The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosThis study aimed to analyze serum levels of L-arginine and 25-hydroxyvitamin D as predictors of survival in severely preeclamptic women.
MethodsThis study is a retrospective descriptive study using medical record data from June to August 2019 and has received a recommendation for ethical approval with the protocol number UH20070290. The study was conducted in 4 hospitals in Makassar: Dr. General Hospital. Wahidin Sudirohusodo, Hasanuddin University Teaching Hospital, Siti Fatimah Regional Mother and Child Health Hospital, and Sitti Khadijah 1 Mother and Child Hospital. The samples of this study were mothers who gave birth with a diagnosis of normal pregnant women, severe preeclampsia, and severe preeclampsia with complications.
ResultsSerum l-arginine level did not affect the survival of severe preeclamptic mothers. It was shown at p-value 0.799>0.05. Meanwhile, serum levels of 25-hydroxyvitamin D affect the predictors of maternal preeclampsia where the p-value is 0.024<0.05. In comparing serum levels of L-arginine and 25-hydroxyvitamin D, there was no significant difference in groups of normal pregnant women, severe preeclampsia, and severe preeclampsia with complications.
ConclusionSerum level of 25-hydroxyvitamin affects the survival of severe preeclamptic mothers.
Preeclampsia is an obstetric problem that cannot be resolved comprehensively in the world, likewise in Indonesia. Major complications in pregnancy are due to hypertensive disease in pregnancy, including gestational hypertension, preeclampsia (PE), and eclampsia, and accounted for 14% of maternal mortality.1
Preeclampsia is a particular symptom in pregnancy marked with high blood pressure and proteinuria after 20 weeks, occurring in 8% of pregnant women.2 The cause of preeclampsia until now is not known. Severe preeclampsia experienced by pregnant women does not occur by itself. Many risk factors can affect the incidence of severe preeclampsia: Mother's age, parity, gestational age, number of children, the number of ANC visits, and the History of Hypertension.3
Protective effects for preeclampsia are probably best if vitamin L-arginine and antioxidants are added before the 24-week gestation age.4 Vitamin D mother is low during pregnancy, and preeclampsia incidence suggests that vitamin deficiency can be an independent risk factor for preeclampsia. The damage or dysfunction of endothelial cells appears to be the basic pathophysiological event of the maternal vascular system in women with preeclampsia.5
Several studies reported statistical significance between L-arginine supplementation and nitric oxide levels in women with preeclampsia. The study also showed an increase in nitric oxide levels in the blood after L-arginine supplementation, and these women had a lower chance of developing preeclampsia than those who did not receive L-arginine supplementation. This study demonstrated the specificity of nitric oxide as a marker of the development of preeclampsia.6 Several studies have found that vitamin D is associated with preeclampsia as evidenced by research7 Low maternal and placental calcium levels in preeclampsia. These changes may be associated with some dysfunction in the mother and placental compartment, including deregulation of the immune system, characterized by high levels of pro-inflammatory cytokines in preeclampsia. Therefore, vitamin D supplementation has been suggested to reduce the incidence of preeclampsia. Therefore, the background of this research is still rarely found in publications in Indonesia. Therefore, based on the above problems, it is necessary to research the analysis of serum L-arginine levels and serum 25-hydroxyvitamin D levels as predictors of survival for mothers and infants with severe preeclampsia and compare serum levels of L-arginine and 25-hydroxyvitamin D in the mother group. Normal pregnancy, severe preeclampsia, and severe preeclampsia with complications.
MethodsThis research is a secondary data study (medical record data). In this study, the researchers wanted to analyze serum levels L-arginine and 25-hydroxyvitamin D as a predictor of survival of severe preeclampsia mothers. In addition, it also analyzed comparisons of serum levels L-arginine and serum levels of 25-hydroxyvitamin D in normal pregnant women, severe preeclampsia, and preeclampsia with complications.
Research time and placeMedical records were taken from June 2019–August 2019. The research was conducted in 4 hospitals in Makassar, including Dr. Wahidin Sudirohusodo General Hospital, Hasanuddin University Education Hospital, Sitti Khadijah 1 Mother and Child Hospital, Sitti Fatimah maternal and child health hospital.
Data collection techniquesThis study is a descriptive retrospective study using medical record data by reviewing patient characteristics, treatment rooms, and supplements. In addition, other supporting data are serum levels L-arginine and 25-hydroxyvitamin D in a sample group of normal pregnant women, severe preeclampsia, and severe preeclampsia with complications. The data were analyzed using statistical analysis with survival analysis statistics test and one-way Anova test.
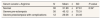
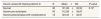
ResultsThe number of samples in this study was 72 samples. The serum l-arginine level in severe preeclampsia was greater than the significance level of 0.799 (P>0.05), which means that the serum l-arginine level had no significant effect on the survival time of the mother with severe preeclampsia. While the serum level of 25-hydroxyvitamin D has a value that is smaller than the significance level of 0.024 (P>0.05) so that the serum level of 25-hydroxyvitamin D affects the survival duration of severe preeclampsia (Table 1). In contrast, the comparison of L-arginine and 25-hydroxyvitamin D serum levels in normal pregnant women (Table 2 and Table 3), severe preeclampsia, and severe preeclampsia with complications showed results where the P value >0.05 with the conclusion that there was no significant difference between the three sample groups with serum levels of L-arginine and 25-hydroxyvitamin D.
Arginine is considered an unnecessary amino acid in many species, including humans. However, in specific physiological (growth, pregnancy) or pathophysiological conditions with certain conditions, arginine is required in preterm birth; sepsis and diabetes can cause arginine to be necessary. Usually, these conditions can benefit from exogenous arginine supplementation because this amino acid is required for NO, creatine, polyamine, and protein synthesis.8
L-arginine is categorized as a semi-essential amino acid; under normal circumstances, the body can meet its needs by synthesizing L-arginine, but in pregnant conditions, the need for L-arginine will increase.9 L-arginine is the most important source in the regulation of nitric oxide so that in pregnancy, there will be a period of increased deposition in maternal and fetal tissues so that increased NO synthesis is needed to be a major contributor to maternal vascular expansion in pregnancy and blood flow to the placenta. This makes the need for L-arginine to be an essential amino acid in pregnant women.9
Vitamin D is a fat-soluble vitamin that plays a significant role in bone mineralization. However, low levels of vitamin D have been linked to osteoporosis and coronary artery disease, diabetes, obesity, and cancer. In pregnancy, vitamin D status is important for the health of both mother and fetus. Low serum vitamin D during pregnancy results in poor fetal bone mineralization at 19 weeks gestation.10
In pregnancy, vitamin D is needed by the body. In general, the need for vitamin D is not only for pregnant women but also for the general population, namely ≥50nmol/L (or 20ng/mL). Pregnant women who have decreased levels of vitamin D≤50nmol/L serum 25-(OH) D have the potential to experience hypertension, immunological disorders (regulation of cytokines and immunoglobins), and differentiation of proliferative cells (gene regulation), which underlie the occurrence of preeclampsia, namely if there is a decrease in placental growth factor concentrations and there is endothelial dysfunction.7
During pregnancy, deficiencies of vitamins and minerals, collectively known as micronutrients, can have significant adverse effects on maternal and birth outcomes. Evidence-based nutrition interventions could make a difference and could potentially avoid this outcome. Iron supplementation has been shown to increase the average hemoglobin concentration of the mother over a period of time and reduce the risk of anemia. Zinc supplementation has been shown to result in small but significant reductions in preterm birth.7
Meanwhile, this study is in line with the research (Amran and Faruk, 2015) with the research title Non-parametric survival model in Diarrhea Patient Hospital Data at Indralaya Public Health Center, and this study is looking for an estimate of the survival function and the estimation of the hazard function, the results are obtained. On the 4th day, the lowest hospitalization was h (4)=0.0357, while the highest chance was on the 15th day. Two types of testing were carried out in this study, namely simultaneous covariate contribution testing and partial testing. Based on the simultaneous test, if all covariates are entered together, the effect on the survival time of all covariates is not significant. Meanwhile, in the partial test, when the other covariates were deemed not influential, only the covariate of private occupation and moderate-severe disease status had a significant effect on survival time.11
In addition, this research is also in line with research from Qomaria, Fatekurohman, and Qomaria et al. (2019) with the research title Cox Proportional Hazard Model Application for Stroke Patients at RSD Balung, Jember Regency using the compilation of a proportional hazard cox model preceded by a proportional hazard assumption test and followed by selecting the best model using backward elimination and selecting the model that has the smallest AIC value. Finally, the hazard ratio interpretation is carried out from the best model. The result: Increasing age, the risk of death will increase by 1.2094 times. Patients who do not have comorbidities with DM have a risk of death 0.6175 times less than patients who have DM comorbidities. Patients with hemorrhagic stroke had a risk of death 3.0178 times greater than patients with ischemic stroke.12
ConclusionSerum L-arginine level does not affect the survival duration of severe preeclamptic mothers, while serum 25-hydroxyvitamin D levels affect the survival duration of severe preeclamptic mothers. There was no significant difference between serum levels of L-arginine and 25-hydroxyvitamin D in each group with normal pregnancy status, severe preeclampsia, and severe preeclampsia with complications. However, the mean low serum L-arginine levels were found in severely preeclamptic women with complications, while insufficient serum 25 hydroxyvitamin D levels were found in the group of normal pregnant women.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.