To study the level of agreement among health professionals and managers in Catalonia on the benefits of nurse prescribing (NP).
MethodAn online Real Time Delphi was conducted to collect the level of agreement of health professionals and managers. Participants voted in a 6-point scale (1 low benefit and 6 high benefit) for 12 items describing benefits of NP. A total of 1332 professionals participated. The level of consensus was calculated applying interquartile ranges of scores and standardized mean differences among subgroups using effect sizes (ES) and their corresponding 95% confidence intervals.
ResultsThe scores indicate a general agreement on the perceived benefits of NP among participants. Standardized differences among scores on the perceived benefits among professionals were small to high (ES range between 0.2 and 1.2) between nurses and medical doctors and high between nurses and pharmacists (ES range: 1.2 and 2.4). Differences between scores of nurses and those of managers or other professionals in the present study were smaller for most voted benefits.
ConclusionsThe study shows an agreement on the benefits of NP. Nevertheless, when standardized scores are taken into consideration, differences among professionals’ perceptions emerged, and aligned with documented barriers identified in the literature such as corporative aspects, cultural limitations, institutional and organisational inertia, beliefs and unawareness of what NP implies.
Estudiar el nivel de consenso entre profesionales de salud y gestores en Cataluña sobre los beneficios de la prescripción enfermera (PE).
MétodoSe realizó un Delphi en tiempo real en línea para recoger el nivel de acuerdo de profesionales de la salud y gestores. Las personas participantes votaron en una escala de 6 puntos (1 bajo beneficio y 6 alto beneficio) en 12 ítems que describen los beneficios de la PE. Participaron 1332 profesionales. El nivel de consenso se calculó aplicando rangos intercuartílicos de puntuaciones y diferencias de medias estandarizadas entre subgrupos a partir de tamaños del efecto (ES) y sus correspondientes intervalos de confianza del 95%.
ResultadosLas puntuaciones indican un acuerdo general sobre los beneficios percibidos de la PE entre las personas participantes. Las diferencias estandarizadas entre las puntuaciones sobre los beneficios percibidos entre profesionales fueron de pequeñas a altas (rango ES: 0,2 a 1,2) entre enfermeras y médicos, y altas entre enfermeras y farmacéuticos (rango ES: 1,2 a 2,4). Las diferencias entre las puntuaciones de profesionales de enfermería y gestión clínica u otros profesionales en el presente estudio fueron menores para los beneficios más votados.
ConclusionesEl estudio muestra un acuerdo sobre los beneficios de la PE. Sin embargo, cuando se tienen en cuenta las puntuaciones estandarizadas se encontraron algunas diferencias entre las percepciones de profesionales y se alinearon con las barreras documentadas identificadas en la literatura, como aspectos corporativos, limitaciones culturales, inercia institucional y organizativa, creencias y desconocimiento de lo que implica la PE.
In rutinary clinical practice, nurses plan actions to respond to patient's healthcare needs and they implement prescriptions in the majority of cases. These prescriptions (either health interventions, drugs or other healthcare products) help to resolve, improve, stabilise, avoid complications, provide wellbeing or improve patient's health status. In spite of this context, the current legislation does not allow nurses to fully implement in an easy and nominal manner these actions. In the United Kingdom (UK), pharmacists and nurses are authorised to prescribe as non-medical prescribers. In other countries, such as the United States, Australia, Canada, Finland, New Zealand, Norway, Holland or Sweden, including Spain, nurses have the authority to prescribe but with restrictive legal requirements.1 According to a more recent study based on an expert survey and data from the OCDE 2nurses specialists in Ireland, Netherlands and independent nurse prescribers in UK can prescribe most medicines, while they are set to some selected drugs in Cyprus, Denmark, Estonia, Finland, France, Norway, Poland, Spain or Sweden. All countries have regulatory and minimum educational requirements to prescribe and most with medical doctor's supervision.2 It should be noted, that nursing prescription goes beyond medicines and drugs, and apply to any kind of health intervention, medical devise or health product.
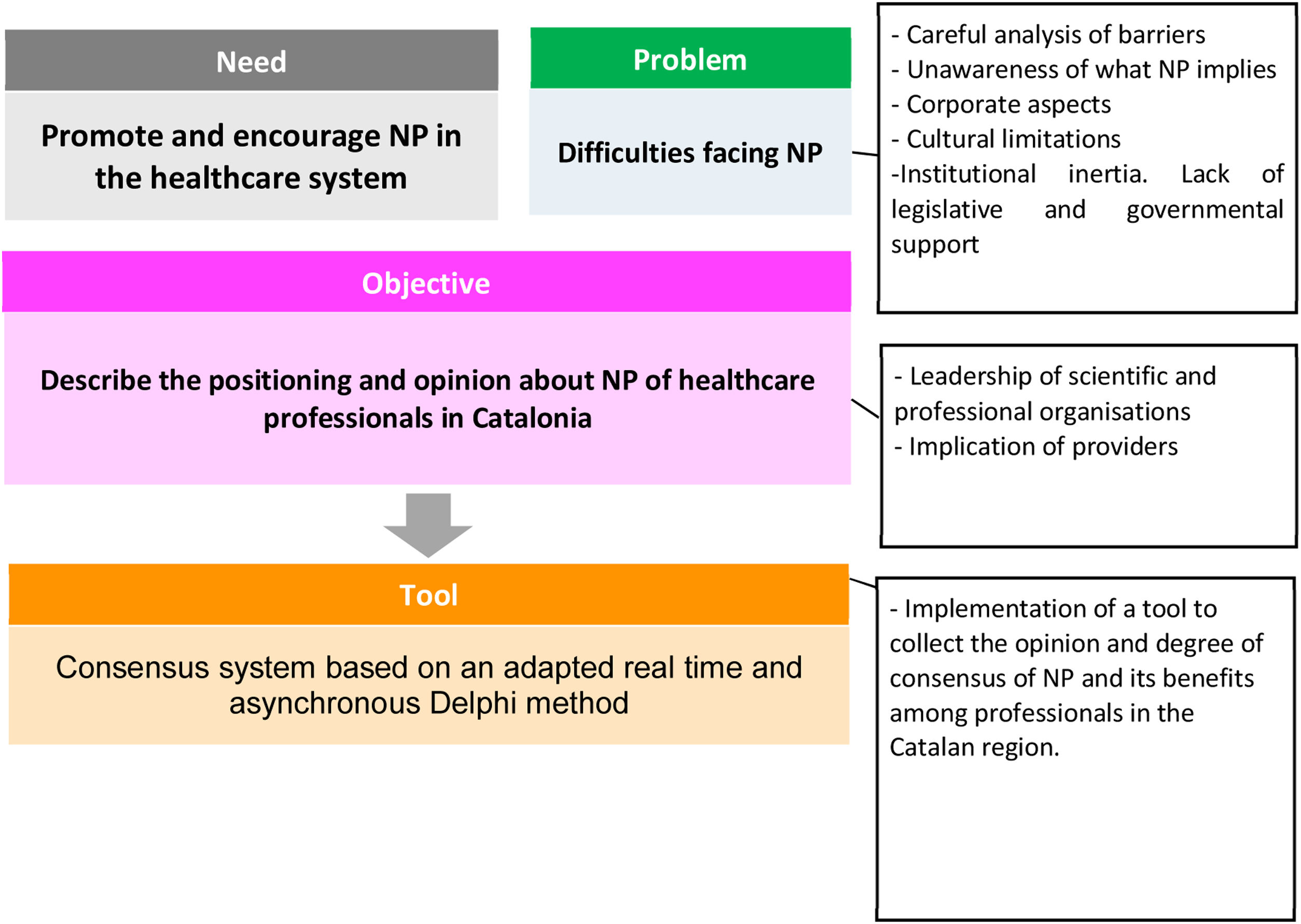
At state level, several publications summarize the evolution of nurse prescription in Spain over the past years and is further summarized in the Online Appendix 1.3–6 Nursing prescription has evolved from an extra-legal framework to an implicit legality, from an explicit illegality to a legal context were a full implementation is still expected.5 In the case of Catalonia, NP is not covered by any specific legal framework. When the Royal Decree 1302/2018 was published on nurse prescribing which regulated the indication, use and authorization of dispensing of medicines and health products for human use by nurses, a positioning paper was made by the Council of Nursing College of Catalonia. The positioning was that it provided greater legal coverage for nurses compared to previous initiatives, even though it was far from establishing a regulation for an effective implementation. In this context, a pilot study gathered the opinion of primary care and community-based health professionals regarding NP and its perceived benefits in a specific health area close to Barcelona in 2015.7,8 In order to further advance in understanding the opinion on the benefits of NP, a wider consensus study was carried out open to health professionals and managers working for the Catalan healthcare system, also as a strategy to generate collective intelligence and knowledge transfer round this topic and is the basis of the present study (Fig. 1).
The general objective of the study was to describe the positioning and level of consensus on the benefits of nursing prescription in Catalonia by nurses and other health professionals.
MethodDesignA Real Time Delphi was conducted, using the Health Consensus platform, widely used in decision-making and for the consensus of new knowledge in the context of health policy.9 A digitally adapted Delphi technique allows participation in areas where there is usually limited available scientific evidence10 enabling processes of knowledge creation.11
Sample/participantsA working group was defined including representatives from key organisations: the Association of Family and Community Nursing of Catalonia (AIFiCC), Official College of Nurses of Barcelona (COIB), Council of Colleges of Nurses of Catalonia, Onsanity, Polytechnic University of Catalonia (UPC) and the Agency of Health Quality and Assessment of Catalonia (AQuAS). In addition, an advisory committee was defined with representatives from the following institutions: Catalan Association of Health (ACES), Catalan Association of Midwives (ACLL), Catalan Association of Welfare Resources (ACRA), Catalan Social and Health Consortium (CSSC), Council of Medical Colleges of Catalonia (CCMC), Catalan Department of Health (DSC), Catalan Health Institute (ICS), Catalan Health Service (SCS), Catalan Hospitals Union (UCH).
The theoretical sample included all professionals working in public and concerted centres in the health system network of Catalonia (SISCAT; promoting mainly the participation of nurses, medical doctors and pharmacists; also managers, professionals from the fields of health planning, and purchase or service evaluation). An open call to participate was made with a direct link to participate in the Health Consensus on NP.
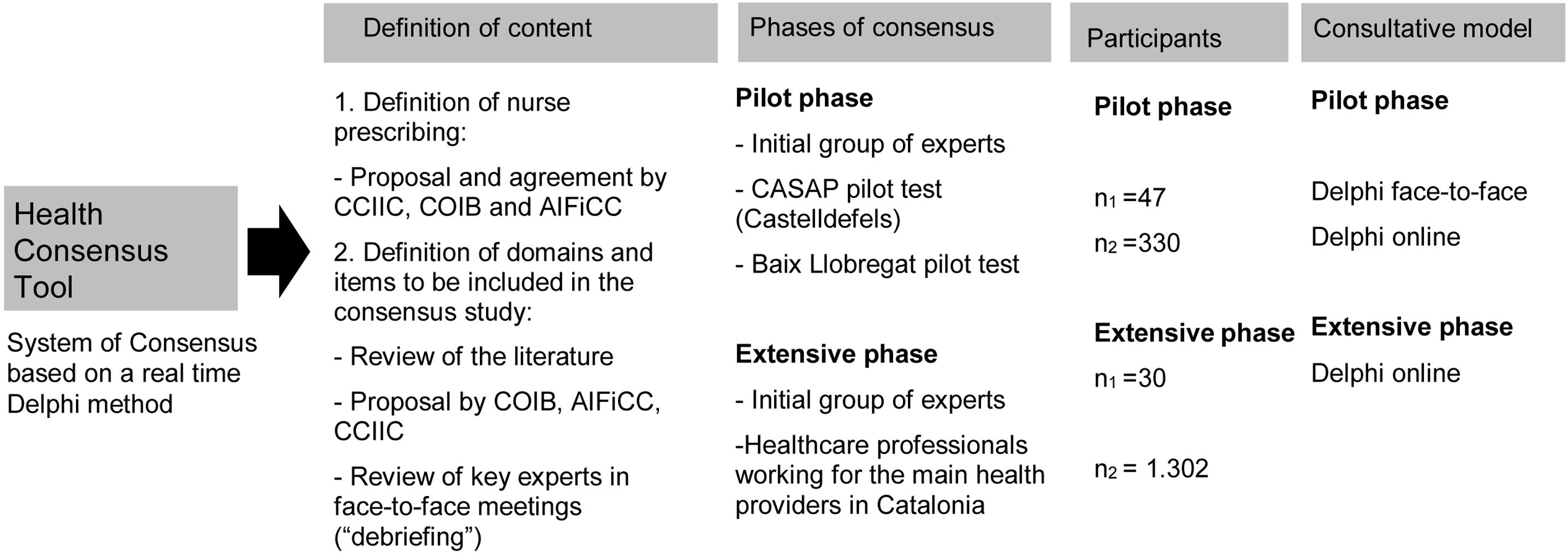
Data collectionIn figure 2, a summary of the phases and steps to develop and implement the contents to be agreed on are presented. The conceptual definition of nurse prescribing (see Online Appendix 2) was proposed by a steering committee and revised by nursing colleges (CCIIC, COIB and AIFiCC). The items reflecting what nurse prescription implies and its benefits were defined based on an ad hoc literature review and debriefing meetings. In a pilot 20 items where tested grouped in 6 domains measuring NP and how it could contribute to improving and benefiting nursing discipline and the healthcare process8: 1) independence, responsibility and job satisfaction, 2) workloads, 3) qualification-competence, 4) relationships among professionals, 5) relationship with patients, and 6) healthcare continuity.
Chart of the consensus process regarding nurse prescribing and its benefits in Catalonia. ACES: Catalan Association of Health; ACLL: Catalan Association of Midwives; ACRA: Catalan Association of Welfare Resources; AIFiCC: Association of Family and Community Nursing of Catalonia; AQuAS: Agency of Health Quality and Assessment of Catalonia; CCIIC: Council of Colleges of Nurses of Catalonia; CCMC: Council of Medical Colleges of Catalonia; COIB: Official College of Nurses of Barcelona, Onsanity; CSSC: Catalan Social and Health Consortium; DS: Department of Health; ICS: Catalan Health Institute; SCS: Catalan Health Service; UCH: Catalan Hospitals Union; UPC: Polytechnic University of Catalonia.
The extensive consensus phase, the basis for the present study, included 12 of 20 items in the pilot phase. After the pilot, an additional debriefing session was implemented to modify and refine them to improve clarity, feasibility and content validity (Fig. 2). The benefits of NP represented through the 12 items were included in an online consensus survey (Tables 1-3) that were supported by publish literature.12–15Figure 2 also shows the phases and rounds of consensus.
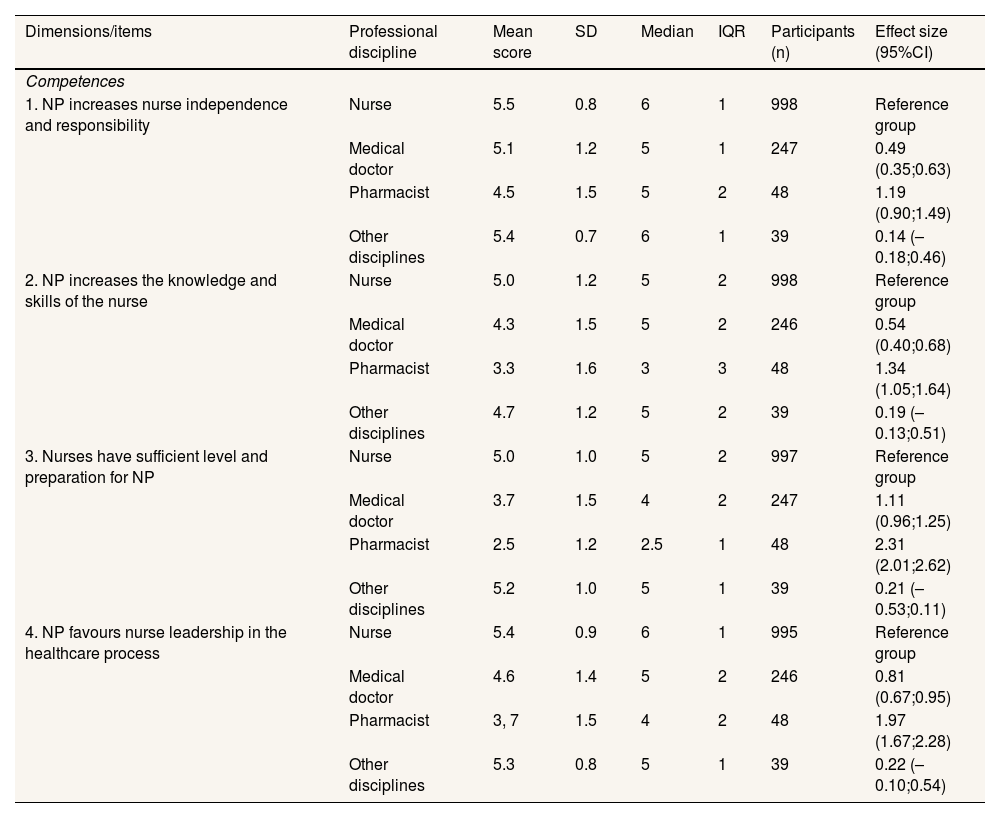
Description of the degree of consensus level on nurse prescribing and its benefits in Catalonia according to professional discipline in statements 1 to 4 (n=1332).
| Dimensions/items | Professional discipline | Mean score | SD | Median | IQR | Participants (n) | Effect size (95%CI) |
|---|---|---|---|---|---|---|---|
| Competences | |||||||
| 1. NP increases nurse independence and responsibility | Nurse | 5.5 | 0.8 | 6 | 1 | 998 | Reference group |
| Medical doctor | 5.1 | 1.2 | 5 | 1 | 247 | 0.49 (0.35;0.63) | |
| Pharmacist | 4.5 | 1.5 | 5 | 2 | 48 | 1.19 (0.90;1.49) | |
| Other disciplines | 5.4 | 0.7 | 6 | 1 | 39 | 0.14 (–0.18;0.46) | |
| 2. NP increases the knowledge and skills of the nurse | Nurse | 5.0 | 1.2 | 5 | 2 | 998 | Reference group |
| Medical doctor | 4.3 | 1.5 | 5 | 2 | 246 | 0.54 (0.40;0.68) | |
| Pharmacist | 3.3 | 1.6 | 3 | 3 | 48 | 1.34 (1.05;1.64) | |
| Other disciplines | 4.7 | 1.2 | 5 | 2 | 39 | 0.19 (–0.13;0.51) | |
| 3. Nurses have sufficient level and preparation for NP | Nurse | 5.0 | 1.0 | 5 | 2 | 997 | Reference group |
| Medical doctor | 3.7 | 1.5 | 4 | 2 | 247 | 1.11 (0.96;1.25) | |
| Pharmacist | 2.5 | 1.2 | 2.5 | 1 | 48 | 2.31 (2.01;2.62) | |
| Other disciplines | 5.2 | 1.0 | 5 | 1 | 39 | 0.21 (–0.53;0.11) | |
| 4. NP favours nurse leadership in the healthcare process | Nurse | 5.4 | 0.9 | 6 | 1 | 995 | Reference group |
| Medical doctor | 4.6 | 1.4 | 5 | 2 | 246 | 0.81 (0.67;0.95) | |
| Pharmacist | 3, 7 | 1.5 | 4 | 2 | 48 | 1.97 (1.67;2.28) | |
| Other disciplines | 5.3 | 0.8 | 5 | 1 | 39 | 0.22 (–0.10;0.54) |
95%CI: 95% confidence interval; IQR: interquartile range; NP: nurse prescribing; SD: standard deviation.
Reference group when comparing the standardised differences of mean scores (for example nurse versus medical doctor/physician, or nurse versus pharmacist).
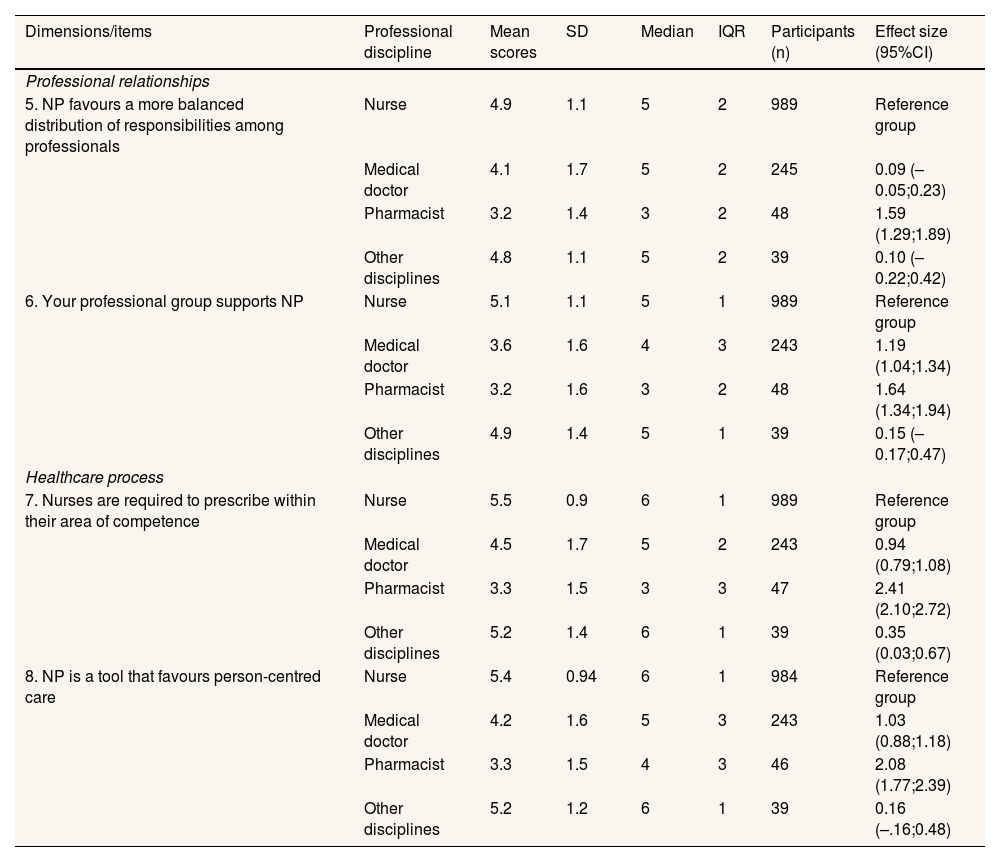
Description of the degree of consensus level on nurse prescribing and its benefits in Catalonia according to professional discipline in statements 5 to 8 (n=1332).
| Dimensions/items | Professional discipline | Mean scores | SD | Median | IQR | Participants (n) | Effect size (95%CI) |
|---|---|---|---|---|---|---|---|
| Professional relationships | |||||||
| 5. NP favours a more balanced distribution of responsibilities among professionals | Nurse | 4.9 | 1.1 | 5 | 2 | 989 | Reference group |
| Medical doctor | 4.1 | 1.7 | 5 | 2 | 245 | 0.09 (–0.05;0.23) | |
| Pharmacist | 3.2 | 1.4 | 3 | 2 | 48 | 1.59 (1.29;1.89) | |
| Other disciplines | 4.8 | 1.1 | 5 | 2 | 39 | 0.10 (–0.22;0.42) | |
| 6. Your professional group supports NP | Nurse | 5.1 | 1.1 | 5 | 1 | 989 | Reference group |
| Medical doctor | 3.6 | 1.6 | 4 | 3 | 243 | 1.19 (1.04;1.34) | |
| Pharmacist | 3.2 | 1.6 | 3 | 2 | 48 | 1.64 (1.34;1.94) | |
| Other disciplines | 4.9 | 1.4 | 5 | 1 | 39 | 0.15 (–0.17;0.47) | |
| Healthcare process | |||||||
| 7. Nurses are required to prescribe within their area of competence | Nurse | 5.5 | 0.9 | 6 | 1 | 989 | Reference group |
| Medical doctor | 4.5 | 1.7 | 5 | 2 | 243 | 0.94 (0.79;1.08) | |
| Pharmacist | 3.3 | 1.5 | 3 | 3 | 47 | 2.41 (2.10;2.72) | |
| Other disciplines | 5.2 | 1.4 | 6 | 1 | 39 | 0.35 (0.03;0.67) | |
| 8. NP is a tool that favours person-centred care | Nurse | 5.4 | 0.94 | 6 | 1 | 984 | Reference group |
| Medical doctor | 4.2 | 1.6 | 5 | 3 | 243 | 1.03 (0.88;1.18) | |
| Pharmacist | 3.3 | 1.5 | 4 | 3 | 46 | 2.08 (1.77;2.39) | |
| Other disciplines | 5.2 | 1.2 | 6 | 1 | 39 | 0.16 (–.16;0.48) |
95%CI: 95% confidence interval; IQR: interquartile range; NP: nurse prescribing; SD: standard deviation.
Reference group when comparing the standardised differences of mean scores (for example nurse versus medical doctor/physician, or nurse versus pharmacist).
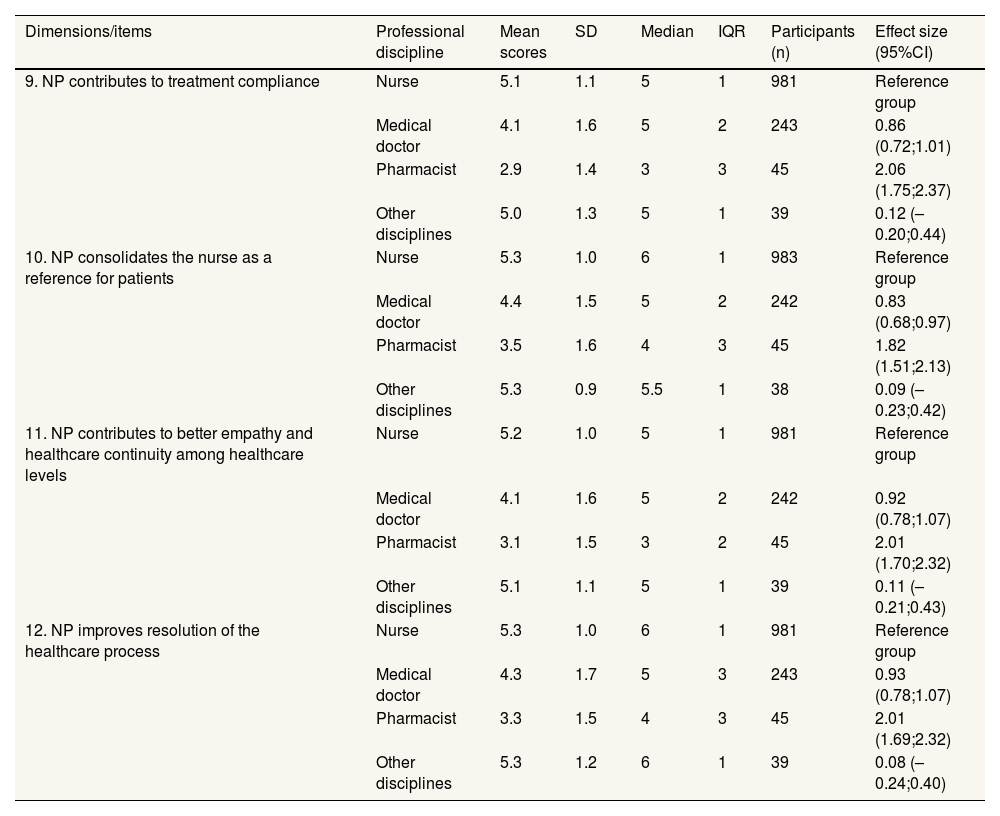
Description of the degree of consensus level on nurse prescribing and its benefits in Catalonia according to professional discipline in statements 9 to 12 (n=1332).
| Dimensions/items | Professional discipline | Mean scores | SD | Median | IQR | Participants (n) | Effect size (95%CI) |
|---|---|---|---|---|---|---|---|
| 9. NP contributes to treatment compliance | Nurse | 5.1 | 1.1 | 5 | 1 | 981 | Reference group |
| Medical doctor | 4.1 | 1.6 | 5 | 2 | 243 | 0.86 (0.72;1.01) | |
| Pharmacist | 2.9 | 1.4 | 3 | 3 | 45 | 2.06 (1.75;2.37) | |
| Other disciplines | 5.0 | 1.3 | 5 | 1 | 39 | 0.12 (–0.20;0.44) | |
| 10. NP consolidates the nurse as a reference for patients | Nurse | 5.3 | 1.0 | 6 | 1 | 983 | Reference group |
| Medical doctor | 4.4 | 1.5 | 5 | 2 | 242 | 0.83 (0.68;0.97) | |
| Pharmacist | 3.5 | 1.6 | 4 | 3 | 45 | 1.82 (1.51;2.13) | |
| Other disciplines | 5.3 | 0.9 | 5.5 | 1 | 38 | 0.09 (–0.23;0.42) | |
| 11. NP contributes to better empathy and healthcare continuity among healthcare levels | Nurse | 5.2 | 1.0 | 5 | 1 | 981 | Reference group |
| Medical doctor | 4.1 | 1.6 | 5 | 2 | 242 | 0.92 (0.78;1.07) | |
| Pharmacist | 3.1 | 1.5 | 3 | 2 | 45 | 2.01 (1.70;2.32) | |
| Other disciplines | 5.1 | 1.1 | 5 | 1 | 39 | 0.11 (–0.21;0.43) | |
| 12. NP improves resolution of the healthcare process | Nurse | 5.3 | 1.0 | 6 | 1 | 981 | Reference group |
| Medical doctor | 4.3 | 1.7 | 5 | 3 | 243 | 0.93 (0.78;1.07) | |
| Pharmacist | 3.3 | 1.5 | 4 | 3 | 45 | 2.01 (1.69;2.32) | |
| Other disciplines | 5.3 | 1.2 | 6 | 1 | 39 | 0.08 (–0.24;0.40) |
95%CI: 95% confidence interval; IQR: interquartile range; NP: nurse prescribing; SD: standard deviation.
Reference group when comparing the standardised differences of mean scores (for example nurse versus medical doctor/physician, or nurse versus pharmacist).
In a first round of consensus, each participant was asked to score individual items (12 items) on a scale from one to six (1 low benefit and 6 high benefit). Once each participant had voted, the Health Consensus platform displayed the mean scores of participants, 50th percentile (P50), standard deviation (SD) and interquartile range (IQR). If considered necessary, they could then change their first vote/positioning (2nd round). The platform was open to participate in the consensus from the end of September and lasted until the end of December 2017 (more details of the process are described elsewhere).
Ethical considerationsThis study followed a strategy to ensure data protection and confidentiality of participants. Participation in the Health consensus was anonymous and a direct link to participate in the platform was sent through institutional websites or providers internal portals. As mentioned before, the call to participate was not nominal (addressed to specific health professionals). This strategy implied participation from scientific societies and health providers/ key institutions/ regional offices first, who then allowed participation of individuals (health professionals) directly through the open link to a survey.
Data analysisDescriptive statistical analysis including the calculation of mean, standard deviation (SD), median (percentile 50; P50), interquartile range (percentile 75-percentile 25, IQR) and percentile 25 (P25) of each of the 12 voted items were applied. These statistics were presented on a global level and stratified by sex, age, professional discipline (nursing, medicine, pharmacy, other), professional profile (healthcare, healthcare and management, management, other) working area (primary and community care, acute care at hospital, mental health, residential care, sexual and reproductive care among other), geographical area where employed, and years of experience.
The level of consensus was described based on IQR statistics. It was established that a value of IQR equal or below 1 implied a high level of consensus, IQR above 1 and below or equal 2 implied a moderate level of consensus, IQR above 2 and equal or below 3 a low level of consensus and finally, an IQR above 3, null or inexistent consensus. To facilitate interpretation of the differences between subgroups regarding their level of consensus (for example between nursing and pharmacy professionals) effect size (ES; standardised difference between mean scores of two subgroups) and their 95% confidence intervals (CI) were calculated. The literature establishes that ES values above 0.8 are considered high differences between scores, ES between 0.5 and 0.8 moderate differences, ES between 0.2 and 0.5 slight differences and ES below 0.2 as no differences between the scores of two subgroups.
ResultsA total of 1332 healthcare professionals and managers participated and voted the 12 items (benefits of NP). Of these, the majority were nurses (74.9%), medical doctors (18.5%) and performed healthcare activities (65.4%). As for the professional field, the majority of participants worked in primary and community-based healthcare (44.4%) or acute hospitals (36.3%) (see Online Appendix 3).
All items measuring the benefits of nurse prescription scored globally a median of 5 to 6 (6 maximum score) by participants (n=1332). Additionally, fifty percent of items reached a high level of consensus on these benefits (data available on request) and the other 50% a moderate level of consensus globally. These results indicate a generalised positioning in favour of NP for professionals participating in the present study.
Effect sizes show moderate to high differences in items (benefits) comparing the standardized differences of nurses with medical doctors scores, as well as nurses with pharmacists scores (Table 1). Differences were null or small for other variables analysed (data not shown and can be obtained on request). Nurses participating in the present study showed a high degree of consensus for the following benefits of NP (median scores between 5 and 6 and IQR between 0 and 1) (Tables 1-3):
- •
Empowers the nursing profession.
- •
Favours leadership of the nurse in the care process.
- •
Necessary among the skills of nurses.
- •
Favours person-centred care.
- •
Contributes to better empathy and healthcare continuity.
- •
Improves other aspects of healthcare quality.
- •
Improves resolution of the healthcare process.
- •
Increases the feeling of support from their collective to become a NP.
Half (50%) of the medical doctors that participated gave a score of five or more (scale of 1 to 6) for almost all the benefits considered for NP in the Health Consensus. Nevertheless, when the scores (votes) for the benefits of NP were stratified and standardised they showed moderate (effect size between 0.6 and 0.8) to high (effect size above 0.8) differences when compared to the nursing collective for almost all the items assessed (Tables 1-3).
Medical doctors had an opinion similar to nurses regarding the following proposed benefits of NP:
- •
Increases independence and responsibility of the nurse.
- •
Favours a more balanced distribution of responsibilities among professionals.
The degree of consensus for the benefits of NP was lower in the pharmacists participating in the study, who valued the advantages of NP far below the perception of nurses (the magnitude of the differences between these two groups was high ES>0.8). Nevertheless, pharmacists showed a moderate degree of consensus (IQR between 1 and 2) and 50% gave a score of five or more (scale from 1 to 6) in relation to the fact that NP increases nurse independence and responsibility. Finally, in the group of “other” professional disciplines, the scores for the 12 items (benefits of NP) seemed to be practically the same as the standardised scores for nursing profiles. The group of “other disciplines” showed a moderate to high degree of consensus regarding the benefits of NP.
DiscussionTo our knowledge, this is one of the widest consensus study on nurse prescription and its benefits in the Spanish National Health System. In general, there was agreement on the benefits of NP by participants. When stratification of scores was made by their discipline, nurses seem to score higher and reach a highest level of agreement in most benefits included in the Delphi study.
The main barriers of nurse prescription documented in the literature are cultural and corporative (values and beliefs that limit the discipline and rule the biomedical care context), institutional (rules, regulations, protocols) and organizational (funding and leadership). A potential barrier could be the unawareness of what prescription implies in real clinical practice and thus, generating a differential positioning on nurse prescription and the level of agreement on its benefits. These barriers have been studied in various systemic reviews of the evidence identified.1,14,16 Additionally, personal skills and attitudes such as confidence or professional leadership are seen as facilitators in the implementation of nurse prescribing. Regarding system barriers, participants in Noblet et al.14 review include the support and facilitation by existing regulatory frameworks, motivation, funding for continuing education, key strategic approaches and health planning. Based on the factors identified, a conceptual framework was proposed to facilitate decision-makers to implement the prescription of non-medical professionals safely.
Graham-Clarke et al.16 concluded that prescription by non-medical professionals (mainly in the field of nursing and pharmacy, as well as physiotherapists) encourages independence, professional satisfaction and supports professional development. Nevertheless, some studies included reported that the prescribing process resulted in additional anxiety and a certain caution among the professionals involved. Regarding perception of knowledge and skills, in a study from the Netherlands,17 from 386 participant nurses in 2006 and 644 in 2012, only 12% of them considered they were not adequately prepared to prescribe medicines. In a study led in the Spanish context, participating nurses perceived they had better knowledge than primary care physicians do on drugs and medical devices based on available guidelines recommendations for the prevention and treatment of pressure ulcers.18 In a similar study,19 nurses considered that they give better advice about disease and its treatment than medical doctors do. It pointed out that a holistic view of their practice and a greater opportunity to involve their patients could be key aspects for these perspectives.17
Apart from the savings factor (efficiency) and improved quality of healthcare, other benefits of prescribing documented are the improved image of the profession, as well as a gain in independence and therefore, less dependence on the primary healthcare physician or other professionals when attending the needs of patients.16 In this context, the field of “nurse prescribing” will be a hot topic in many areas of care in the near future: the replacement of the nurse in acute care20 or in chronic care, such as diabetes.19 An adequate preparation will be required for the expansion of the scope of independent prescribing for nurses.21,22
LimitationsOne of the main limitations when evaluating the benefits of the prescriber being a nurse or other medical professionals is the measure being assessed and the fact that in rutinary clinical practice, few countries have fully implemented NP. The majority of studies identified in the literature are qualitative and based on the opinion of professionals about these benefits. It seems that the studies published report good cohesion of nursing and other non-healthcare professionals in favour of the benefits of NP.
The strategy used to reach participants in the consensus study has proved to be both useful and valid, although caution should be taken when making extrapolation to the positioning and opinion to all health professionals working in Catalonia. The present study included a wide and multidisciplinary call to all health professionals from different care providers of Catalonia. The most motivated professionals were nurses. Even if there was participation of other health professionals profiles there were not as widely represented. This could be due to less interest in this topic, or actually are less involved in nurse prescription, supporting the hypothesis that nurse prescription is happening informally, and formally in some best practice models/ health centres. The study does not seek to draw causal conclusions, but rather to describe the opinion and level of consensus of participants, and thus the approach used is considered valid and reliable.
The fieldwork was carried out during September to December 2017. The COVID pandemic has limited the advances in the present publication. This could be a limitation, as the knowledge and level of consensus may have changed or evolved due to actions at clinical, management and health policy level, Nevertheless, the authors consider the results can add to the remaining debate on a relevant topic to improve quality of healthcare and the efficiency of services. There is still a remaing need to spread knowledge on what nurse prescription implies. In this sense, few advances have been made regarding strategies to implement nurse prescription in real-world clinical practice not only in Catalonia but in other autonomous communities and state level.6 Future studies should collect consensus in other regions in Spain and update those collected in Catalonia together with the view of aligned disciplines such as psychologists, physiotherapists, social workers, and the view of patients and users (citizens).
Final considerations and recommendationsSome specific recommendations to improve the level of consensus of health professionals on nurse prescribing and further steps for its implementation are proposed as followed:
- •
Define actions with the medical and pharmaceutical community together with nurses to spread and transfer information of the skills and knowledge of the nursing profession for prescribing.
- •
Leadership, expertise, communication, support and personal/professional trust are highlighted as key elements to be present in the implementation of nurse prescription.
- •
Define a communication plan that assures the effective deployment of nurse prescription in Catalonia. In this sense, managers at clinical and healthcare level should aid in the implementation and change process to advance in everyday clinical practice.
- •
Promote strategies aimed at periodically evaluating the benefits of multi-professional teams, provider centers and the profession itself, on effective and safe NP, in the same way that is predicable of any health care by health professionals.
To conclude, there is agreement on the benefits of NP in the participants in the present study in Catalonia. When standardized scores are taken into consideration, differences among professional's perceptions emerged (ex. among nurses and pharmacist or medical doctors). These differences could be due to the documented barriers identified in the literature such as corporative aspects, cultural limitations, institutional and organizational inertia, beliefs and unawareness of what NP really implies in real clinical and daily practice. The results can be considered of usefulness as a small contribution to the theoretical and work framework of current nursing care (pre- and post-COVID pandemic) and in our context.
Open data available on the website of the COPI project at AQuAS: https://aquas.gencat.cat/ca/detall/article/prescripcio_infermera.
Benefits of nurse prescribing in the quality and of healthcare has been evidenced.
What does this study add to the literature?This study has facilitated the agreement on nurse prescribing benefits by a wide group of professionals in our context.
What are the implications of the results?Training and clinical pathways would guide in the increasing knowledge of what nurse prescribing is in clinical practice.
Azucena Santillán-García.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsG. Jodar-Solà, A. Brugués-Brugués, V. Serra-Sutton and J.M. Monguet-Fierro contributed to the conceptualisation of the research. G. Jodar-Solà, V. Serra-Sutton and M. Espallargues-Carreras contributed to the funding acquisition and provided the resources to carry out the research. J.M. Monguet-Fierro and A. Trejo-Omeñaca provided the software used in the study. V. Serra-Sutton, A. Trejo-Omeñaca and J.M. Monguet-Fierro were involved in the data curation and its formal analysis. M. Espallargues-Carreras supervised the study. V. Serra-Sutton, G. Jodar-Solà and A. Brugués-Brugués wrote the original draft. All coauthors participated in the proposal and revision of statements included in the consensus. All coauthors contributed to the recruitment of participants/institutions. All coauthors participated on the discussion of results. All coauthors reviewed the original draft and contributed to the final version.
AcknowledgementsThe present project was commissioned to the Agency for Health Quality and Assessment of Catalonia (AQuAS), a public governmental organization and has been co-leaded in close collaboration with COIB, AIFICC, Onsanity and UPC. We would like to acknowledge the support and collaboration of professionals participating in the project, health providers and health regions in Catalonia who have stimulated participation and dissemination of the project. Specifically we would like to thank the following organizations and representative professionals who have been members of the advisory committee of the present project (see Annexed).
FundingThe present study has not received a specific funding. The Agency of Health Quality and Assessment of Catalonia (AQuAS) signed a collaboration agreement with the Council of Nurses and Infermers Colleges of Catalonia (CIIC) and the Family and Community Nursing Association of Catalonia (AIFiCC) to carry out the study. The project was partially financed by AQuAS and the budget of Group 15 of the Spanish scientific network Consorcio Centro de Investigación Biomédica (CIBER) in Epidemiology and Public Health (CIBERESP). The Spanish Biomedical Network- CIBER financed the Health Delphi platform applied in this consensus study. The revision of English grammar was carried out by a native linguist financed by the CCIIC.
Conflicts of interestThe authors express they have no conflict of interest and have completed the conflict of interest declaration proposed by the ICMJE. Nevertheless, we would like to express the following: G. Jodar and A. Brugués represent the Council of Nurses’ Colleges of Catalonia (CCIIC) and the Association of Family and Community Nursing of Catalonia (AIFiCC). AQuAS contributes to fostering independence in the project development process, the analysis of results, discussion and conclusions/recommendations, together with Onsanity and the Universitat Politècnica de Catalunya (UPC). This collaboration has facilitated the implementation of a rigorous and transparent methodology to analyze the position and opinion on nursing prescription in Catalonia. It should be mentioned that to minimize any potential conflict of interest linked to the COPI study; a wide group of professionals representing key entities has been invited to be part of the project's advisory committee. Regarding the academic profiles of the authors: G. Jodar and A. Brugués are nurses and work in the field of clinical management and are managers in primary health care teams; V. Serra-Sutton is a sociologist and health service researcher working at AQuAS, she is also head of the scientific group representing AQuAS at the CIBERESP, and M. Espallargues is a doctor specializing in preventive medicine and public health and is responsible for the scientific and quality area at AQuAS; J.M. Monguet and A. Trejo are industrial engineers, researchers and teachers in innovation at the UPC. In addition, A. Trejo is director of Onsanity Solutions S.L.
The project had the support and collaboration of the following entities making up the advisory group:
- •
Catalan Association of Health Entities (Núria Cobalea).
- •
Catalan Association of Midwives (Cristina Martínez).
- •
Health and Social Consortium of Catalonia (Palmira Borrás).
- •
Department of Health (Guadalupe Figueras).
- •
Catalan Health Institute (Montse Artigas).
- •
Catalan Health Service (Montserrat Bosch).
- •
Catalan Union of Hospitals (Encarna Ramos and Mercè Estrem).
The research team of the project specifically thanks the improvement comments throughout the project (external reviewers and advisory group):
- •
Ana Ríos and Montserrat Artigas (Directorate of Cures, Catalan Institute of Health).
- •
Núria Cuxart (Directorate of Programs, Official College of Nurses of Barcelona).
- •
Lorena Villa (Consorci Castelldefels Health Agents of Primary Care, CASAP).
- •
Ramon Piñol (Sector Director, Health Region of Lleida).
- •
Mercè Estrem (Technical Secretariat of Health Care, La Unió; Association of Health and Social Entities).
- •
Alicia Ávila and Sandra Lomas (General Directorate of Health Professionals, Department of Health).
- •
Ingrid Bullich (Management of Planning and Care Services Portfolio, Catalan Health Service).
- •
Eva M. Melendo (Socio-Health Directorate Plan, General Directorate of Health Planning, Department of Health).