To compare the prevalence of chronic headache (CH), chronic neck pain (CNP) and chronic low back pain (CLBP) in the autonomous region of Madrid by analyzing gender differences and to determine the factors associated with each pain location in women in 2007.
MethodsWe analyzed data obtained from adults aged 16 years or older (n = 12,190) who participated in the 2007 Madrid Regional Health Survey. This survey includes data from personal interviews conducted in a representative population residing in family dwellings in Madrid. The presence CH, CNP, and CLBP was analyzed. Sociodemographic features, self-perceived health status, lifestyle habits, psychological distress, drug consumption, use of healthcare services, the search for alternative solutions, and comorbid diseases were analyzed by using logistic regression models.
ResultsThe prevalence of CH, CNP and CLBP was significantly higher (P<0.001) in women (7.3%, 8.4%, 14.1%, respectively) than in men (2.2%, 3.2%, 7.8%, respectively). In women, CH, CNP and CBLP were significantly associated with having ≥3 chronic diseases (OR 7.1, 8.5, 5.8, respectively), and with the use of analgesics and drugs for inflammation (OR: 3.5, 1.95, 2.5, respectively). In the bivariate analysis, the factors associated with pain in distinct body locations differed between men and women.
ConclusionsThis study found that CH, CNP and CLBP are a major public health problem in women in central Spain. Women have a higher overall prevalence of chronic pain than men. Chronic pain was associated with a higher use of analgesics and healthcare services.
Comparar la prevalencia de dolor crónico de cabeza, cervical y lumbar en la Comunidad de Madrid analizando diferencias de sexo, y estudiar factores asociados con la presencia de cada uno de estos dolores en las mujeres.
MétodosSe analizaron los datos de los sujetos de 16 años o más de edad (n = 12,190) que participaron en la Encuesta Regional de Salud de Madrid en el año 2007. La encuesta incluye los datos recogidos de una población representativa de la región de Madrid que vive en su domicilio. Se analizó la presencia de dolor crónico de cabeza (DC), cervical (DCv) y lumbar (DL). Se investigaron características sociodemográficas, percepción de salud, hábitos de vida, estrés psicológico, consumo de fármacos, uso de servicios sanitarios, uso de terapias alternativas y patologías crónicas asociadas mediante análisis multivariado.
ResultadosLa prevalencia de DC, DCv y DL fue significativamente mayor (p <0,001) en las mujeres (7,3%, 8,4%, 14,1%, respectivamente) que en los hombres (2,2%, 3,2%, 7,8%, respectivamente). En las mujeres, el dolor en todas las regiones estuvo asociado con padecer al menos tres afecciones (odds ratio [OR]: 7,1, 8,5, 5,8, respectivamente) y con el uso de analgésicos y antiinflamatorios (OR: 3,5, 1,95, 2,5, respectivamente). El dolor en cada una de las regiones mostró diferentes factores asociados en hombres y en mujeres en el análisis bivariado.
ConclusionesEste estudio encontró que el dolor crónico de cabeza, cervical y lumbar es un problema de salud en las mujeres, ya que presentan mayor prevalencia de dolor que los hombres. El dolor se asocia a un mayor consumo de fármacos y de recursos sanitarios.
Chronic pain (consistent pain for more than 3 months) has a direct impact on quality of life, days off work, and healthcare costs.1 In the United Kingdom, back pain accounted for £1,632 million in direct expenditure and £10,668 million in indirect costs.2 Furthermore, the total cost estimated for the 22 million patients with migraine in the US was 14.4 billion US dollars3 and 27 billion euros for the 41 million patients in Europe.4 Although the most frequent localization is in the low back,5 neck and shoulder pain are also common forms of chronic pain.1,6
A common finding of these studies was that the prevalence of pain was higher in women than in men.6–15 Bingefors and Isacson reported a prevalence of back pain of 24.3% in women and 20.9% in men, and a prevalence of headache of 17.6% in women and 6.7% in men.9In Spain, only a few studies have investigated the prevalence of pain in adults.7,10–15 Indeed, only two studies have analyzed the prevalence of chronic pain.12,15 The first reported a prevalence of back pain (including the neck and low back) of 21.5%.12 The second studied chronic pain in the upper back and neck and found a prevalence of 14.7%.15 Again, the Spanish studies found a higher prevalence of pain in women.7,10–15
The objectives of this study were 1) to estimate and compare the prevalence of chronic headache (CH), chronic neck pain (CNP) and chronic low back pain (CLBP) by sociodemographic variables in women and men living in the autonomous region of Madrid, and 2) to compare differences between women with and without chronic head, neck or low back pain according to self-perceived health status, lifestyle habits, and use of health services or alternative medicine, and to identify which factors are associated with each of the pain locations in women.
MethodsThe 2007 Madrid Regional Health SurveyWe used secondary data provided by the Madrid Regional Health Survey 2007.16 This survey included 12,190 adults (6,448 women, and 5,742 men) and was carried out among non-institutionalized adults (aged 16 years and over) living in the autonomous region of Madrid and was undertaken by the Health and Consumers’ Department of this region. The population in this area was approximately 6 million in 2007.17 The Madrid Regional Health Survey includes individuals residing in main family dwellings (households) selected by probabilistic multistage sampling of residents and registered people. Information was collected by home-based personal interviews between March 2007 and June 2007. The detailed methodologies are described elsewhere.16
The variables used for this study were created from answers to the questions included in the survey questionnaire. Individuals were classified as having CH, CNP or CLBP if they responded “yes” to the question “Have you suffered from head, neck or low back pain over the previous 12 months?”. One question was used for each pain location. As these variables are related to self-reported data, we asked for medical confirmation of the symptoms, particularly headache.
We analyzed the following sociodemographic characteristics: sex, age, marital status, educational level, and place of birth (Spain/not Spain); self-perceived health; number of chronic diseases; lifestyle habits (smoking, alcohol consumption, and obesity); psychological distress; limitation in mobility; drug consumption, and use of healthcare services and the search for alternative solutions for pain as dependent variables.
Among sociodemographic characteristics, similar age categories to those in a previous study7 were used (16-24 years; 25-44 years; 45-64 years; >65 years); marital status was defined as single, married/cohabiting, widowed, and divorced. Educational level was classified into no studies, primary, secondary and university studies.16
Self-perceived health was assessed with the question “What is your perception of your current health status?”. Participants described their health status as excellent, good, fair, poor, or very poor. This variable was also dichotomized into two categories: good health (excellent/good) or bad health (fair/poor/very poor). In addition, individuals were asked about problems with mobility, for instance, at work or at home.
Among lifestyle habits, smoking differentiated between current smokers and non-smokers. Alcohol consumption was measured using the question “Have you frequently consumed alcoholic drinks in the last 12 months?”. Body mass index (BMI) was calculated from self-reported body weight and height. Individuals with a BMI ≥30 were classified as obese.18
Self-reported chronic diseases diagnosed by a physician included high cholesterol, high blood pressure, diabetes, osteoarthritis, asthma, fibromyalgia, osteoporosis, chronic bronchitis, varicose veins, allergy, insomnia, menopausal symptoms, depression, thyroid disease, and anxiety. The number of chronic diseases was categorized into “no chronic diseases”, “1 or 2”, and “3 or more”. Specific questions related to drug consumption, use of healthcare services and the search for alternative solutions for pain were also included as follows: “Have you consumed any specific medications in the last 2 weeks for pain management?” and “Have you receive any healthcare during the last 2 weeks?”.
Finally, the 12-item General Health Questionnaire (GHQ-12) was used to measure psychological distress. The GHQ-12 consists of 12 items assessing the severity of a mental problem over the past few weeks. The response categories of the GHQ-12 scale were scored according to the method proposed by Goldberg and Williams.19 Scores are obtained from the sum of responses to the 12 questions, with the first two response options scoring 0 and the last two scoring 1 (0-0-1-1). A cut-off of 3 points or higher indicates a risk of psychiatric distress according to the Spanish validation studies and the recommendations of the instrument's author.19,20
Statistical analysisTo analyze the data, we first estimated and compared the prevalence (in percentages with their 95%CI) by the sociodemographic variables of adults classified as having CH, CNP or CLBP according to sex. Secondly, we focused only on women and estimated and compared the prevalence (in percentages with their 95%CI) of the three pain locations according to the study variables. The bivariate association between the variables was assessed using the chi square test. Three multivariate logistic regression models were constructed to determine the variables independently associated with the pain location. We included statistically significant variables in the bivariate analysis, as well as those that were of interest from an epidemiological viewpoint. Variables were eliminated, one at each step, according to their significance in the model (Wald statistic) and considering the model's goodness of fit with regard to the previous step (likelihood ratio test). The effects of interaction among the variables included in the final model were also examined. The results of the logistic models were shown as adjusted odds ratios (OR) with 95%CI.
The analyses were performed using the “svy” (survey command) functions of the STATA program, which allowed us to incorporate the study design and weights in all the statistical calculations. Survey command includes sampling weights, cluster sampling, and stratification of the data to reduce the possibility of error in the analysis. Statistical significance was established at p <0.05. As this analysis was conducted in a de-identified, public-use dataset, no approval from an ethics committee was required according to Spanish legislation.
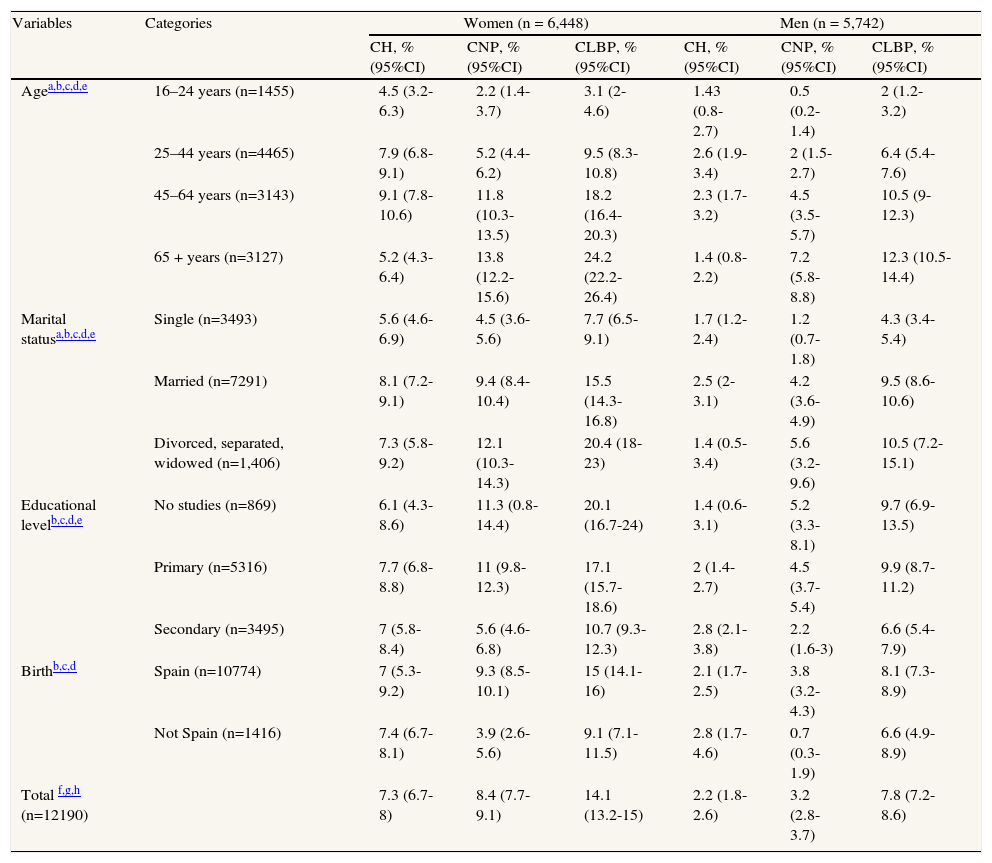
ResultsThe prevalence of CH, CNP and CLBP in women (7.3%, 8.4%, 14.1% respectively) was higher (P <0.001) than in men (2.2%, 3.2%, 7.8% respectively). In all age groups and all sociodemographic variables, the prevalence in women was at least twice as high as that in men (Table 1).
Prevalence of chronic headache (CH), chronic neck pain (CNP) and chronic low back pain (CLBP) among women and men included in the Madrid Regional Health Survey, according to sociodemographic characteristics.
| Variables | Categories | Women (n = 6,448) | Men (n = 5,742) | ||||
| CH, % (95%CI) | CNP, % (95%CI) | CLBP, % (95%CI) | CH, % (95%CI) | CNP, % (95%CI) | CLBP, % (95%CI) | ||
| Agea,b,c,d,e | 16–24 years (n=1455) | 4.5 (3.2-6.3) | 2.2 (1.4-3.7) | 3.1 (2-4.6) | 1.43 (0.8-2.7) | 0.5 (0.2-1.4) | 2 (1.2-3.2) |
| 25–44 years (n=4465) | 7.9 (6.8-9.1) | 5.2 (4.4-6.2) | 9.5 (8.3-10.8) | 2.6 (1.9-3.4) | 2 (1.5-2.7) | 6.4 (5.4-7.6) | |
| 45–64 years (n=3143) | 9.1 (7.8-10.6) | 11.8 (10.3-13.5) | 18.2 (16.4-20.3) | 2.3 (1.7-3.2) | 4.5 (3.5-5.7) | 10.5 (9-12.3) | |
| 65 + years (n=3127) | 5.2 (4.3-6.4) | 13.8 (12.2-15.6) | 24.2 (22.2-26.4) | 1.4 (0.8-2.2) | 7.2 (5.8-8.8) | 12.3 (10.5-14.4) | |
| Marital statusa,b,c,d,e | Single (n=3493) | 5.6 (4.6-6.9) | 4.5 (3.6-5.6) | 7.7 (6.5-9.1) | 1.7 (1.2-2.4) | 1.2 (0.7-1.8) | 4.3 (3.4-5.4) |
| Married (n=7291) | 8.1 (7.2-9.1) | 9.4 (8.4-10.4) | 15.5 (14.3-16.8) | 2.5 (2-3.1) | 4.2 (3.6-4.9) | 9.5 (8.6-10.6) | |
| Divorced, separated, widowed (n=1,406) | 7.3 (5.8-9.2) | 12.1 (10.3-14.3) | 20.4 (18-23) | 1.4 (0.5-3.4) | 5.6 (3.2-9.6) | 10.5 (7.2-15.1) | |
| Educational levelb,c,d,e | No studies (n=869) | 6.1 (4.3-8.6) | 11.3 (0.8-14.4) | 20.1 (16.7-24) | 1.4 (0.6-3.1) | 5.2 (3.3-8.1) | 9.7 (6.9-13.5) |
| Primary (n=5316) | 7.7 (6.8-8.8) | 11 (9.8-12.3) | 17.1 (15.7-18.6) | 2 (1.4-2.7) | 4.5 (3.7-5.4) | 9.9 (8.7-11.2) | |
| Secondary (n=3495) | 7 (5.8-8.4) | 5.6 (4.6-6.8) | 10.7 (9.3-12.3) | 2.8 (2.1-3.8) | 2.2 (1.6-3) | 6.6 (5.4-7.9) | |
| Birthb,c,d | Spain (n=10774) | 7 (5.3-9.2) | 9.3 (8.5-10.1) | 15 (14.1-16) | 2.1 (1.7-2.5) | 3.8 (3.2-4.3) | 8.1 (7.3-8.9) |
| Not Spain (n=1416) | 7.4 (6.7-8.1) | 3.9 (2.6-5.6) | 9.1 (7.1-11.5) | 2.8 (1.7-4.6) | 0.7 (0.3-1.9) | 6.6 (4.9-8.9) | |
| Total f,g,h (n=12190) | 7.3 (6.7-8) | 8.4 (7.7-9.1) | 14.1 (13.2-15) | 2.2 (1.8-2.6) | 3.2 (2.8-3.7) | 7.8 (7.2-8.6) | |
The prevalence of CH among women was highest in the group aged 45-64 years (9.1%); among men, the prevalence was higher in the groups aged 25-44 and 45-64 years (2.6% and 2.3%, respectively). In both sexes, the prevalence of CNP and CLBP was highest among the group aged ≥65 years. In all age groups, the highest prevalence of chronic pain corresponded to CLBP, except in women in the group aged 16-24 years, in whom the prevalence of CH was higher. The least prevalent type of pain was CNP among persons aged 16-44 years of both sexes, and was CH among those aged 45 years or more. Participants who reported their marital status as ‘married’ showed the highest prevalence of CH whereas those who reported being divorced/separated/widowed showed the highest prevalence of CNP and CLBP. Women and men with no studies or only primary studies had more CNP and CLBP. Finally, participants born in Spain reported more CNP, whereas women born outside Spain had more CLBP (Table 1).
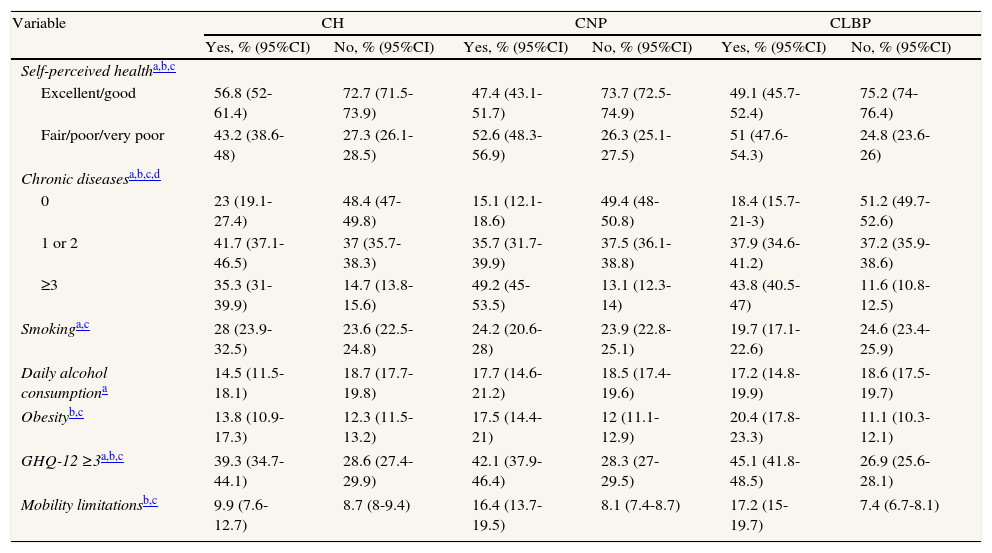
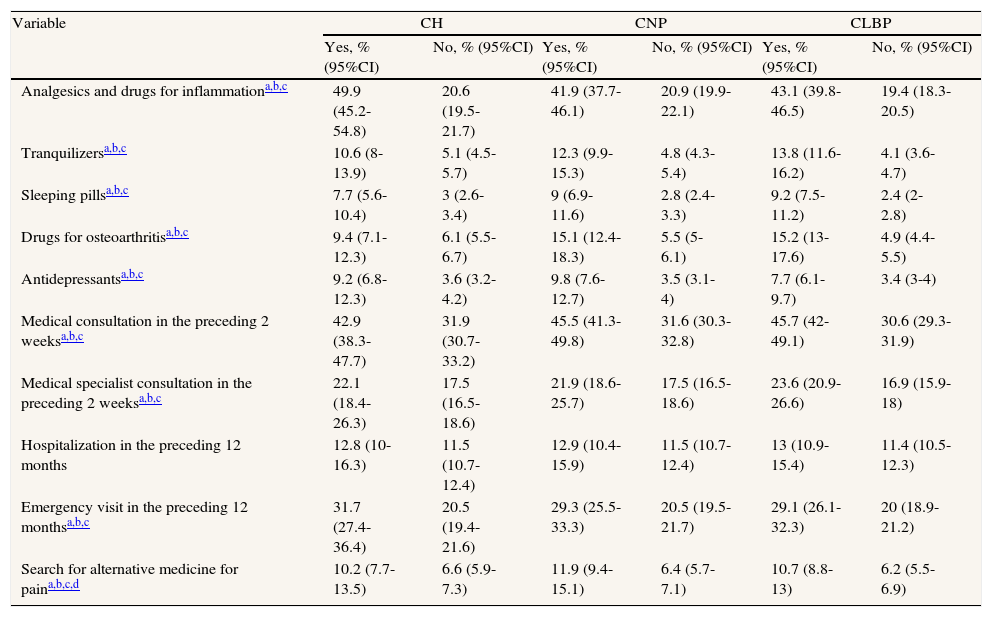
Women with chronic pain of any localization reported poorer self-perceived health than those without pain, showed higher psychological distress, had a greater number of chronic comorbid conditions and used medication and health services more frequently than women with no pain (Tables 2 and 3). Obesity and mobility limitations were associated with the presence of CNP and CLBP. Finally, the prevalence of emergency visits was 10% higher among women with chronic pain than among non-sufferers.
Characteristics of women with and without chronic headache (CH), chronic neck pain (CNP) and chronic low back pain (CLBP) according to self-rated health, comorbidity, lifestyle variables, psychological distress (GHQ-12 ≥3) and mobility limitations.
| Variable | CH | CNP | CLBP | |||
| Yes, % (95%CI) | No, % (95%CI) | Yes, % (95%CI) | No, % (95%CI) | Yes, % (95%CI) | No, % (95%CI) | |
| Self-perceived healtha,b,c | ||||||
| Excellent/good | 56.8 (52-61.4) | 72.7 (71.5-73.9) | 47.4 (43.1-51.7) | 73.7 (72.5-74.9) | 49.1 (45.7-52.4) | 75.2 (74-76.4) |
| Fair/poor/very poor | 43.2 (38.6-48) | 27.3 (26.1-28.5) | 52.6 (48.3-56.9) | 26.3 (25.1-27.5) | 51 (47.6-54.3) | 24.8 (23.6-26) |
| Chronic diseasesa,b,c,d | ||||||
| 0 | 23 (19.1-27.4) | 48.4 (47-49.8) | 15.1 (12.1-18.6) | 49.4 (48-50.8) | 18.4 (15.7-21-3) | 51.2 (49.7-52.6) |
| 1 or 2 | 41.7 (37.1-46.5) | 37 (35.7-38.3) | 35.7 (31.7-39.9) | 37.5 (36.1-38.8) | 37.9 (34.6-41.2) | 37.2 (35.9-38.6) |
| ≥3 | 35.3 (31-39.9) | 14.7 (13.8-15.6) | 49.2 (45-53.5) | 13.1 (12.3-14) | 43.8 (40.5-47) | 11.6 (10.8-12.5) |
| Smokinga,c | 28 (23.9-32.5) | 23.6 (22.5-24.8) | 24.2 (20.6-28) | 23.9 (22.8-25.1) | 19.7 (17.1-22.6) | 24.6 (23.4-25.9) |
| Daily alcohol consumptiona | 14.5 (11.5-18.1) | 18.7 (17.7-19.8) | 17.7 (14.6-21.2) | 18.5 (17.4-19.6) | 17.2 (14.8-19.9) | 18.6 (17.5-19.7) |
| Obesityb,c | 13.8 (10.9-17.3) | 12.3 (11.5-13.2) | 17.5 (14.4-21) | 12 (11.1-12.9) | 20.4 (17.8-23.3) | 11.1 (10.3-12.1) |
| GHQ-12 ≥3a,b,c | 39.3 (34.7-44.1) | 28.6 (27.4-29.9) | 42.1 (37.9-46.4) | 28.3 (27-29.5) | 45.1 (41.8-48.5) | 26.9 (25.6-28.1) |
| Mobility limitationsb,c | 9.9 (7.6-12.7) | 8.7 (8-9.4) | 16.4 (13.7-19.5) | 8.1 (7.4-8.7) | 17.2 (15-19.7) | 7.4 (6.7-8.1) |
95%CI: confidence interval of 95%; GHQ-12: the 12-item General Health Questionnaire.
Characteristics of women with and without chronic headache (CH), chronic neck pain (CNP) and chronic low back pain (CLBP) according drug consumption, health services utilization and other consultations.
| Variable | CH | CNP | CLBP | |||
| Yes, % (95%CI) | No, % (95%CI) | Yes, % (95%CI) | No, % (95%CI) | Yes, % (95%CI) | No, % (95%CI) | |
| Analgesics and drugs for inflammationa,b,c | 49.9 (45.2-54.8) | 20.6 (19.5-21.7) | 41.9 (37.7-46.1) | 20.9 (19.9-22.1) | 43.1 (39.8-46.5) | 19.4 (18.3-20.5) |
| Tranquilizersa,b,c | 10.6 (8-13.9) | 5.1 (4.5-5.7) | 12.3 (9.9-15.3) | 4.8 (4.3-5.4) | 13.8 (11.6-16.2) | 4.1 (3.6-4.7) |
| Sleeping pillsa,b,c | 7.7 (5.6-10.4) | 3 (2.6-3.4) | 9 (6.9-11.6) | 2.8 (2.4-3.3) | 9.2 (7.5-11.2) | 2.4 (2-2.8) |
| Drugs for osteoarthritisa,b,c | 9.4 (7.1-12.3) | 6.1 (5.5-6.7) | 15.1 (12.4-18.3) | 5.5 (5-6.1) | 15.2 (13-17.6) | 4.9 (4.4-5.5) |
| Antidepressantsa,b,c | 9.2 (6.8-12.3) | 3.6 (3.2-4.2) | 9.8 (7.6-12.7) | 3.5 (3.1-4) | 7.7 (6.1-9.7) | 3.4 (3-4) |
| Medical consultation in the preceding 2 weeksa,b,c | 42.9 (38.3-47.7) | 31.9 (30.7-33.2) | 45.5 (41.3-49.8) | 31.6 (30.3-32.8) | 45.7 (42-49.1) | 30.6 (29.3-31.9) |
| Medical specialist consultation in the preceding 2 weeksa,b,c | 22.1 (18.4-26.3) | 17.5 (16.5-18.6) | 21.9 (18.6-25.7) | 17.5 (16.5-18.6) | 23.6 (20.9-26.6) | 16.9 (15.9-18) |
| Hospitalization in the preceding 12 months | 12.8 (10-16.3) | 11.5 (10.7-12.4) | 12.9 (10.4-15.9) | 11.5 (10.7-12.4) | 13 (10.9-15.4) | 11.4 (10.5-12.3) |
| Emergency visit in the preceding 12 monthsa,b,c | 31.7 (27.4-36.4) | 20.5 (19.4-21.6) | 29.3 (25.5-33.3) | 20.5 (19.5-21.7) | 29.1 (26.1-32.3) | 20 (18.9-21.2) |
| Search for alternative medicine for paina,b,c,d | 10.2 (7.7-13.5) | 6.6 (5.9-7.3) | 11.9 (9.4-15.1) | 6.4 (5.7-7.1) | 10.7 (8.8-13) | 6.2 (5.5-6.9) |
95%CI: confidence interval of 95%.
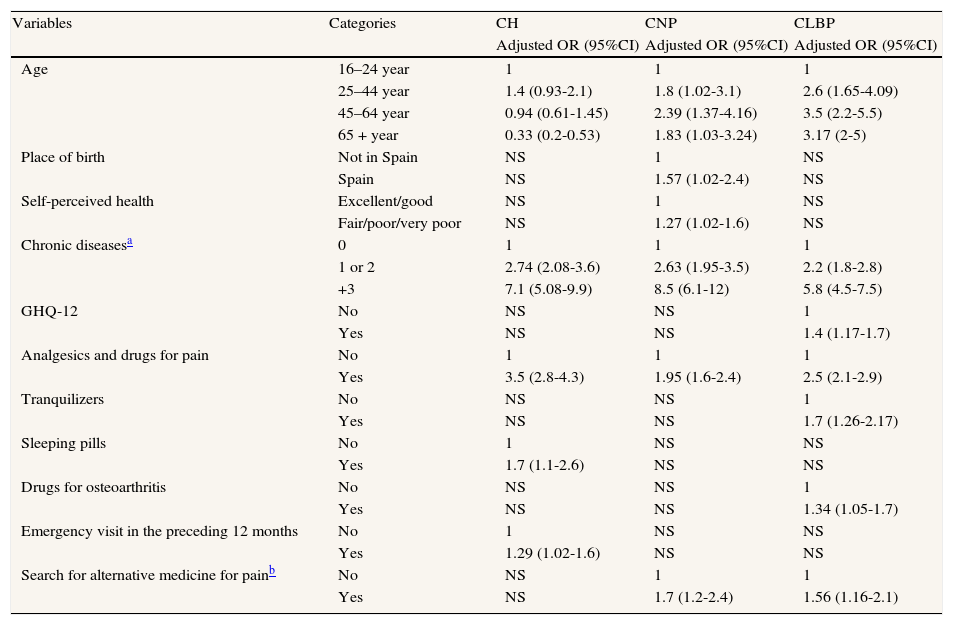
The multivariate analyses showed that CH was less frequent among the oldest age group than among that aged 16-24 years (OR = 0.33; 95%CI: 0.2-0.53). We also found a significant association with having ≥3 chronic diseases when compared with having no conditions (OR = 7.1; 95%CI: 5.08-9.9) and with the use of analgesics and drugs for inflammation (OR = 3.5; 95%CI: 2.8-4.3) (Table 4). Variables significantly associated with CH, but not with either CNP or CLBP, were the use of sleeping pills (OR = 1.7; 95%CI: 1.1-2.6) and emergency visits in the preceding 12 months (OR = 1.29; 95%CI: 1.02-1.6).
Multivariate logistical regression to identify the variables independently associated with chronic headache (CH), chronic neck pain (CNP) and chronic low back pain (CLBP) among women.
| Variables | Categories | CH | CNP | CLBP |
| Adjusted OR (95%CI) | Adjusted OR (95%CI) | Adjusted OR (95%CI) | ||
| Age | 16–24 year | 1 | 1 | 1 |
| 25–44 year | 1.4 (0.93-2.1) | 1.8 (1.02-3.1) | 2.6 (1.65-4.09) | |
| 45–64 year | 0.94 (0.61-1.45) | 2.39 (1.37-4.16) | 3.5 (2.2-5.5) | |
| 65 + year | 0.33 (0.2-0.53) | 1.83 (1.03-3.24) | 3.17 (2-5) | |
| Place of birth | Not in Spain | NS | 1 | NS |
| Spain | NS | 1.57 (1.02-2.4) | NS | |
| Self-perceived health | Excellent/good | NS | 1 | NS |
| Fair/poor/very poor | NS | 1.27 (1.02-1.6) | NS | |
| Chronic diseasesa | 0 | 1 | 1 | 1 |
| 1 or 2 | 2.74 (2.08-3.6) | 2.63 (1.95-3.5) | 2.2 (1.8-2.8) | |
| +3 | 7.1 (5.08-9.9) | 8.5 (6.1-12) | 5.8 (4.5-7.5) | |
| GHQ-12 | No | NS | NS | 1 |
| Yes | NS | NS | 1.4 (1.17-1.7) | |
| Analgesics and drugs for pain | No | 1 | 1 | 1 |
| Yes | 3.5 (2.8-4.3) | 1.95 (1.6-2.4) | 2.5 (2.1-2.9) | |
| Tranquilizers | No | NS | NS | 1 |
| Yes | NS | NS | 1.7 (1.26-2.17) | |
| Sleeping pills | No | 1 | NS | NS |
| Yes | 1.7 (1.1-2.6) | NS | NS | |
| Drugs for osteoarthritis | No | NS | NS | 1 |
| Yes | NS | NS | 1.34 (1.05-1.7) | |
| Emergency visit in the preceding 12 months | No | 1 | NS | NS |
| Yes | 1.29 (1.02-1.6) | NS | NS | |
| Search for alternative medicine for painb | No | NS | 1 | 1 |
| Yes | NS | 1.7 (1.2-2.4) | 1.56 (1.16-2.1) |
OR: odds ratio; 95%CI: confidence interval of 95%; NS = not significant; GHQ-12: the 12-item General Health Questionnaire.
The multivariate analyses showed that CNP was more frequent among the group aged 45-64 years (OR = 2.39; 95%CI: 1.37-4.16) than among that aged 16-24 years. Again, a high association with having ≥ 3 chronic diseases (OR = 8.5; 95%CI: 6.1-12) and with the use of analgesics and drugs for inflammation (OR = 1.95; 95%CI: 1.6-2.4) was found (Table 4). The variables significantly associated with CNP, but not with either CH or CLBP, were birth in Spain (OR = 1.57; 95%CI: 1.02-2.4) and worse self-perceived health (OR = 1.27; 95%CI: 1.02-1.6). Individuals with CNP used homeopathy, osteopathy, acupuncture, chiropractic or naturist products 1.7 times more frequently than those not reporting this pain as alternatives or solutions to pain (OR = 1.7; 95%CI: 1.2-2.4).
Chronic low back painThe multivariate analyses showed that CLBP was more frequent among the groups aged 45-64 and ≥65 years (OR = 3.5, 95%CI: 2.2-5.5; OR = 3.17, 95%CI: 2.0-5.0, respectively) than among the reference age group (16-24 years). We found a significant association between CLBP and having ≥3 chronic diseases (OR = 5.8; 95%CI: 4.5-7.5) and with the use of analgesics and drugs for inflammation (OR = 2.5; 95%CI: 2.1-2.9). Psychological distress (OR = 1.4; 95%CI: 1.17-1.7), the use of tranquilizers (OR = 1.7; 95%CI: 1.26-2.17) and drug consumption for osteoarthritis (OR = 1.34; 95%CI: 1.05-1.7) were significantly associated with CLBP, but not with CH or CNP. Finally, the use of alternatives or solutions to pain was associated with CLBP (OR = 1.56; 95%CI: 1.16-2.1).
DiscussionOur results indicate that CH, CNP and CLBP are a major public health problem in the autonomous region of Madrid. Overall, the most prevalent type of pain was CLBP. Chronic pain was more than twice as common in women than in men. In women, the use of analgesics and drugs for inflammation and having ≥3 chronic diseases was significantly associated with chronic pain. Finally, we found that CH, CNP and CLBP have their own independently associated factors.
The prevalence of CH, CNP and CLBP found in our study was slightly different to that reported by other authors.1,6,12,15,21,22 Previous studies found higher prevalences than the current results. In the Netherlands, Picavet and Schouten found a prevalence of 14.3% of CNP (but without showing the data separately by gender).6 In Spain, previous studies reported prevalences of 21.5%12 and 14.7%15 for both CNP and CLBP together. There are also some studies reporting lower prevalence rates. In North Carolina (US), the prevalence of CNP was 2.2%,21 and that of CLBP was 12.2% in women and 8% in men.22 Differences among studies may be related to different definitions of chronic pain, the recall period used, the study population, data collection, and other factors.
In agreement with previous data, we also found that CLBP was the most common form of pain.5 Our results also agree with previous studies in which women reported a higher prevalence of chronic pain.6–11,13,14
The higher prevalence of chronic pain in women could be explained by several biological differences between women and men. Women have less efficient pain habituation and a greater susceptibility to develop temporal summation of chemically-evoked pain,23 and mechanically-evoked pain,24 as well as less efficient diffuse noxious inhibitory mechanisms25 than men. Other mechanisms are related to estrogen fluctuations and certain genetic relationships in women.26
In addition to biological differences, other possible explanations may include the following: 1) in Spain, women experience higher psychological distress than men, and psychological distress is associated with pain;272) women exhibit a greater number of concomitant chronic diseases,28 which are associated with an increased likelihood of experiencing chronic pain and psychological distress; and 3) unconscious healthcare provider bias may affect healthcare delivery with women being diagnosed less or being treated less effectively or aggressively than men.
With regard to the first point, a recent study conducted in Spain found that women presenting with invalidating musculoskeletal pain had a higher probability (OR = 1.38) of suffering psychological distress than men.27
In a similar population-based study using data from the 2005 Madrid Regional Health Survey, Esteban-Peña et al28 showed that all the chronic diseases included in our study were more prevalent in women than in men: osteoarthritis/arthritis/rheumatism (25.4% vs. 8.9%), allergy (13.5% vs. 10.8%), osteoporosis (8.5% vs. 1%), varicose veins (13.4% vs. 3.4%), and depression (12.4% vs. 5.3%).
Regarding the third point, previous studies have shown that patient and physician gender may impact the process of medical care.29 Physical examinations are less frequently performed in women, which may delay diagnostic tests, thereby increasing the probability of pain becoming chronic in women.30 Nevertheless, it is generally assumed that women have more severe chronic pain and depression than men.30
We found that women with CH, CNP and CLBP consumed more analgesics and drugs for inflammation, especially those with CH. Radat and Lanteri-Minet reported that acute headache medications containing psychoactive components, e.g., barbiturates or opiates, were associated with an increased risk of medication-overuse headache.31 This finding may serve as a possible explanation for the current results, indicating that higher drug consumption may perpetuate chronic pain. Medication overuse in individuals with headache may be related to patients’ dependency on some drugs or to the inefficacy of some drugs, particularly antiinflammatory drugs, in providing pain relief.
As well as the higher consumption of analgesics and drugs for inflammation, we also found an association between CLBP and the use of tranquilizers. In a previous study in Spain, we found similar results: the use of tranquilizers was 1.65 times higher among persons with invalidating musculoskeletal pain. A previous study showed that low back pain was strongly associated with osteoarthritis.14 This finding is expected, since facet joint dysfunction, e.g., due to osteoarthritis, is generally considered as a nociceptive source in low back pain.32 Sleeping pills are associated with CH, which agrees with the results observed by Strine et al,33 who found that headache sufferers were more likely to report insomnia, excessive sleepiness, and depressive or anxiety symptoms.
We found that worse self-perceived health and more visits to the emergency center were associated with CH. A recent review investigating determinant and risk factors for neck pain in the general population supports the association between poor psychological health status and neck pain.34
Finally, the search for alternative medicine for pain relief was also associated with CNP and CLBP. This finding may be related to poor recovery with pharmacological treatment.35 Importantly, musculoskeletal pain is a multidimensional problem in which structure and function interact with personal, environmental and social factors.36 We suggest that, as conventional drug treatment covers one part of the puzzle of chronic pain, patients will usually seek additional help from alternative medicine providers.
The strengths of this study include a large sample size, random selection of the study population and the possibility of analyzing a large number of variables that can often not be obtained from medical records. Information was collected individually, and always from the perspective of citizens, which complements the information that can be obtained from other study sources, e.g., health services, hospital data, etc. However, this study has a number of limitations. Firstly, the questions included in the survey to classify patients as having CH, CNP and CLP included self-reported answers and have not been validated. Nevertheless, this method is commonly used in epidemiological studies.7,13,14,27,28 A strength of the diagnosis is that pain should be diagnosed by a physician. Secondly, information obtained from surveys may be subject to recall errors or to participants’ tendency to provide socially desirable responses. Thirdly, the Madrid Regional Health Survey includes non-institutionalized individuals; therefore, our results cannot be generalized to the institutionalized Spanish population, which may lead to underestimation of the prevalence of pain. Fourthly, the survey did not collect information on pain characteristics, i.e., duration, severity, cause, and working conditions, workload, environment, type of work day, i.e. part-time or full-time, all of which may affect the presence of CH, CNP and CLBP. Finally, since this population-based study has a cross-sectional design, a cause and effect relationship cannot be established. Nevertheless, Picavet and Hazes demonstrated that health surveys are a valuable source of information on musculoskeletal pain problems, which is not available from most other sources of information.37
ConclusionsThis population-based study indicates that CH, CNP, and CLBP are a public health problem in the autonomous region of Madrid, particularly among women. CLBP was the most prevalent pain. Women had a higher overall prevalence than men for chronic pain in all locations. In women, chronic pain was associated with the use of analgesics and drugs for inflammation and with a greater number of comorbid diseases. Clinicians should be aware of these associated conditions to improve the management of women with CH, CNP, and CLBP.
Chronic pain constitutes a public health problem. In the last few years, women have been found to experience chronic pain more frequently than men. Nevertheless, the location of pain may be related to different lifestyle habits or socio-demographic factors.
What does this study contribute to the literature?This is the first epidemiological study conducted in the autonomous region of Madrid that investigates the prevalence of chronic pain. The results confirm that chronic head, neck and low back pain are more prevalent in women than in men, the most frequent localization being low back pain. Chronic pain is associated with analgesic drug consumption and comorbid diseases in women. Identification of the factors associated with chronic pain in distinct locations could be useful in the development of health promotion services.
All authors participated in the study design, data analysis, data interpretation, and drafting and approval of the manuscript submitted for publication.
FundingNone.
Conflicts of interestNone.