To explore healthcare professionals’ opinions about low-value practices, identify practices of this kind possibly present in the hospital and barriers and facilitators to reduce them. Low-value practices include those with little or no clinical benefit that may harm patients or lead to a waste of resources.
MethodUsing a mixed methodology, we carried out a survey and two focus groups in a tertiary hospital. In the survey, we assessed doctors’ agreement, subjective adherence and perception of usefulness of 134 recommendations to reduce low-value practices from local and international initiatives. We also identified low-value practices possibly present in the hospital. In the focus groups with professionals from surgical and medical fields, using a phenomenological approach, we identified additional low-value practices, barriers and facilitators to reduce them.
Results169 doctors of 25 specialties participated (response rate: 7%-100%). Overall agreement with recommendations, subjective adherence and usefulness were 83%, 90% and 70%, respectively. Low-value practices form 22 recommendations (16%) were considered as possibly present in the hospital. In the focus groups, the professionals identified seven more. Defensive medicine and scepticism due to contradictory evidence were the main barriers. Facilitators included good leadership and coordination between professionals.
ConclusionsHigh agreement with recommendations to reduce low-value practices and high perception of usefulness reflect great awareness of low-value care in the hospital. However, there are several barriers to reduce them. Interventions to reduce low-value practices should foster confidence in decision-making processes between professionals and patients and provide trusted evidence.
Explorar las opiniones de profesionales sanitarios sobre las prácticas de poco valor, identificar aquellas posiblemente presentes en el hospital y las barreras y los facilitadores para reducirlas. Las prácticas de poco valor incluyen aquellas con poco beneficio clínico que pueden perjudicar a los pacientes o desperdiciar recursos.
MétodoUsando una metodología mixta se llevaron a cabo una encuesta y varios grupos focales en un hospital terciario. En la encuesta se evaluó el grado de acuerdo, la adherencia subjetiva y la percepción de utilidad de 134 recomendaciones para reducir las prácticas de poco valor de iniciativas locales e internacionales, y se identificaron aquellas que podrían estar realizándose en el hospital. En dos grupos focales con profesionales de campos médicos y quirúrgicos, utilizando un enfoque fenomenológico, se identificaron prácticas de poco valor adicionales, barreras y facilitadores para reducirlas.
ResultadosEn la encuesta participaron 169 médicos de 25 especialidades (tasa de respuesta: 7-100%). El acuerdo con las recomendaciones, la adherencia subjetiva y la utilidad fueron del 83%, el 90% y el 70%, respectivamente. Se identificaron prácticas de poco valor de 22 recomendaciones (16%) posiblemente presentes en el hospital. En los grupos focales se identificaron siete prácticas de poco valor adicionales; la medicina defensiva y el escepticismo debido a evidencia contradictoria como principales barreras; y un buen liderazgo y la coordinación entre profesionales como facilitadores.
ConclusionesEl alto grado de acuerdo con las recomendaciones para reducir las prácticas de poco valor y la alta percepción de utilidad reflejan una gran concienciación sobre este problema en el hospital. Sin embargo, existen numerosas barreras para eliminarlas. Las intervenciones para reducirlas deberían fomentar la confianza en la toma de decisiones entre profesionales y pacientes, y proporcionar una evidencia confiable.
Low-value practices include doing tests and treatments in contexts with little or no clinical benefit. They are of low-value because: 1) they do more harm than good; or 2) lack proven effectiveness; or 3) are unnecessary because they do not modify clinical decision-making; or 4) are interventions providing little or no benefit in health at high costs.1–4 All interventions of this kind should be avoided, because they threaten patients’ safety and the quality and sustainability of health systems.5–8
Many initiatives worldwide have been established to address low-value practices. Some of the best known are the Choosing Wisely Campaigns, where scientific societies provide recommendations to reduce practices whose necessity should be discussed. These campaigns have taken place in several countries, including the United States of America, Canada, Australia and Italy.9–12 Initiatives in other countries have adopted some of these recommendations and developed several more, for instance, the Spanish initiatives Essencial,13 and Commitment to quality of the Spanish scientific societies.14
Even though proposing recommendations to reduce low-value practices is a big first step, their detection at local settings and understanding health professionals’ views on this problem are crucial in developing effective interventions to reduce them. Several studies have assessed doctors’ perspectives about the concept of low-value care. However, almost all them have taken place in the primary care setting,15–19 and scarce studies have analysed the hospital setting, where health spending is higher. Studies in the hospital setting have assessed the concept of low-value care in general,20 or consulted the opinion of directors and division chiefs.21,22 Yet, as far as we know, little is known about barriers and facilitators in this setting.
The aims of this study were to explore healthcare professionals’ opinions about low-value practices, identify practices of these kind possibly present in the hospital and barriers and facilitators to reduce them.
MethodStudy design and settingWe used a mixed methodology through an online survey and two focus groups. The study took place between January 2016 and June 2017 in the Vall d’Hebron University Hospital, a tertiary university hospital in Spain with more than 1000 beds. It was approved by the Vall d’Hebron Clinical Research Ethics Committee.
In the on-line survey we assessed doctors’ opinions about a set of recommendations to reduce low-value practices, and practices of this kind possibly present in the hospital. Survey results were complemented with focus groups with health professionals to identify additional low-value practices possibly present in the hospital and barriers and facilitators to reduce them.
Online survey- 1)
Selection of recommendation to reduce low-value practices
The recommendations were obtained from DianaHealth.com, an open access on-line database of appraisals about healthcare interventions considered of low value by several initiatives worldwide.23 From the recommendations available in the database, we randomly preselected 200 and then, we selected from five and up to ten recommendations per specialty where the intervention and the specialty in reference were available in the hospital. When recommendations related to the same population and the same intervention were selected, we kept only one, preferably from a local initiative. When a given specialty was found to have less than five recommendations, the database was consulted again.
- 2)
Survey's sample and process
The survey was aimed at all doctors from the specialties related to the included recommendations, residents were excluded.
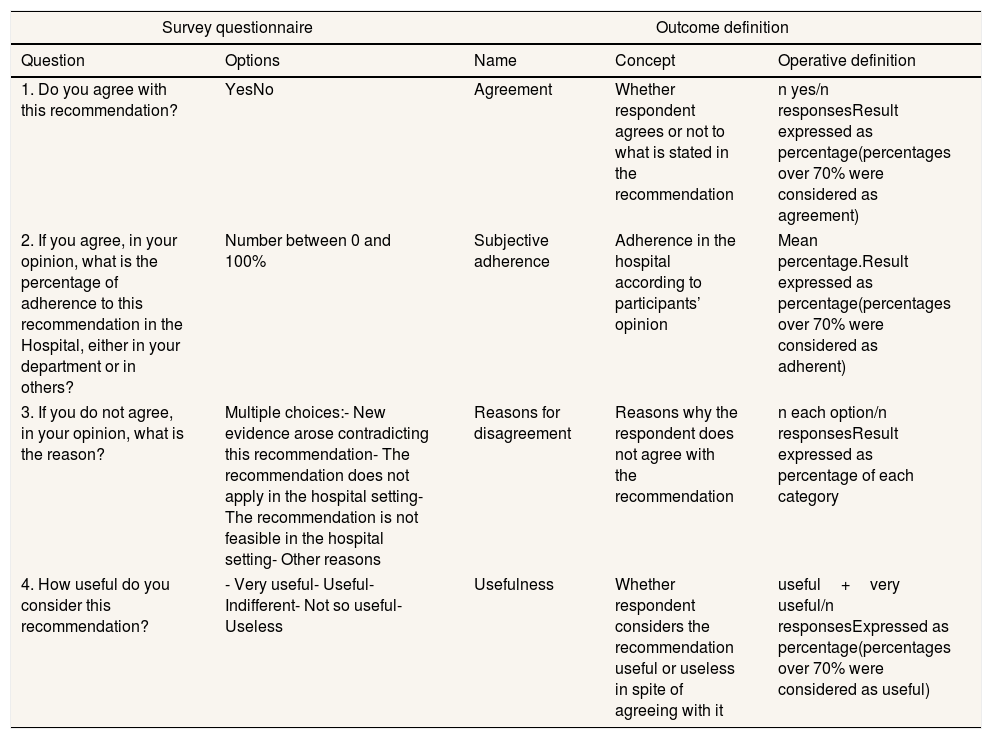
In the questionnaire, participants were asked to specify whether they were specialists or residents and their specialty. No personal information was asked. According to doctors’ specialty, the form displayed a list of 5 to 10 recommendations and four questions about them that are shown in Table 1. The questionnaire was tested before collecting data; completion time was between 10-20minutes.
Survey questionnaire and outcome definition.
| Survey questionnaire | Outcome definition | |||
|---|---|---|---|---|
| Question | Options | Name | Concept | Operative definition |
| 1. Do you agree with this recommendation? | YesNo | Agreement | Whether respondent agrees or not to what is stated in the recommendation | n yes/n responsesResult expressed as percentage(percentages over 70% were considered as agreement) |
| 2. If you agree, in your opinion, what is the percentage of adherence to this recommendation in the Hospital, either in your department or in others? | Number between 0 and 100% | Subjective adherence | Adherence in the hospital according to participants’ opinion | Mean percentage.Result expressed as percentage(percentages over 70% were considered as adherent) |
| 3. If you do not agree, in your opinion, what is the reason? | Multiple choices:- New evidence arose contradicting this recommendation- The recommendation does not apply in the hospital setting- The recommendation is not feasible in the hospital setting- Other reasons | Reasons for disagreement | Reasons why the respondent does not agree with the recommendation | n each option/n responsesResult expressed as percentage of each category |
| 4. How useful do you consider this recommendation? | - Very useful- Useful- Indifferent- Not so useful- Useless | Usefulness | Whether respondent considers the recommendation useful or useless in spite of agreeing with it | useful+very useful/n responsesExpressed as percentage(percentages over 70% were considered as useful) |
We sent an email to invite doctors to participate in the survey explaining the purpose of the study and a link to the questionnaire. Two reminders were sent one and two months later. Participation was anonymous, voluntary and not economically compensated.
- 3)
Survey analysis
Doctors’ opinion was assessed through the following outcomes: agreement, subjective adherence, reasons for disagreement and usefulness. Outcomes definition are shown in Table 1. The unit of analysis was doctors’ response. We compared results by type of specialty: medical and surgical specialties and by type of intervention in four categories: diagnostic images, diagnostic laboratory tests and procedures, pharmacological therapies and non-pharmacological therapies.
The low-value practices possibly present in the hospital were identified through a composite outcome defined as those practices from recommendations with an agreement over 70% and a subjective adherence under 70%. Usefulness was not taken into account in the composite outcome since we were interested in identifying low-value practices, even when doctors may consider the recommendation as not useful. Data was analysed with SPSS v.23..
Focus group- 1)
Focus groups’ sample and process
One focus groups included professionals from the surgical field and the other from the medical field. A convenience sample of 20 participants (10 per group) was selected from the staff database using the following criteria: even distribution according to sex and age (<35, 35-50 and>50 years) and at least one active researcher, one specialist in diagnostic tests and one nurse should be included.
We sent an invitation letter by email to the participants. In cases where the invitation was declined, we looked for another candidate following the same selection criteria. The two groups worked in face-to-face single sessions of 90minutes each. Before the session, all the participants gave verbal consent to participate in the study and to audio-record the session. One of the researchers (LAM), an external expert with over ten years of experience in qualitative research methodology, conducted the sessions, and a second researcher (MSD), recorded them and made notes. None of them knew the participants.
A pre-defined discussion guide available in Table I in the online Appendix was used in the session. The discussion included examples of low-value practices; individual, institutional and social factors leading to low-value practices or difficulties when trying to avoid them; and factors that help to reduce or avoid low-value practices.
- 2)
Focus groups analysis
We analysed the audio-records and notes of the two sessions with a phenomenological approach, using the paradigm of grounded theory.24,25 LAM transcribed audio-records and notes, keeping participants names and specialties anonymised.
Verbatim were coded using a matrix proposed a priori by the Agency for Health Quality and Assessment of Catalonia, based on a similar study carried out in primary care (in process of publication). In a first phase, we used an open coding, creating labels to identify topics; and then we classified them as barriers or facilitators. In a second phase we used axial coding to relate topics in constructs called categories. These categories were grouped into four levels: micro (related to individuals: patients and health professionals), meso (related to Doctor-Patient relationship and management and processes in the institution), macro (related to the Health system) and external factors (outside the Health system).
All researchers discussed and reviewed the organisation of themes until consensus was achieved. The analysis included a comparison between medical and surgical specialties. Data was analysed with the software Atlas.Ti v.6. The results and conclusions of the analysis were returned to participants for comment and feedback.
ResultsSurveyFrom 2475 recommendations and appraisals to reduce low-value practices available in DianaHealth.com, we included 134 recommendations applicable interventions available in our hospital: 65 (49%) on diagnostic tests, 53 (40%) on pharmacological therapies and 16 (12%) on non-pharmacological therapies, including surgery and physical therapy. The recommendations, specialty, type of intervention, and source are shown in Table II in the online Appendix.
A total of 169 doctors from 25 specialties responded the survey. They gave their opinion on 127 of the 134 recommendations (total of responses=1183). Response rate by specialty ranged from 7% to 100% (Figure I in the online Appendix), being 28% and 18% in medical and surgical specialties respectively.
- 1)
Agreement
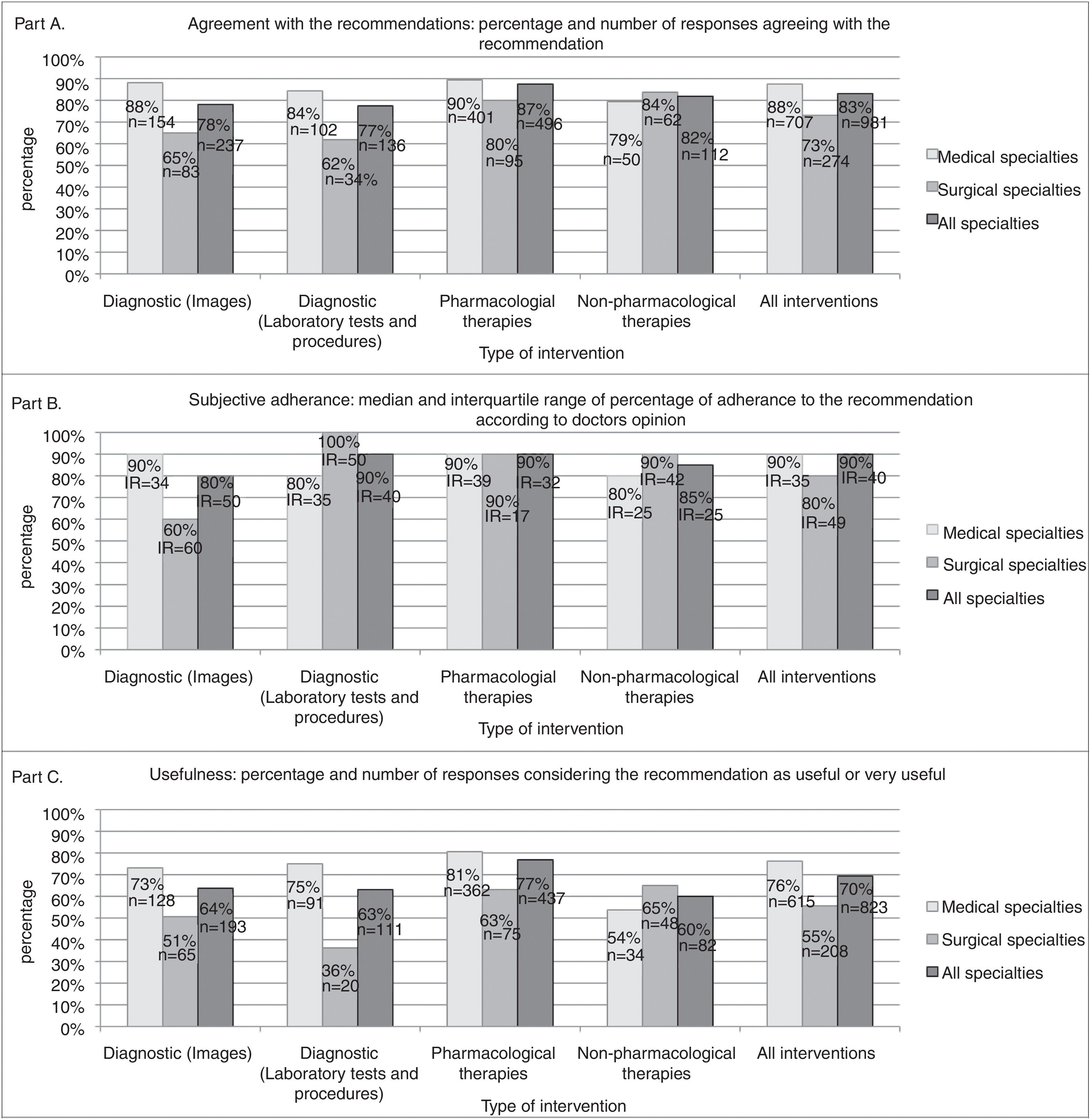
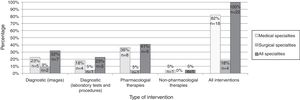
Figure 1 A shows aggregated results of doctors’ agreement by specialty and type of intervention. The proportion of responses where doctors agreed with a recommendation was over 70% in all type of recommendations, except in those on diagnostic tests in the group of surgical specialties. For example, one out of 11 urologists (agreement of 9%) agreed on a recommendation about prostate biopsy for histological confirmation if clinical suspicion of prostate cancer is high (results of individual recommendations are shown in Table III in the online Appendix).
In 42 (33%) recommendations, at least one doctor did not agree with the recommendation. Reasons of disagreement were: new evidence arose contradicting this recommendation (9 out of 66 responses=13%); recommendation did not apply in the hospital setting (12%); and recommendation was not feasible in the hospital setting (5%). Other reasons were explained in 70% (n=46) of cases; they were related mainly to the use of a test to orientate the treatment and concerns about missing the right diagnosis.
- 2)
Subjective adherence
Figure 1 B shows aggregated results of subjective adherence. The median percentage of subjective adherence was over 70% in all type of recommendations, except in those on diagnostic images in the group of surgical specialties.
- 3)
Usefulness of recommendations
Figure 1C shows aggregated results of usefulness. In total, in 70% of responses, participants considered the recommendations as useful or very useful. However, it was under 70% in all type of interventions in the surgical specialties. For example, two out of 14 specialists considered a recommendation advising not to use injectable drugs locally for nonspecific low back pain as useful or very useful (usefulness: 14%).
- 4)
Low-value practices possibly present in the hospital
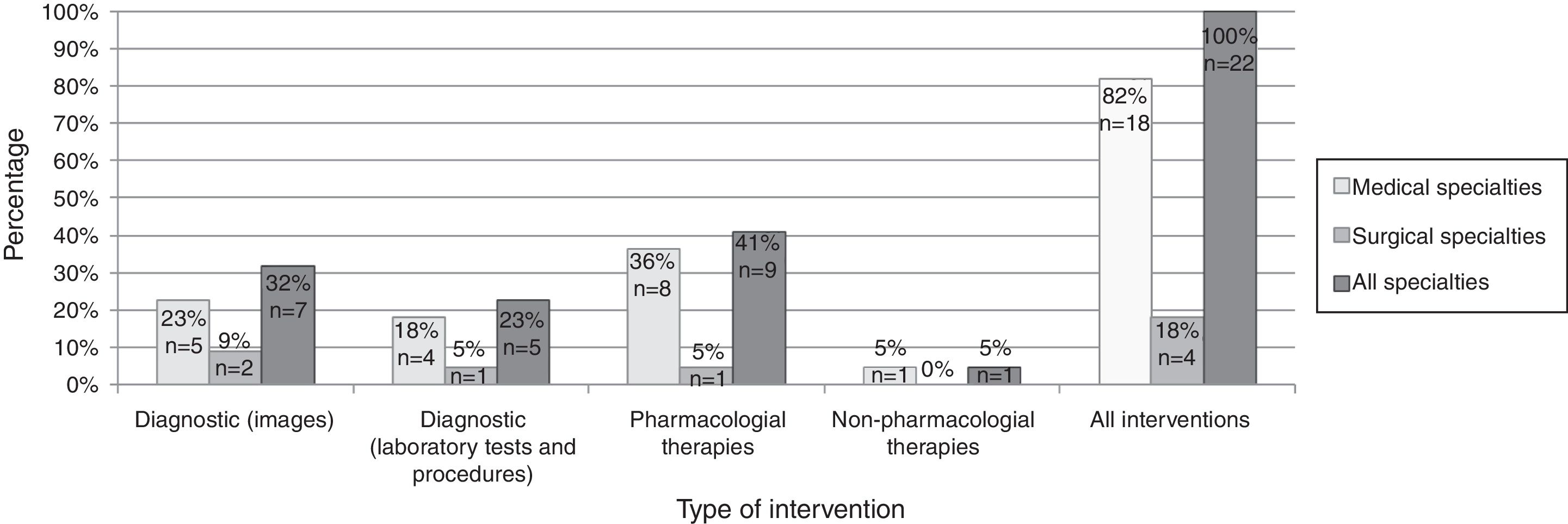
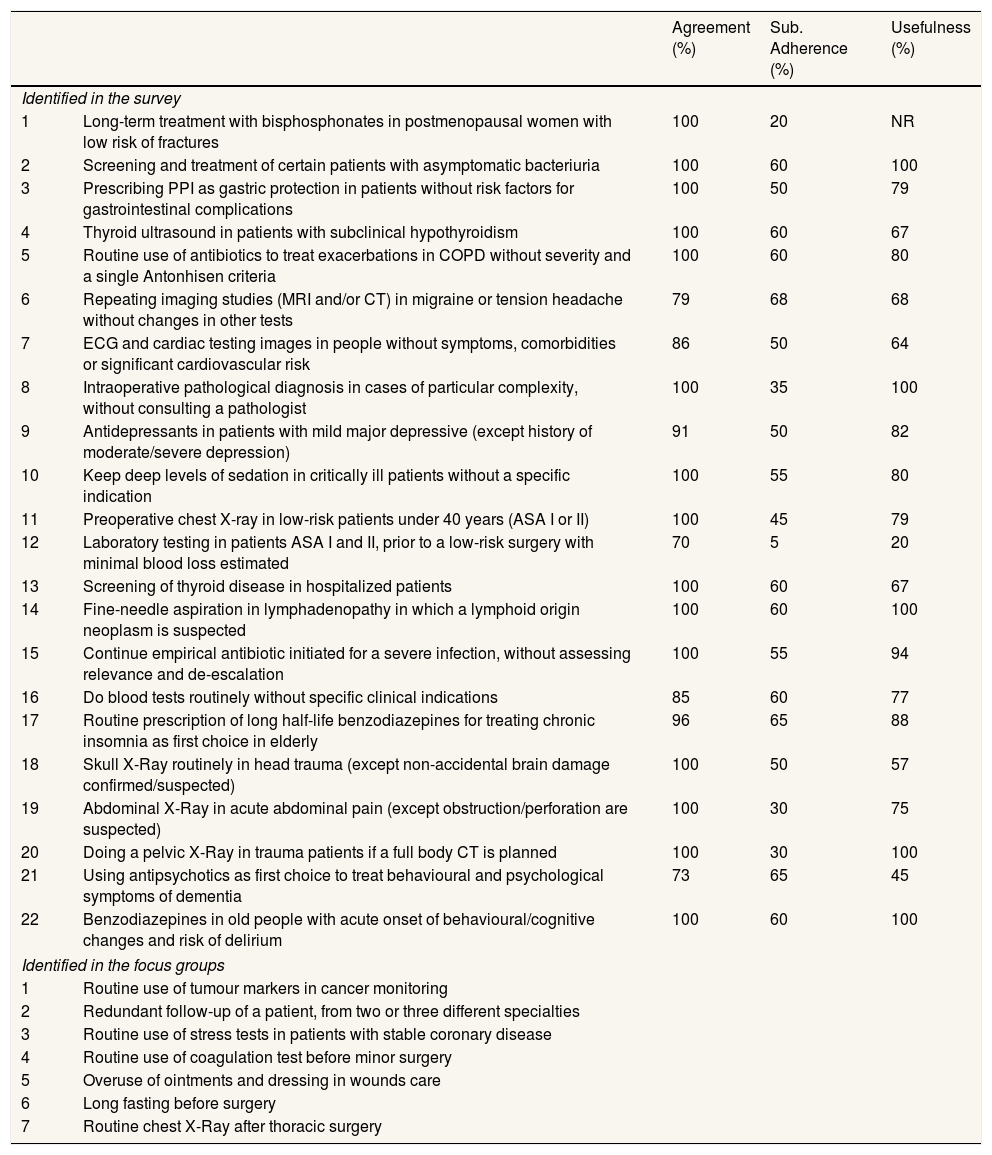
Practices from 22 recommendations had an agreement of 70% or more and subjective adherence under 70%; they represent 16% of the 134 recommendations. The distribution of these practices by specialty and type of intervention is shown in the Figure 2. In 14 out of the 22 (64%) recommendations usefulness was 70% or more.
Focus groupEight professionals participated in the group of medical specialties and seven in the surgical group. Five doctors could not attend the session. The composition of each group is described in Table IV in the online Appendix.
- 1)
Low-value practices possibly present in the hospital
Participants gave seven examples of low-value practices present in the hospital that are summarised in Table 2.
- 2)
Barriers for reducing low-value practices
Low-value practices possibly present in the hospital.a
| Agreement (%) | Sub. Adherence (%) | Usefulness (%) | ||
|---|---|---|---|---|
| Identified in the survey | ||||
| 1 | Long-term treatment with bisphosphonates in postmenopausal women with low risk of fractures | 100 | 20 | NR |
| 2 | Screening and treatment of certain patients with asymptomatic bacteriuria | 100 | 60 | 100 |
| 3 | Prescribing PPI as gastric protection in patients without risk factors for gastrointestinal complications | 100 | 50 | 79 |
| 4 | Thyroid ultrasound in patients with subclinical hypothyroidism | 100 | 60 | 67 |
| 5 | Routine use of antibiotics to treat exacerbations in COPD without severity and a single Antonhisen criteria | 100 | 60 | 80 |
| 6 | Repeating imaging studies (MRI and/or CT) in migraine or tension headache without changes in other tests | 79 | 68 | 68 |
| 7 | ECG and cardiac testing images in people without symptoms, comorbidities or significant cardiovascular risk | 86 | 50 | 64 |
| 8 | Intraoperative pathological diagnosis in cases of particular complexity, without consulting a pathologist | 100 | 35 | 100 |
| 9 | Antidepressants in patients with mild major depressive (except history of moderate/severe depression) | 91 | 50 | 82 |
| 10 | Keep deep levels of sedation in critically ill patients without a specific indication | 100 | 55 | 80 |
| 11 | Preoperative chest X-ray in low-risk patients under 40 years (ASA I or II) | 100 | 45 | 79 |
| 12 | Laboratory testing in patients ASA I and II, prior to a low-risk surgery with minimal blood loss estimated | 70 | 5 | 20 |
| 13 | Screening of thyroid disease in hospitalized patients | 100 | 60 | 67 |
| 14 | Fine-needle aspiration in lymphadenopathy in which a lymphoid origin neoplasm is suspected | 100 | 60 | 100 |
| 15 | Continue empirical antibiotic initiated for a severe infection, without assessing relevance and de-escalation | 100 | 55 | 94 |
| 16 | Do blood tests routinely without specific clinical indications | 85 | 60 | 77 |
| 17 | Routine prescription of long half-life benzodiazepines for treating chronic insomnia as first choice in elderly | 96 | 65 | 88 |
| 18 | Skull X-Ray routinely in head trauma (except non-accidental brain damage confirmed/suspected) | 100 | 50 | 57 |
| 19 | Abdominal X-Ray in acute abdominal pain (except obstruction/perforation are suspected) | 100 | 30 | 75 |
| 20 | Doing a pelvic X-Ray in trauma patients if a full body CT is planned | 100 | 30 | 100 |
| 21 | Using antipsychotics as first choice to treat behavioural and psychological symptoms of dementia | 73 | 65 | 45 |
| 22 | Benzodiazepines in old people with acute onset of behavioural/cognitive changes and risk of delirium | 100 | 60 | 100 |
| Identified in the focus groups | ||||
| 1 | Routine use of tumour markers in cancer monitoring | |||
| 2 | Redundant follow-up of a patient, from two or three different specialties | |||
| 3 | Routine use of stress tests in patients with stable coronary disease | |||
| 4 | Routine use of coagulation test before minor surgery | |||
| 5 | Overuse of ointments and dressing in wounds care | |||
| 6 | Long fasting before surgery | |||
| 7 | Routine chest X-Ray after thoracic surgery | |||
ASA: American Society of Anaesthesiologists’ classification; COPD: chronic obstructive pulmonary disease; CT: computed tomography scan; ECG: electrocardiogram; MRI: magnetic resonance imaging; NA: No response; PPI: proton pump inhibitors.
See the online Appendix to read the full text of the recommendation supporting the low-value practice.
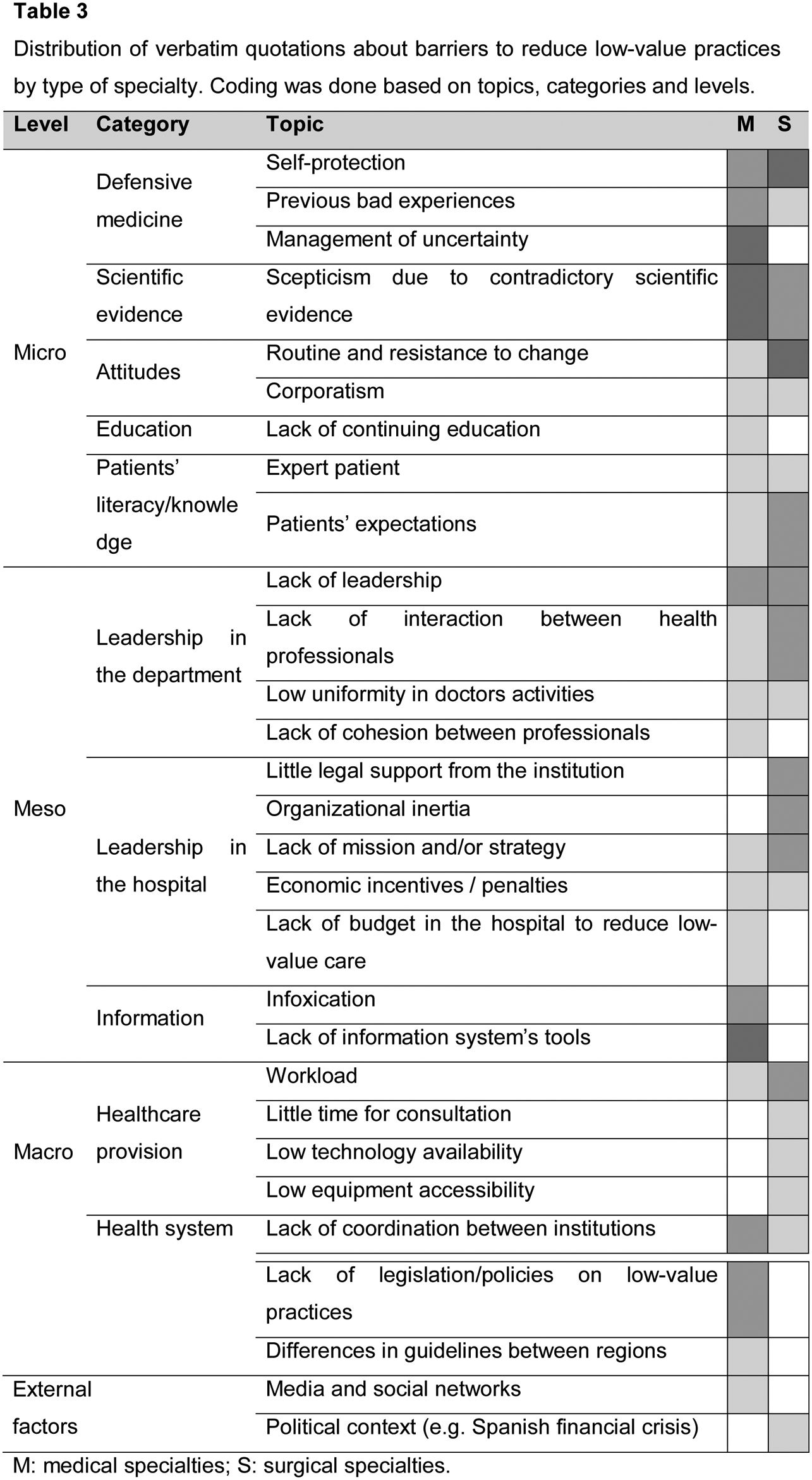
Most of the quotations were about barriers. Several topics were about individuals (micro level) and interactions between professionals and the organisation (meso level). At the micro level, the most common barrier was related to the category of defensive medicine (Table 3): “…in my case, is better to have one test more than one test missing. Because, if you miss something that may have dramatic consequences, for instance an undetected recurrence. So, you ended up asking for that test. Even though you know… you are 95% sure you will not find anything bad”.
Regarding scientific evidence, participants considered evidence-based resources excessive and sometimes outdated and even contradictory, leading to a low confidence and low adherence to clinical recommendations. Patients’ literacy and knowledge was considered as a barrier when expert patients demand specific tests that doctors may consider of low-value in a given context.
At the meso level, lack leadership, lack of interaction between professionals and low uniformity in doctors’ activities were perceived as important barriers; for instance: duplicity in diagnostic tests between departments during follow-up, or criteria variability when ordering diagnostic tests or prescribing treatments. Duplicity was classified as a barrier at the meso level because most of the cases it is related to lack of coordination at an institutional level; however, there are duplicities that may be related to professionals’ misuse of tests, for instance when tests are made unnecessarily often, e.g. the measurement of thyroid-stimulating hormone before 6 weeks after modifying the dose, or taking daily sampling in critical patients (that may induce anaemia in elderly).
When comparing between medical and surgical groups, medical specialties mentioned topics that did not appear in the surgical group, for instance the management of uncertainty or excess of information (infoxication). On the other hand, surgical specialties expressed concerns about legal support from the institution that were not mentioned in the medical specialties’ group (Table 3).
- 3)
Facilitators for reducing low-value practices
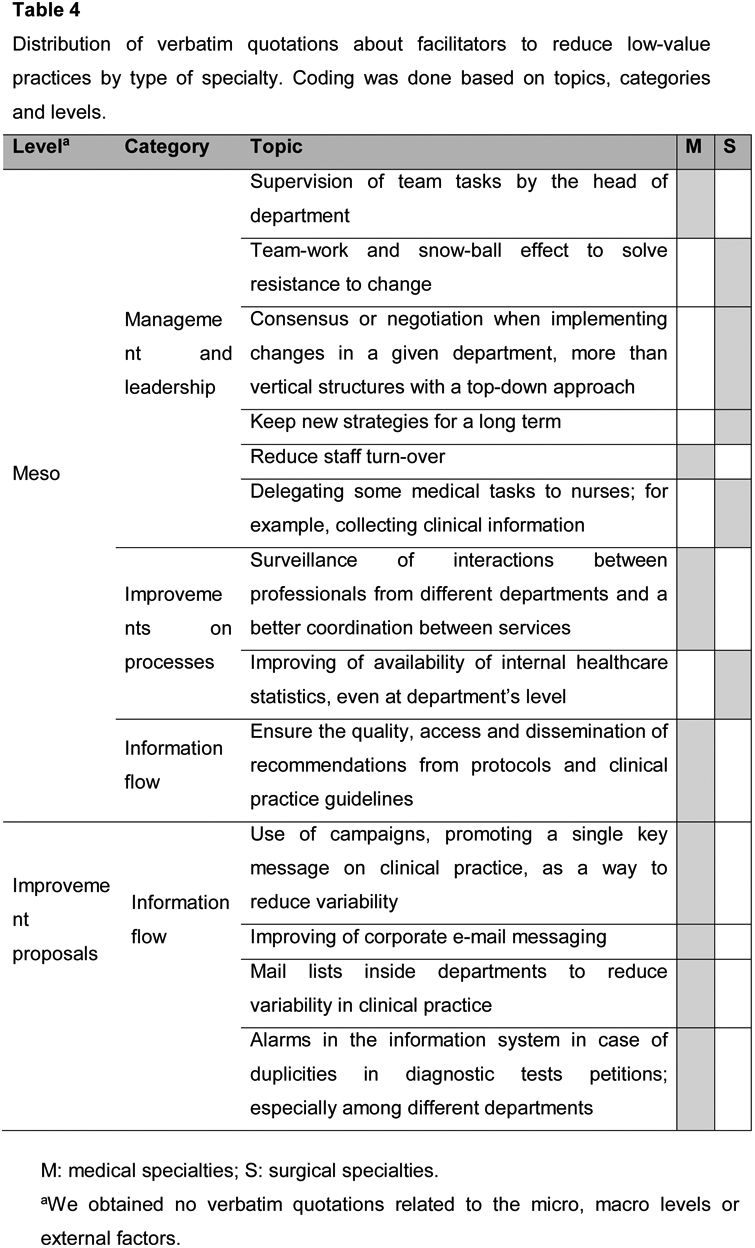
All the facilitators suggested by the participants were related to the meso-level barriers. Discussion was mostly about management and leadership where teamwork was considered as a facilitator: “…You will always find 20% of people that will not agree with you. teamwork is essential. because if one team member starts to turn the wheel, and another team member does the same, after a while the wheel will turn automatically”. See more examples of verbatim in Tables V and VI in the online Appendix. Some verbatim were specific improvement proposals that may reduce low-value practices (Table 4).
Distribution of verbatim quotations about facilitators to reduce low-value practices by type of specialty. Coding was done based on topics, categories and levels.
M: medical specialties; S: surgical specialties.
aWe obtained no verbatim quotations related to the micro, macro levels or external factors.
The aims of this study were to explore healthcare professionals’ opinions about low-value practices, identify practices of these kind possibly present in the hospital and barriers and facilitators to reduce them.
Specialists showed an acceptable agreement with 134 recommendations aimed to reduce low-value practices (83%), and in most responses the recommendations were considered useful or very useful (70%). Recommendations from Choosing Wisely campaigns and similar seem to be good at identifying low-value practices, as concluded by other authors.15 According to our results, local campaigns such as Essencial13 and Commitment to quality of the Spanish scientific societies14 may be also good.
Agreement in general, was lower in surgical specialties than in medical specialties, reflecting different perceptions of low-value care of professionals according to their specialty, as reported in Colla et al.15 in the primary care setting. There was also a smaller proportion of surgeons considering useful or very useful the recommendations on low-value practices (55% versus 76%). Reasons why a given recommendation to reduce a low-value practices is considered useless may varied: is considered incapable of producing any change in clinical practice; it refers to uncommon tests or treatments; the low value of the practice is too obvious to be reinforced through a recommendation. These reasons should be explored in future studies.
From the 134 recommendations analysed in the survey, 22 (16%) were about practices possibly present in the hospital according to doctors’ opinion. In the focus groups we identified seven more. These numbers may seem small, and the amount of low-value practices that are really present in the hospital may be more or less than this, however, we consider them a good point to start working to reduce them.
Regarding barriers to reduce low-value care, defensive medicine was identified as an important barrier perceived by professionals to reduce low-value practices, especially in the medical specialties. Other studies have identified this as a factor for low-value practices.16,20 The origin of this barrier have been associated with doctor-patient communication.26 Dialog between doctors and patients is probably becoming more complex due to increasing patients’ literacy and knowledge. Furthermore, expert patients’ demands for tests that doctors may consider of low-value suggest a paradox: while it is a low-value practices, it may contribute to building trust between professionals and patients. Talking about low-value practices is perceived as difficult; for instance, Brandt et al.27 found that, even though 91% of doctors would choose high-value care; in almost all cases they would not include the concept of value in their conversations with patients. However, emerging evidence shows that patients seem ready to de-adopt low-value practices.17 Provision of education to patients can help improve knowledge around unnecessary care.
Scepticism due to excessive and contradictory scientific evidence was another important barrier. Even though evidence of good quality is fundamental, Grover et al.18 found that greater knowledge of guidelines to reduce low-value practices is associated with greater cost-consciousness; however, it is not associated with less use of low-value interventions. This should make us aware that knowledge is not enough to reduce low-value care, and that other resources are needed.28
Facilitators included teamwork in order to defeat resistance to change from some individuals; more consensus, instead of top-down instructions and better information flow. Interventions aimed to reduce low-value should be multicomponent,29 involving both patient and clinician roles, as well as bottom-up and top-down interventions. We obtained fewer verbatim quotations about facilitators, in comparison with the number of quotations about barriers; this was because both groups spent less time discussing this section.
Differences between specialties found in the survey might be explained either by the recommendations selected for the survey, or by a different perception of low-value care among doctors from surgical specialties. However, differences were also found in the focus groups, reinforcing the second hypothesis. In the focus groups, while surgical specialties remarked legal support, medical specialties showed more concern about contradictory evidence and management of uncertainty. Legal concerns are not a surprise considering that lawsuits have been traditionally more common in surgical than in medical specialties.
Strengths and weaknesses of this studyThe main limitation of our study is a low representativeness in some specialties where the response rate was low. Probably those responding to the survey are “early adopters” or the most conscious about low-value care. However, most of our findings are consistent with other studies,15,18,19,27 even in studies assessing a different set of recommendations from the same or other initiatives. Strengths include the mixed methodology using quantitative and qualitative methods that gave us complementary views on the low-value practices issue. Furthermore, as far as we know this is the first study comparing medical and surgical specialties, and assessing agreement, adherence and usefulness for individual recommendations in the hospital setting. Several studies have assessed doctors’ perspectives either about the concept of low-value care in general,17–20,26–29 or focussing on recommendations on only one specialty15,18,19,21,27,30 and most of them in the primary care setting.15–19 Besides, our methodology led us to identify potential low-value practices present in the hospital.
Implications for clinicians and policymakersThis work shows caregivers, healthcare managers, policy-makers, and academics key elements for developing interventions to reduce low-value care. The survey led us to identify 22 potential low-value practices in our hospital, and the focus groups seven more, as well as the main barriers and facilitators to reduce low-value care; highlighting that interventions to reduce low-value practices should facilitate decision- making and doctors’ and patients’ confidence in medical decisions. This methodology may be applied by other hospitals and medical centres in order to identify low-value practices, barriers and facilitators in their own settings.
Based on the results of our study, a new commission was created in our hospital to address low-value practices, including a mailbox to facilitate their reporting and a multidisciplinary team to work in the development of strategies to reduce them.31
Recommendations for further researchFuture research should focus on the development and assessment of strategies to facilitate doctor-patient communication specifically related to low-value practices. These tools should take into possible differences between medical and surgical specialties, and also, differences between diagnostic and therapeutic interventions.
ConclusionsHigh agreement to recommendations to reduce low-value practices and high perception of usefulness probably reflect great awareness of low-value care in the hospital setting. Future interventions to reduce low-value care should be designed to foster confidence in decision-making process between professionals and patients and teamwork. These interventions should take into account different needs and perceptions found between medical and surgical specialties. Surveys and focus groups applied locally to know health professionals’ opinions may contribute to identify low-value practices locally in the hospital.
Low-value care includes practices with little or no clinical benefit that may harm patients, and lead to a waste of resources. Interventions of this kind threaten patients’ safety and the quality and sustainability of health systems. Interventions to reduce them are needed.
What does this study add to the literature?The survey led us to identify 22 low-value clinical practices possibly present in the hospital, and the focus groups seven more, as well as the main barriers and facilitators related to low-value practices in the medical and surgical fields. Interventions to reduce these practices should include mechanisms to facilitate decision-making and doctors’ and patients’ confidence in medical decisions.
Clara Bermúdez-Tamayo.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsD. Osorio, S. Romea-Lecumberri, M. Solans-Domenech and L. Arroyo-Moliner contributed to development of the study methods. D. Osorio, S. Romea-Lecumberri, M. Solans-Domenech and L. Arroyo-Moliner directed and managed implementation of the study. D. Osorio, M. Solans-Domenech and L. Arroyo-Moliner provided data collection and management. D. Osorio, S. Romea-Lecumberri, A. Ribera, M. Ballesteros, M. Solans-Domenech and L. Arroyo-Moliner led analysis and interpretation of the findings reported here. D. Osorio and L. Arroyo-Moliner wrote the manuscript, with contributions from S. Romea-Lecumberri, A. Ribera, M. Ballesteros and M. Solans-Domenech. All authors read and approved the final submission.
A**ck**nowledgementsWe would like to thank to the Agency for Health Quality and Assessment of Catalonia (AQuAS, as per the acronym in Catalan) for their support in the design and performance of the focus group. Also to Dr. Sergi Bellmunt Montoya for his advice during the publication process. D. Osorio is a PhD candidate in Methodology of Biomedical Research and Public Health at the Universitat Autònoma de Barcelona, Spain.
FundingNone.
Conflicts of interestNone.