indicates that health professionals who have received training are more likely to perform positive changes in each of the steps of the 5A's smoking cessation intervention than untrained controls (including: asking patients to set a quit date (p <0.0001); making follow-up appointments (p <0.00001); counselling of smokers (p <0.00001); provision of self-help material (p <0.0001); and prescription of a quit date (p <0.00001), and no evidence of an effect was observed for the provision of nicotine gum/replacement therapy.12 Likewise, online smoking cessation training using the 5A's model has been proved to be effective in other middle income countries such as Czech Republic and China.26,27
In addition, our online training course has demonstrated changes in some identified barriers and opportunities. The main positive changes were observed in the self-reported preparedness, competency and importance of smoking cessation intervention in their job. These findings are in consonance with Applegate et al.13 results, who also demonstrated that training was strongly associated with higher levels of confidence, intervening more often, and reporting fewer barriers to providing cessation services. Some studies have demonstrated a significant relationship between positive attitude and frequent rate of smoking cessation performance.13,14 Reported before, health providers from South American countries may have a high level of resistance to be trained and treat smoking cessation28, this could be a consequence that this service has had little implementation experiences before and there are not many successful precedents. Nevertheless, we observe that in our study while individual factors changed and in some cases improved, organizational factors did not according to health care professionals’ opinion. There are some organizational barriers such as lack of protocols, records, educational materials and, pharmacological aids that might hamper the correct performance of smoking cessation.23,24,29,30 Hence, beyond training these factors may also be incorporated to facilitate the correct implementation of smoking cessation practices.
Tobacco cessation services have been poorly implemented in these countries.4 Online education in tobacco cessation might be the solution to provide evidence-based treatment for tobacco dependence in these countries because it is cost efficient, and can reach remote locations. Most of the existing smoking cessation training programs have been designed in high income countries and are available only in English.19 To our knowledge this is the first study that tests the feasibility and effectiveness of implementing an online smoking cessation training program addressed to health care providers in Bolivia, Guatemala and Paraguay that uses an online platform. Therefore, we can consider that the Fruitful Study approach is groundbreaking for Latin American Region. As proposed in review on Internet-based education, when designing an Internet-based course, this must engage the target group of learners and second “interactivity” is highly valued by leaners32. In our study we learned that doctors were the most interested in enrolling and completing the course. In addition, they obtained higher scores than the rest of health professionals. This could be due to differences between the Internet skills among health professionals in participating countries. In addition, our study offered assistance to students with little or no computer skills. Technical support was mainly used by other professionals and older workers who were less familiar with the use of computers, as previously reported elsewhere.20.
Limitations and strengthsSeveral limitations should be noted for this study. First, this study relies on self-reported responses, and we did not explored patient outcomes as it is suggested by experts in how integrate learning into practice33, that should explored in future research Anyhow in this phase of the FRUIFUL study, we were interested in testing the training course as a tool to gain performance of the 5A's among health care professionals in three Latin American countries. Second, our participants may not be representative of the general profile of the hospital workers in these three countries. Third, only half of our participants completed the pre-post evaluations even though they successfully completed the online course. Despite of the low level of compliance with the two questionnaires, the level of participation is similar to that in previous pre-post training evaluations that have used the Internet (around 50%).27,31 In addition, participants in our course might have a different level of computer skills and Internet usage than non-participants; given that certain computer skills were necessary. Online training programs also require devices for its use −for instance computers, tablets or smart-phones, etc.− and high-speed Internet connection. Internet service and technologic devices are rapidly growing in low-income countries but are not of high quality yet.34 However, this study explores, for the first time in three Latin American Countries, the impact of online smoking cessation training on changing the level of implementation of the 5A's model. Finally, our sample size was small (99 subjects) but enough for pre-post paired comparisons.
ConclusionHospital workers from three low-medium income countries in Latin America reported an increase in all the components of the 5A's smoking cessation model, greater preparedness and competency in assisting smokers, more familiarity with resources after participating in the online program. However, healthcare organizations must facilitate the incorporation of smoking cessation into best practices, facilitating some support and resources. Online training is more feasible in this context and could be a solution to improve a successful implementation of smoking cessation services in low income countries. Future online training programs should have into account that some health professionals could have either little interest or insufficient Internet skills to enroll and complete these courses properly, so some organizations support is required to overcome these barriers.
The tobacco consumption epidemic is shifting to low- and medium-income countries such as some countries in the Latin American Countries. Tobacco cessation training programs are scarce in Spanish speaking low-income countries.
What does this study add to the literature?Hospital workers from participant hospitals in the Fruitful Study reported an increase in all the components of the 5A's smoking cessation model. In addition, hospital workers reported an increase in their level of preparedness and competency in assisting smokers, more familiarity with resources after participating in the online smoking cessation training program. Healthcare organizations must facilitate the incorporation of smoking cessation into best practices, providing managerial support and resources.
Clara Bermúdez-Tamayo.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsDr Martinez and Dr Fernández conceived the project. Dr Martínez coordinated the contents of the program. Dr Martínez and Dr Company co-designed the study, oversaw the training content, and supervise the day to day activities. O Guillen and M Margalef manage the technical support with the online platform. Dr Arrien, Dr Sánchez, J Barnoya and, Dr Cáceres are the project leaders in their hospitals and are responsible for advancing the project activities as scheduled. Y Castellano performed the statistical analysis. The first version of the manuscript was prepared by Dr. Martínez, all the authors contributed to it and approved the final version.
We would like to thank the group of hospital coordinators, Liz Soraya Pérez, Julio Poiqui, Maria del Camen Guzman, Noelia Cañete, Eduardo Gharzouzi,WendyYantuche, and Victor Samayoa, for their assistance in the implementation of this training project.
FundingThis study has been funded by Global Bridges Mayo Clinic (Pfizer Medical Group; GB-13520139: Development and Dissemination of a Tobacco Cessation Training Program for Healthcare Professionals in Spanish-speaking Countries). Moreover, C. Martínez and E. Fernández are also funded by the Spanish Government (Instituto de Salut Carlos III, grant PI15-00875) and the Catalan Government (Xarxa Catalana d’Hospitals sense fum, Agència de Salut Pública de Catalunya, contracte N° 2015VAR171).
Conflicts of interestNone.