The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosThis study aims to analyze the risk factors (knowledge, role of health workers, drug Consumption Supervisors activity, side effects of drugs, duration of taking medication, and feeling healthy) for non-adherence to TB patients taking medication at the Puskesmas.
MethodThe research design used in this study was a case control where the population was all patients who visited the working region of the Polonia Public Health Center. The research subjects were 138 samples consisting of 68 cases and 68 controls. The data were analyzed using a tabulation and statistical system using the SPSS program with the Odds ratio test and logistic regression.
ResultIt was found that there was an influence on the role of health workers OR=8,933 (95% CI: 1,085–73.525), side effects of drugs with OR=6,873 (95% CI; 2,435–19,398), felt healthy OR=4,643 (95% CI; 1,247–17,287), and knowledge OR=2,700 (95% CI; 1,083–6,731) It is recommended to be healthy and monitor the occurrence of drug side effects in patients during treatment.
WHO (2003) declared TB as a Global Health Emergency. TB is considered an important problem because approximately 1/3 of the world's population is infected by TB mycobacteria. There are 22 countries with a high burden of TB category. There are 8.9 million sufferers, with 80% in 22 developing countries with 3 million deaths per year. One person can be infected with TB every second and kill 1 million women per year during pregnancy and childbirth.1 In 1998, an estimated 3,617,047 TB cases were recorded worldwide. Most TB cases (95%) and deaths (98%) occur in developing countries, with 3 million deaths per year. Among them, 75% are in the productive age, namely 20–49 years. Due to the dense population and high prevalence, more than 65% of new TB cases and deaths occur in Asia.2
Nationally, Indonesia is still a country that has a lot of tuberculosis. Based on 2010 WHO Global Tuberculosis Report, Indonesia is a country that is recorded as the fifth-largest contributor to pulmonary TB cases in the world after India, China, South Africa, and Nigeria. Irregular treatment is suspected of having caused double immunity of TB germs to drug-resistant TB (DR TB) or Multidrug-resistant (MDR). Irregular treatment behavior is a factor causing failure to achieve a cure.3
Based on this WHO report, tuberculosis causes the death of about 1.3 million people. The mortality rate from this disease is still very high, and until now, pulmonary TB is still one of the goals in the SDGs (Sustainability Development Goals), namely ending the tuberculosis epidemic in the world. Based on the Global TB Report 2018, it is estimated that in 2017 there were 842,000 cases of pulmonary TB (319 per 100,000) and 116,000 deaths due to pulmonary TB (44 per 100,000), including TB-HIV positive.4 From the survey results on the prevalence of tuberculosis, the leading cause of failure of treatment for tuberculosis is the large number of patients who have not been successfully cured due to the high rate of drug resistance, especially infectious patients (AFB positive). This resistance occurs due to irregular and inadequate drug use.1
Based on survey data conducted in 2015, the province of North Sumatra ranks sixth nationally with 165 cases of pulmonary TB per 100,000 population in Indonesia. The achievement of Case Detection Rate (CDR) in North Sumatra Province in 2017 was 47.7%, still far from the CDR figure recommended by WHO, which is 70% and still below the national CDR figure of 64.5%.5
Drug side effects after taking medication also influence Non-adherence to taking medication in TB patients. However, only a small proportion can experience side effects. Monitoring the possibility of side effects is very important. According to a 2003 WHO report, the average patient adherence to long-term therapy for chronic diseases in developed countries is only 50%, while in developing countries, this number is even lower. Treatment adherence requires the patient's active participation in self-care management and collaboration between the patient and the health care provider. Patients who adhere to treatment are those who complete regular and complete treatment without interruption for a minimum of 6–9 months.6
Supervision of patients swallowing drugs requires perseverance and understanding of patients and their families to undergo treatment to completion, and the patient is declared cured with a negative AFB examination (–). Patients are said to be incomplete in treatment if they do not come for more than three days to 2 months from the appointment and are said to be Drop Out if they do not come for more than two consecutive months for treatment. The causes of tuberculosis patients not complying with the reasons for failing to take medication as recommended, not following the rules, stopping doing rehabilitation exercises against diet and lifestyle changes recommended by health practitioners, eliminating some doses, using drugs for the wrong reasons, taking the wrong amount of medication and wrong time, not continuing to take medication until the time limit is set.5
The DOTS (Directly Observed Treatment Shortcourse) strategy is a short-term treatment with close supervision to achieve effective eradication results so that tuberculosis is no longer a health problem.7 Examination of sputum or phlegm containing tuberculosis germs gives a positive AFB result. The discovery of AFB through microscopic examination of sputum is the primary diagnosis. It is said to be AFB (+) if there are two or more sputum AFB (+) or 1 AFB (+) accompanied by radiological results showing active tuberculosis.5 Other examinations can also be carried out with chest X-rays, cultures, and sensitivity tests to support the correct diagnosis.8
Non-compliance in the tuberculosis treatment program with irregularities in taking medication from the amount and type of anti-tuberculosis drugs must be taken both in the intensive and advanced phases.1 If the patient does not follow the TB treatment program, it will fail treatment, and prevention will become a health problem. The patient's behavior in taking medication also plays an important role in breaking the transmission to the community and the impacts that arise for the patient.
The Health Belief Model (HBM) theory states that changes in individual behavior in taking action to improve health status are influenced by factors such as susceptibility to disease, perceived severity or seriousness of the illness, perceived benefits, perceived costs or barriers, and cues to action obtained from personal interactions such as family and also other supporting factors such as community leaders.9
The transmission source is a positive AFB-TB patient, which can transmit to other people around them, especially close contact when coughing or sneezing; the patient spreads into the air in the form of droplets (splashes, phlegm). People around will be infected if inhaled into the breath.10
MethodStudy designThe research design used in this study was a case-control where the population was all patients who visited and recorded medical records in the active region of Polonia Health Center Medan. The case sample was some 68 cases of pulmonary TB and 68 controls. The study aimed to analyze the risk factors for non-adherence to TB patients taking medication at the Polonia Health Center. This analysis is used to see the most influential factors. In this study, there are five independent variables which are numeric/continuous, while the dependent variable is categorical. Therefore, the appropriate multivariate analysis to analyze the data is to use the logistic regression test.
Data types and sourcesData collected from the sample are demographic data, including age, gender, and occupation,
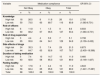
ResultCharacteristics of respondentsBased on Table 1, it is found that in general, respondents aged 15–24 years are 35 people (25.7%), and at least 65–74 years are six people (4.4%), while the male gender is 76 people. (9 55.9%) greater than women as many as 60 people (44.1%) and based on the occupation of the respondents generally do not work, namely 51 people (37.5%) and at least as fishermen, namely five people (3.7%).
Distribution of respondents based on the characteristics of respondents.
| Characteristics of respondents | ||
|---|---|---|
| Age group (year) | Frequency (n) | % |
| 15–24 | 35 | 25.7 |
| 25–34 | 33 | 24.3 |
| 35–44 | 31 | 22.8 |
| 45–54 | 19 | 14.0 |
| 55–64 | 12 | 8.8 |
| 65–74 | 6 | 4.4 |
| Gender | ||
| Men | 76 | 55.9 |
| Women | 60 | 44.1 |
| Occupation | ||
| Housewife | 51 | 37.5 |
| Civil Servant | 12 | 8.8 |
| Entreoreneur | 35 | 25.7 |
| Farmer | 18 | 13.2 |
| Fisherman | 5 | 3.7 |
| Labor | 8 | 5.9 |
| Student | 7 | 5.1 |
| Total | 136 | 100.0 |
Non-adherence to treatment by not participating in the DOTS program for 6–8 months and not taking medication every day as many as eight items, not taken at once, is considered not to have participated in the pulmonary TB treatment program with the correct DOTS strategy.11 The risk factors for non-adherence to pulmonary TB patients taking medication, based on the results of statistical analysis, were obtained as follows (Table 2).
The relationship between knowledge risk factors, the role of officers, the role of drug supervisor, side effects of drugs, duration of taking medication, feeling healthy towards non-adherence to taking medication at Polonia Health Center Medan.
| Variable | Medication compliance | OR 95% CI | |||||
|---|---|---|---|---|---|---|---|
| Not Obey | Obey | Total | |||||
| n | % | n | % | n | % | ||
| Knowledge | |||||||
| High risk | 18 | 26.5 | 8 | 11.8 | 26 | 19.1 | 2.700 |
| Low risk | 50 | 73.5 | 60 | 89.7 | 110 | 80.9 | (1.083-6.731) |
| Role of officers | |||||||
| High risk | 6 | 11.8 | 1 | 1.5 | 9 | 6.6 | 8.933 |
| Low risk | 60 | 88.2 | 67 | 96.5 | 127 | 93.4 | (1.083–6.731) |
| Role of drug supervisor | |||||||
| High risk | 3 | 4.4 | 4 | 5.9 | 7 | 5.1 | 0.738 |
| Low risk | 65 | 95.6 | 64 | 94.1 | 129 | 94.9 | (0.159–3.432) |
| Side effects of drugs | |||||||
| High risk | 24 | 35.3 | 5 | 7.4 | 29 | 21.3 | 6.873 |
| Low risk | 44 | 64.7 | 63 | 92.6 | 107 | 78.7 | (2.435–19.398) |
| Duration of taking medication | |||||||
| High risk | 5 | 7.4 | 10 | 14.7 | 15 | 11.0 | 0.460 |
| Low risk | 63 | 92.6 | 58 | 85.3 | 121 | 89.0 | (0.149–1.427) |
| Feeling healthy | |||||||
| High risk | 12 | 17.6 | 3 | 4.4 | 15 | 11.0 | 4.643 |
| Low risk | 56 | 82.4 | 65 | 95.6 | 121 | 89.0 | (1.247–17.287) |
| Total | 68 | 100.0 | 68 | 100.0 | 136 | 100.0 | |
Based on Table 3, the logistic regression analysis of the bivariate variables included in the logistic regression analysis shows that the role of health workers that has the most influence on non-compliance with TB patients taking medication is 58.416 times. The side effect variable for drugs is 33.702, and the variable feels healthy 29.208 times. Knowledge 15.556 times. So the less knowledge there are, the more patients who do not comply with taking anti-tuberculosis drugs at Polonia Health Center Medan in 2020.
Selection of variables that become model candidates in logistics regression test based on bivariate analysis.
| Variable | B | p value | Exp(B)OR | 95%CI Exp(B) |
|---|---|---|---|---|
| Knowledge | 2.774 | 0.000 | 15.556 | 4.919–49.198 |
| Role of health workers | 4.068 | 0.000 | 58.416 | 6.320–539.922 |
| Side effect of drugs | 3.518 | 0.000 | 33.702 | 9.689–117.229 |
| Feeling healthy | 3.374 | 0.000 | 29.208 | 6.573–129.786 |
| Constant | −25.420 | 0.000 | 0.000 |
Knowledge is the result of knowing, and this occurs after people sense a specific object; from experience and research, it is proven that behavior based on knowledge will be more lasting than behavior that is not based on knowledge.12
Based on the results of the logistic regression test, the OR value of the knowledge variable was 2.700 with a significant level of p=0.029<0.05 (95% CI; 1.083–6.731), because the OR value >1, the lower and upper limit CIs did not include the value 1, meaning that the knowledge of TB patients is a risk factor for non-adherence to patients taking medication at the Polonia Health Center. So it can be concluded that there is an effect of patient knowledge in taking anti-tuberculosis drugs at Polonia Health Center Medan in 2020.
Good knowledge will affect personal attitudes and actions to comply with treatment which will support the patient's healing process. The higher the level of personal knowledge about the understanding of TB, the symptoms or signs of TB disease, the causes of TB disease, and the consequences of non-adherence to taking medication, it will enable the patient to carry out treatment according to the instructions given by the doctor. Knowledge can be obtained from various sources and references, not only through formal education.13
The role of health workers’ support for pulmonary TB patients can increase awareness, willingness, and role in treatment, which pulmonary TB patients highly expect to raise the spirit of life to undergo the healing process. Motivation and support by people who are considered to understand the disease they are suffering from foster a sense of trust and strength to follow the procedures and recommendations given to follow medication adherence so that germs or bacteria Mycobacterium Tuberculosis can be treated. Based on multiple logistic regression analysis, the OR value was 8.933 with (5% CI 1.085–73.525, which means that the role of officers is a risk factor for non-compliance with TB patients taking medication. The relationship between health workers will establish effective communication both to TB patients and their families so that it will be easier to recognize the emotional needs of Tuberculosis patients so that Tuberculosis patients feel their emotional needs are fulfilled.14 The Odds Ratio value of the role of health workers is 8.933, indicating that if the officers are less involved, the respondent is at risk for non-adherence to taking medication compared to if the officers play an active role. Failure in TB treatment is due to the lack of motivation of doctors and other health workers in providing the services needed by pulmonary TB sufferers; this happens because the officers feel that if they want to recover, the patient is the one who is more active in seeking treatment related to the disease they are suffering, even though not all patients knowing TB disease correctly and the existing treatment program at the health center, for this reason, the role of the officer is very much needed to disseminate information related to TB disease and treatment management and the impact of the drug is interrupted.15
The role of the drug-taking supervisor is aimed at ensuring more regularity in treatment. This is also to ensure the smooth continuity of the pulmonary TB eradication program. The effectiveness of healing will occur if the medication supervisor can monitor continuously to avoid drug withdrawal which can lead to resistance in the patient. The DOTS strategy will provide comprehensive oversight. Drugs supervisors will encourage patients to undergo treatment regularly, and this is because the support provided is used as a driving force for patients in carrying out a therapy program.16
Drug side effects are other signs that sufferers feel due to taking anti-tuberculosis drugs, which are symptoms of drug administration. Complaints of side effects that often occur in patients include pain, nausea, abdominal pain, joint pain, tingling, skin redness, itching, and severe side effects such as respiratory syndrome (shortness of breath), shock, kidney failure, and redness of the skin, deafness, jaundice, without other causes, and other disorders.5 Based on multiple logistic analyses, the Odds Ratio value was 6.873 with a significant level of p=0.000<0.05 (95% CI; 2,435–19,398, so the drug side effect variable is a risk factor for non-compliance with taking medication for pulmonary TB patients at Polonia Health Center Medan. Drug side effects can occur in a person because it is a factor in the body's response to any foreign objects that enter, causing unwanted symptoms or reactions.12 Symptoms that arise cause the patient's non-compliance to drink and stop continuing his treatment because the patient thinks the complaints are getting worse. Monitoring can be done to avoid drug side effects by explaining the signs of side effects during treatment.
Pulmonary TB patients require a prolonged treatment time because it is a chronic disease, which is 6–8 months, causing boredom for pulmonary TB patients, and eventually, non-adherence to treatment can occur. Based on the multiple logistic tests, the Odds Ratio value was 0.450 with a significant level of p=0.171>0.05 (95% CI: 0.149–1.427). OR<1 and 95% CI, the lower and upper limits include a value of 1, meaning that the variable duration of taking medication is not a risk factor for non-adherence to taking medication at Polonia Health Center Medan. Respondents who took medication for a long time were at risk but still took as many as 10 (14.7%) people. This is because patients who have been taking medication for a long time have begun to realize that they need to take medication regularly so that they are no longer interrupted, which of course, has to start from the beginning of treatment and can cause difficult resistance to the use of other drugs.
When patients take anti-tuberculosis drugs, some germs die, and some are still dormant. The impact of anti-tuberculosis drugs will cause changes in a good direction, and some even feel that they are starting to improve and even feel healthy or recover, especially in the first 2 months so that patients stop treatment. This situation is undoubtedly very disturbing adherence to taking medication so that success in undergoing the DOTS program is interrupted and can lead to resistance of germs to anti-tuberculosis drugs.16
Multiple lk is the result of the Odds Ratio value of 4.643 with a significant level of p=0.014<0.05 (95% CI; 1.247–17.297). Based on this analysis, the variable feeling healthy is a risk factor for non-compliance with pulmonary TB patients taking medication at the Polonia Health Center in Medan.17
The multivariate logistic regression test analysis results showed that the role of health workers who were most at risk for non-adherence to TB patients taking medication with an Odds ratio was 58,416 with P=0.000<0.005 (95% CI; 9,689–117,229). This is the role of health workers to change patients’ behavior, especially in motivating and monitoring regularity in taking medication. For officers who are not active, regularity in taking medication is also not appropriately monitored.5
ConclusionThe knowledge of respondents who lacked the risk of non-adherence to taking medication was 2,700 times greater than respondents with sufficient knowledge. The role of health workers in non-adherence to taking medication is 8.933 times greater than respondents who experience drug side effects and have a 6.873 times greater risk of non-adherence to taking medication than those who do not experience drug side effects. The role of the drug supervisor is not at risk of non-adherence to taking medication with an OR of 0.738. The duration of taking medication is not at risk for non-adherence to taking medication with an OR of 0.460. Respondents who feel healthy have a risk of not complying with taking medication 4.643 times greater than patients who feel healthy.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.