To compare the morbidity burden of immigrants and natives residing in Aragón, Spain, based on patient registries in primary care, which represents individuals’ first contact with the health system.
MethodsA retrospective observational study was carried out, based on linking electronic primary care medical records to patients’ health insurance cards. The study population consisted of the entire population assigned to general practices in Aragón, Spain (1,251,540 individuals, of whom 12% were immigrants). We studied the morbidity profiles of both the immigrant and native populations using the Adjusted Clinical Group System. Logistic regressions were conducted to compare the morbidity burden of immigrants and natives after adjustment for age and gender.
ResultsOur study confirmed the “healthy immigrant effect”, particularly for immigrant men. Relative to the native population, the prevalence rates of the most frequent diseases were lower among immigrants. The percentage of the population showing a moderate to very high morbidity burden was higher among natives (52%) than among Latin Americans (33%), Africans (29%), western Europeans (27%), eastern Europeans and North Americans (26%) and/or Asians (20%). Differences were smaller for immigrants who had lived in the country for 5 years or longer.
ConclusionLength of stay in the host country had a decisive influence on the morbidity burden represented by immigrants, although the health status of both men and women worsened with longer stay in the host country.
Comparar la carga de morbilidad de inmigrantes y nativos residents en Aragón a partir de los datos poblacionales procedentes de atención primaria, la cual representa el primer nivel de contacto de los individuos con el sistema sanitario.
MétodoEstudio observacional retrospectivo basado en la historia clínica electrónica de atención primaria y la base de datos de usuarios de Aragón. La población de estudio la conforman los 1.251.540 individuos asignados a alguno de los centros de salud de Aragón (12% de ellos inmigrantes). Los perfiles de morbilidad se estudiaron a través del sistema ACG. Se realizaron regresiones logísticas para comparar la población inmigrante y nativa, ajustando por edad y sexo.
ResultadosSe confirmó la teoría del “inmigrante sano”, en especial en los hombres. La prevalencia de las enfermedades más frecuentes fue menor entre los inmigrantes. La proporción de la población con una carga de morbilidad entre moderada y muy elevada fue mayor en autóctonos (52%) que en latinoamericanos (33%), africanos (29%), europeos occidentales y norteamericanos (27%), europeos del este (26%) y/o asiáticos (20%). Las diferencias fueron menores en los inmigrantes con estancias mayores de 5 años.
ConclusiónLa duración de la estancia en el país de acogida influye de manera decisiva en la evolución de la carga de morbilidad que presenta la población inmigrante, produciéndose un empeoramiento de la misma a medida que aumenta la estancia en el país de acogida.
In 2010, an estimated 72.6 million immigrants lived in the European region.1 In many European countries, one out of ten people is an immigrant. This implies a need for better understanding of the health characteristics of immigrant populations and the inclusion of such specific characteristics in health policy design.1,2 Although a growing concern exists in countries with well-developed healthcare systems regarding a possible “pull effect” of patients with illnesses that would likely benefit from better-quality medical attention,1,3,4 it has been shown that overall, the European immigrant population is healthier than the native population. This phenomenon has been described as the “healthy migration effect”.5,6
To date, studies that have measured the health status of immigrant populations in countries such as Canada,7 United States,8 Germany9 or Spain10 have been based on death registries and health surveys.11,12 To the best of our knowlwedge, there are no studies that used primary sources of information such as medical records. While mortality records indicate a better overall level of health in the immigrant population compared to natives, surveys have shown contradictory results.11,12
It is acknowledged that differences exist between the health patterns of the native and immigrant population5,13 and among immigrants from diverse geographical areas of origin,5,10 and that immigrants’ health worsens with an increased duration of stay in the host country.5,11 However, few studies have investigated these and other differences in depth, due in part to the lack of internationally validated methods for measuring and classifying morbidity burden so that comparisons can be made.
The Adjusted Clinical Group System (ACGs) is an example of this type of tool. The ACG System is a patient classification system that measures populations’ health status according to their case-mix, in order to assess and predict the use of healthcare services.14
In Spain, prior to 2012, universal healthcare coverage existed for immigrants, regardless of their legal status.1,4 The country has received a constant and growing flow of immigrants primarily displaced for economic reasons and who come from many different countries in all continents, excepting Oceania. In Aragón, an autonomous region in the north of Spain, foreigners represented approximately 12% of the total population in 2010, an average similar to that in the whole of Spain.15
The objective of this study is to analyse the morbidity burden of the immigrant population in Aragón and to compare these results with those of the native population. For this purpose, an internationally validated methodology as is the ACG System was used, based on information from patients’ primary care medical records. Our goal is to provide objective and reliable population-level information to enable comparisons with other European and international contexts and to support equitable decision-making regarding healthcare provision in Spain.
MethodsDesign, study population and variablesThis was a retrospective observational study. Data were obtained from primary care electronic medical records and patients’ health insurance card database, both linked via an anonymised patient identifier. The study population comprised all individuals covered by the region's community health centres (n=1,251,540). Since 1986 and until recently, Spain, and therefore the region of Aragón, has used a tax-based health system with universal coverage for the entire population. The primary care model is based on multidisciplinary teams built around a general practitioner, who acts as a gatekeeper to the healthcare system and more specialised care. Each team is assigned a geographically delimited population, and all types of patients and health problems are initially attended at primary care centres.
For each patient, demographic variables regarding age, sex and nationality were extracted from health insurance cards along with their active diagnoses in 2010. These were coded according to the International Classification of Primary Care (ICPC-2).16 Subsequently, diagnostic information was processed by means of the ACG® System (version 10)17 to obtain two different outcomes related to morbidity measurements. First, the ICPC-2 codes were grouped according to their Expanded Diagnostic Clusters (EDCs) based on the clinical, diagnostic and therapeutic similarities of the diseases. EDCs facilitate the management of diagnostic information because the many codes used to describe different forms of the same or related disease (e.g., chronic bronchitis and COPD) are all clustered into a single EDC. Second, using the age, sex and combination of all of the diagnostic episodes (ICPC-2 codes), a single ACG category out of 93 total categories was assigned to each individual. When building the ACGs, besides the patients’ age and sex, different clinical dimensions of their diseases are considered such as duration (acute, recurrent or chronic), severity (minor and stable versus major and unstable), diagnostic certainty (symptomatic versus documented disease), aetiology (infection, injury or other), and specialty care involvement (e.g., medical, surgical or obstetrical). Specific disease clustering in an individual is also considered. As a result, individuals within a given ACG experience a similar morbidity burden over a 1-year period. For the sake of parsimony, ACGs with similar expected morbidity burden -and consequently resource use- are aggregated into so-called Resource Utilisation Bands by the System: RUB 0, non-users; RUB 1, healthy users; RUB 2, low morbidity; RUB 3, moderate morbidity; RUB 4, high morbidity; and RUB 5, very high morbidity. Thus, each individual is additionally assigned a RUB category.
The term immigrant was defined as any person with a non-Spanish nationality, regardless of his or her place of birth and duration of stay in Spain.18 Based on nationality, six areas of origin were distinguished in the study population: Spain, Asia, Africa, Eastern Europe, Latin America, and Western Europe/North America. At the time of the study, almost the entire immigrant population had access to the primary care public network, regardless of the legal status, and was therefore included in the analysis.
To maintain confidentiality, each patient was identifiable only by a unique anonymised code. This study was approved by the Ethics Committee for Clinical Investigation of Aragón (CEICA, for its initials in Spanish).
Statistical analysisDescriptive analyses were performed. To facilitate the analysis by age, four age ranges were created: 0–14, 15–44, 45–64 and >64 years old. Sex and age-standardised prevalence rates for the most frequent EDCs in the native and immigrant populations were calculated. Direct standardisation was performed to prevent differences caused by population distribution taking the Spanish population structure on June 1, 2010 as the reference.15
The RUB distribution according to age group and area of origin and the age and sex-adjusted mean RUB scores were calculated for these same groups. These averages were compared with Student's t-test. Multivariate logistic regression models were conducted to evaluate the magnitude of the differences with regard to morbidity levels within each immigrant subgroup relative to the native population after adjusting for age and sex. To this end, a dependent binary variable was created based on the information supplied by the RUBs: moderate, high and very high morbidity vs. low morbidity, healthy users and non-users (reference category).
Additionally, to asess changes in morbidity burden according to the duration of stay, the models were stratified according to the length of time during which an immigrant had been registered in the patients’ health insurance card database; this variable was classified as <5 and ≥5 years.18 The odds ratios (OR) values and their 95% confidence intervals were graphically represented.
The data were analysed with the STATA statistical package (version 12; StataCorp, College Station, TX, USA) and Excel 2007 (Microsoft Corporation, Redmond, WA, USA) was used for graphical design.
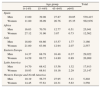
ResultsThe study population comprised 1,251,540 people, of whom 11.9% were immigrants. The distribution by age, sex and country of origin is shown in Table 1, which highlights the high proportion of immigrants between 15–44 years of age and the scarce proportion of immigrants above 64 years. The percentage of women varied according to the area of origin as follows: Latin America, 56%; Eastern Europe, 48%; Asia, 47%; Western Europe and North America, 41% and Africa, 33%.
Age distribution according to sex and area of origin.
| Age group | Total | ||||
| 0–14% | 15–44% | 45–64% | >64% | ||
| Spain | |||||
| Men | 13.00 | 39.08 | 27.87 | 20.05 | 539,415 |
| Women | 11.80 | 36.09 | 26.76 | 25.35 | 562,976 |
| Africa | |||||
| Men | 16.03 | 70.70 | 12.77 | 0.51 | 25,041 |
| Women | 27.12 | 31.96 | 3.87 | 0.73 | 12,562 |
| Asia | |||||
| Men | 18.00 | 64.66 | 15.57 | 1.77 | 3,166 |
| Women | 21.00 | 63.98 | 12.94 | 2.07 | 2,557 |
| Eastern Europe | |||||
| Men | 14.37 | 68.78 | 16.48 | 0.37 | 29,022 |
| Women | 14.59 | 69.72 | 14.80 | 0.89 | 26,989 |
| Latin America | |||||
| Men | 14.70 | 68.42 | 15.56 | 1.32 | 17,913 |
| Women | 10.93 | 68.61 | 18.16 | 2.29 | 23,147 |
| Western Europe and North America | |||||
| Men | 10.19 | 56.75 | 27.95 | 5.11 | 5,202 |
| Women | 14.45 | 57.61 | 22.31 | 5.63 | 3,550 |
The most prevalent EDCs in the immigrant and native populations are shown in Table 2. Although striking similarities exist with respect to the most frequent EDCs in both population groups (14 of the 15 diagnostic groups coincide), the majority of the diagnostic groups, excepting headache, abdominal pain and mouth disorders were less prevalent in immigrants. In immigrants, the diagnosis of depression was not among the 15 most frequent diagnoses; the same was true for abdominal pain in the native population.
Age and sex-standardised prevalence rates of the most frequent conditionsa among natives and immigrants.
| Natives | % | Immigrants | % |
| Acute upper respiratory tract infection | 25.50 | Acute upper respiratory tract infection | 17.36 |
| Hypertensionb | 14.36 | Hypertensionb | 8.91 |
| Disorders of lipoid metabolism | 12.84 | Musculoskeletal signs and symptoms | 8.60 |
| Musculoskeletal signs and symptoms | 10.05 | Disorders of lipoid metabolism | 7.52 |
| Dermatitis and eczema | 7.75 | Disorders of mouth | 6.06 |
| Degenerative joint disease | 6.58 | Nonspecific signs and symptoms | 5.89 |
| Nonspecific signs and symptoms | 6.41 | Dermatitis and eczema | 5.41 |
| Musculoskeletal disorders, other | 6.23 | Headaches | 4.54 |
| Varicose veins of lower extremities | 6.19 | Varicose veins of lower extremities | 4.18 |
| Disorders of mouth | 5.95 | Abdominal pain | 4.13 |
| Depression | 5.52 | Diabetes | 3.62 |
| Gastroenteritis | 4.99 | Musculoskeletal disorders, other | 3.58 |
| Allergic reactions | 4.98 | Gastroenteritis | 3.48 |
| Diabetesc | 4.96 | Degenerative joint disease | 3.34 |
| Headaches | 4.10 | Allergic reactions | 3.20 |
Table 3 shows the distribution of the RUB-defined morbidity burden levels according to the area of origin and age, as well as the age and sex-adjusted mean morbidity burden levels. An inverse distribution can be observed between the immigrant and native populations, with the immigrant population showing a higher proportion of non-users and healthy users and the native population showing moderate to very high morbidity. The highest average RUB value was found in natives (2.07), followed by Africans and Latin Americans (1.62), Western European and North Americans (1.46), Eastern Europeans (1.37) and finally Asians (1.28). The age and sex-adjusted mean RUB value among immigrants was 1.52.
Morbidity burdena distribution according to age and area of origin.
| n | % Non- users | % Healthyusers | % Lowmorbidity | % Moderatemorbidity | % Highmorbidity | % Very highMorbidity | Averageb | p-valuec | |
| Spain | |||||||||
| <15 | 136,540 | 16.78 | 14.15 | 39.30 | 27.59 | 2.15 | 0.02 | 1.89 | |
| 15–44 | 413,990 | 27.11 | 10.00 | 26.48 | 33.70 | 2.68 | 0.04 | 1.76 | |
| 45–64 | 300,983 | 17.90 | 4.64 | 19.83 | 53.78 | 3.54 | 0.31 | 2.27 | |
| >64 | 250,878 | 10.66 | 1.34 | 11.50 | 65.23 | 10.07 | 1.21 | 2.71 | |
| Total | 1,102,391 | 19.57 | 7.08 | 22.84 | 45.60 | 4.53 | 0.38 | 2.07 | – |
| Africa | |||||||||
| <15 | 7,421 | 23.93 | 18.43 | 36.67 | 19.82 | 1.13 | 0.01 | 1.52 | |
| 15–44 | 25,707 | 37.04 | 10.47 | 23.12 | 25.81 | 3.55 | 0.01 | 1.61 | |
| 45–64 | 4,165 | 32.10 | 8.36 | 21.66 | 36.54 | 1.27 | 0.07 | 1.78 | |
| >64 | 310 | 45.16 | 2.58 | 12.90 | 38.06 | 0.97 | 0.32 | 1.47 | |
| Total | 37,603 | 33.97 | 11.74 | 25.55 | 25.92 | 2.80 | 0.02 | 1.62 | <0.001 |
| Asia | |||||||||
| <15 | 1,107 | 42.28 | 15.81 | 29.90 | 11.65 | 0.36 | 0.00 | 1.12 | |
| 15–44 | 3,683 | 52.70 | 7.63 | 20.09 | 17.35 | 2.23 | 0.00 | 1.11 | |
| 45–64 | 824 | 48.06 | 4.61 | 19.30 | 26.94 | 1.09 | 0.00 | 1.37 | |
| >64 | 109 | 35.78 | 2.75 | 19.27 | 36.70 | 5.50 | 0.00 | 1.69 | |
| Total | 4,796 | 49.69 | 8.68 | 21.86 | 18.00 | 1.76 | 0.00 | 1.28 | <0.001 |
| Eastern Europe | |||||||||
| <15 | 5,732 | 31.85 | 16.13 | 32.56 | 18.52 | 0.94 | 0.00 | 1.44 | |
| 15–44 | 38,777 | 44.97 | 9.12 | 20.93 | 22.75 | 2.22 | 0.02 | 1.3 | |
| 45–64 | 8,778 | 43.68 | 5.45 | 17.97 | 31.50 | 1.33 | 0.08 | 1.47 | |
| >64 | 348 | 51.15 | 2.01 | 13.51 | 29.31 | 4.02 | 0.00 | 1.32 | |
| Total | 28,201 | 42.90 | 9.52 | 22.10 | 23.55 | 1.90 | 0.02 | 1.37 | <0.001 |
| Latin America | |||||||||
| <15 | 5,164 | 30.89 | 15.70 | 35.52 | 17.12 | 0.77 | 0.00 | 1.5 | |
| 15–44 | 28,138 | 37.27 | 7.94 | 22.61 | 29.60 | 2.57 | 0.01 | 1.49 | |
| 45–64 | 5,804 | 30.56 | 4.20 | 18.88 | 44.31 | 1.96 | 0.09 | 1.85 | |
| >64 | 766 | 39.16 | 0.65 | 12.53 | 43.60 | 3.92 | 0.13 | 1.7 | |
| Total | 41,060 | 35.36 | 8.14 | 23.41 | 30.79 | 2.26 | 0.03 | 1.62 | <0.001 |
| Western Europe & North America | |||||||||
| <15 | 1,043 | 41.32 | 12.46 | 32.69 | 12.66 | 0.86 | 0.00 | 1.23 | |
| 15–44 | 4,997 | 51.75 | 7.06 | 18.23 | 21.43 | 1.50 | 0.02 | 1.19 | |
| 45–64 | 2,246 | 41.94 | 5.65 | 17.90 | 32.01 | 2.27 | 0.22 | 1.65 | |
| >64 | 466 | 28.33 | 1.72 | 13.52 | 49.79 | 6.01 | 0.64 | 2.1 | |
| Total | 8,752 | 46.74 | 7.06 | 19.62 | 24.61 | 1.86 | 0.10 | 1.46 | <0.001 |
Figure 1 describes the morbidity burden in the adult population by duration of stay, taking into account individulas’ sex and area of origin. The morbidity burden was significantly greater in all immigrants, regardless of their origin, after 5 years of stay in the host country. Similarly, this figure reveals the low morbidity burden among Asians with less than 5 years of stay.
Odds ratios (OR) and 95% confidence intervals derived from multivariate logistic regression analyses among adults. Dependent variables: moderate, high and very high morbidity vs. non-users, healthy users and low morbidity. Reference: Spain (OR=1).
NOTE: models were stratified according to the ammount of time (i.e. <5 and ≥5 years) an immigrant had been registered in the patients’ health insurance card database.
The results of this study show that although the health status of immigrants is initially better than that of natives, thus confirming the so called “healthy migration effect”, immigrants’ health worsens as the duration of stay in the host country increases.
This is the first study including all patients from an extensive geographical area to measure the health status of an immigrant population that benefited from free and universal access to the public health system at the time of the study, regardless of legal or socioeconomic features.1,19 The large size and comprehensiveness of the study sample additionally allowed stratifying the analyses by immigrants’ area of origin increasing the study's external validity.20 Moreover, as far as we know, this is the first study based on primary care data using an internationally validated morbidity burden measurement tool.
A notable finding is that even if the morbidity “profiles” were similar in immigrants and natives with respect to the most frequently registered diagnoses, these showed a lower prevalence in the immigrant population. Similar conclusions have been previously reported,5 but other studies have found a higher prevalence of diabetes mellitus in immigrants,5,21 which was not corroborated by our study. Differences regarding depression (absent from immigrants’ most frequent health problems) and abdominal pain (absent from natives’ most frequent health problems) could be due to actual pathology diverstity, but also to cultural expression of illness, and should be further studied.
Our data confirmed the “healthy migration effect” theory by showing that immigrants’ health status, as measured by a validated tool, was better than that of the native population, even after adjusting for age and sex. Thus, our work adds to the numerous studies that have indicated reduced mortality7–9,13,22–24 and a better health (as perceived from surveys)1,5,11,25 among immigrants. Nevertheless, in a systematic review by Nielsen et al,12 the self-perceived health of immigrants and ethnic minorities was found to be worse than that of natives. Most of the studies in that systematic review focused on immigrants from specific countries, thus impeding the generalisation of the results to overall immigrant population. Moreover, self-perceived health, primary care diagnoses and mortality records offer complementary information that may not always coincide.5
With respect to differences in the morbidity burden according to the area of origin, the healthiest groups were those of Asian and Eastern European origins. The low morbidity observed in Asian immigrants is in agreement with mortality records-based studies conducted in Canada,7 France26 and Denmark.23 Eastern Europeans were also found to have a low mortality rate in the previously cited Danish study,23 but not in the Canadian7 and French studies26 which revealed opposite results. African patients had higher RUB levels in general, a finding that agrees with the majority of studies reporting higher mortality rates in this group,7,23,24 particularly due to cardiovascular causes.10,26 Nevertheless, in the Canadian study by Ng,7 the mortality rate of Africans was among the lowest, while the highest rate was observed in individuals from Western Europe and the United States. The high degree of convergence between results based on mortality records and our data reinforces the validity of the employed methodology.
The very low morbidity burden observed among immigrants over 64 years of age in this study might be partially due to what is known as the “salmon bias”. According to the latter, the lower mortality rate in immigrants stems from the fact that immigrants with serious illnesses return to their countries of origin, seeking their own cultural and family environments when dying.6 Indeed, this finding refutes the “medical tourism” theory used by some western countries to justify restrictions in immigrants’ healthcare rights.1,3,4
Our results confirmed the hypothesis that immigrants’ health worsens as the duration of stay in the host country increases.1,5,7,11,13,27 This finding could be related to worsening socioeconomic conditions,27 changes in the health-illness perception with progressive medicalisation,5 worsening of lifestyles and/or greater use of the health system, which implies an increase in the number of registered diagnoses.5 Anyhow, the observed trend discards the idea that already ill immigrants arrive in Western countries with the aim of receiving medical care.3,4
Among the limitations of this study were those inherent to the employed information source because medical records can contain errors with regard to registered diagnoses. In such case, it could be assumed that the errors would be distributed homogeneously among patients, with independence of their migratory status, and therefore would not affect the differences observed between population groups. The potential system barriers for specific immigrant groups to access health services is unlikely in this study, due to the fact that a free and universal access system existed at the time of the study. Another limitation of our study was the lack of access to patients’ socioeconomic data which means that we could not adjust for these variables, even though they are known to influence individuals’ health levels.22,27 Future population-based studies should include this piece of information. We were not able to include those diagnostic episodes that may be registered exclusively at the hospital level or in private healthcare centres. The use of these type of services seems to be higher by natives than immigrants28 which suggests that differences found in our study would have been even bigger should this information be considered. Last, the fact that some immigrant patients may not get their healthcare insurance cards until they actually become sick could result in a lack of information regarding their health status prior to medical consultation, and the inability to identify immigrants who come to Spain for “medical tourism”. These possible biases would tend to increase the observed differences, thus reinforcing our conclusions with regard to the better health status in immigrants relative to natives.
Future studies should investigate the repercussion of personal socioeconomic circumstances as well as lifestyle factors in the observed differences according to immigrants’ place of origin. Likewise, we believe it is important to study how these findings could improve health and healthcare planning for immigrants in host countries.
Editor in chargeNapoleon Pérez-Farinos.
FundingThis study was supported by grant PI11/01126 from the Carlos III Health Institute of the Spanish Ministry of Economy and Competitiveness.
Conflicts of interestAll authors declare the absence of conflicts of interest.
The rapid increase in the proportion of immigrants in western countries has entailed a rising interest regarding their health status and its repercussion on health systems. Albeit living in poorer socioeconomic conditions, immigrants seem to have better health than that of natives, a phenomenon described as the “healthy migration effect”.
What does this study add to the literature?According to diagnostic data from primary care, immigrants show a lower morbidity burden compared to natives, although the health status of the former worsens with longer stay durations in the host country. The observed trend discards the idea that already ill immigrants arrive in Western countries with the aim of receiving medical care, and calls for further study on how these findings could improve health and healthcare planning for immigrants in host countries.
L. Gimeno-Feliu generated the research question. B. Poblador-Plou processed the data and A. Calderón-Larrañaga carried out the statistical analyses. All authors participated in the interpretation and discussion of results. L. Gimeno-Feliu drafted the manuscript which was revised and approved by the rest of authors.