To determine whether the probability of having heard about human papillomavirus (HPV) vaccination differs by socio-demographic characteristics among Colombian women; and whether the effect of predictors of having heard about HPV vaccination varies by educational levels and rural/urban area of residence.
MethodsData of 53,521 women aged 13–49 years were drawn from the 2010 Colombian National Demographic and Health Survey. Women were asked about aspects of their health and their socio-demographic characteristics. A logistic regression model was used to identify factors associated with having heard about HPV vaccination. Educational level and rural/urban area of residence of the women were tested as modifier effects of predictors.
Results26.8% of the women had heard about HPV vaccination. The odds of having heard about HPV vaccination were lower among women: in low wealth quintiles, without health insurance, with subsidized health insurance, and those who had children (p<0.001). Although women in older age groups and with better education had higher probabilities of having heard about HPV vaccination, differences in these probabilities by age group were more evident among educated women compared to non-educated ones. Probability gaps between non-educated and highly educated women were wider in the Eastern region. Living in rural areas decreased the probability of having heard about HPV vaccination, although narrower rural/urban gaps were observed in the Atlantic and Amazon-Orinoquía regions.
ConclusionsAlmost three quarters of the Colombian women had not heard about HPV vaccination, with variations by socio-demographic characteristics. Women in disadvantaged groups were less likely to have heard about HPV vaccination.
Determinar si la probabilidad de haber oído sobre la vacunación contra el virus del papiloma humano (VPH) varía según características socio-demográficas de las mujeres colombianas; y si el efecto de estos predictores varía según nivel de educación y el área rural/urbana de residencia.
MétodosDatos de 53.521 mujeres entre 13 y 49 años fueron extraídos de la Encuesta Nacional de Demografía y Salud de Colombia, 2010. Se preguntó a las mujeres acerca de su salud y sus características socio-demográficas. Se utilizó un modelo de regresión logística para identificar los factores asociados con haber oído sobre la vacunación contra el VPH. Se evaluó si el nivel educativo y el área rural/urbana de residencia interactuaban con los predictores.
Resultados26,8% de las mujeres había oído sobre la vacunación contra el VPH. Las probabilidades de haber oído sobre la vacunación contra el VPH fueron más bajas en las mujeres de quintiles de riqueza bajos, sin seguro de salud, con seguro de salud subsidiado, y en aquéllas que tenían hijos (p<0,001). A pesar de que las mujeres mayores y con mejor educación tenían una mayor probabilidad de haber oído sobre la vacunación contra el VPH, las diferencias en las probabilidades por grupos de edad fueron más evidentes entre las mujeres con educación comparadas con aquéllas sin educación. Las brechas en las probabilidades entre las mujeres sin educación y las altamente educadas fueron mayores en la región Oriental. Vivir en zonas rurales disminuyó la probabilidad de haber oído sobre la vacunación contra el VPH, aunque las diferencias rural/urbana fueron menos amplias en las regiones Atlántica y de la Amazonía-Orinoquía.
ConclusionesCasi tres cuartas partes de las mujeres colombianas no habían oído sobre la vacunación contra el VPH, con variaciones según sus características socio-demográficas. Las mujeres de grupos desfavorecidos tenían menos probabilidades de haber oído acerca de la vacunación contra el VPH.
Cervical cancer (CC) is responsible for over 275,000 female deaths each year, with more than 500,000 new cases diagnosed worldwide.1 Persistent infection of the anogenital tract with high-risk human papillomavirus (HPV), which is a sexually transmitted disease,2 has been established as a necessary cause for cervical intraepithelial neoplasia and cervical cancer.3,4 Factors such as being sexually active, young age, oral contraceptive use, socioeconomic status, high parity, smoking status, and previous HPV infections, among others have been associated with the transmission of HPV.2
Vaccination against certain high-risk HPV types among women without previous exposure to these viruses and ideally before their sexual debut has been associated with a reduction of pre-invasive cervical lesions.2,5 HPV vaccination provides a potential cost-effective way to prevent CC.6 Currently, two vaccines are available against HPV: the bivalent vaccine protects against HPV types 16 and 18; the quadrivalent one protects against HPV types 6, 11, 16, and 18.5 Awareness of prevention of CC is key to support HPV vaccination7 and raising knowledge about the role of HPV in the development of CC is central improve in CC prevention.8 Previous studies have shown that a lower intention of HPV vaccination is associated with limited awareness and poor knowledge of HPV vaccination.7,9,10 Therefore, measuring awareness of HPV vaccination is critical for CC prevention programs.
In Colombia, CC is the cancer most frequently affecting women.11,12 It has been estimated that about 15% of Colombian women will develop a HPV infection during their lifetime.12 The Colombian Instituto Nacional de Vigilancia de Medicamentos y Alimentos (INVIMA) approved the quadrivalent and bivalent HPV vaccines in 2006 and 2007, respectively;13 then, the HPV vaccines were available for women who were willing to pay for them. The quadrivalent HPV vaccine is an insured service for girls aged 9 years and older since 2012.14 However, a lack of knowledge about HPV infection and HPV vaccination has been reported in Colombia, especially among less educated and low income groups.8,15 Indeed, these disadvantaged groups have been highly affected by the structure of the Colombian Sistema General de Seguridad Social en Salud (SGSSS), which is an insurance-based health care system.16 This system has increased barriers to access health care16 and obtain equal health benefits for individuals unable to pay (subsidized health insurance)16,17 compared to those who can contribute to the system (contributory health insurance)16,18 and those who belong to groups with special health care plans (public teachers, workers of public universities, military forces, police, and employees of the Colombian Oil Company).19
To the best of our knowledge, there are no nationwide studies in Colombia evaluating socioeconomic and personal factors associated with having heard about HPV vaccination among women. Therefore, our objectives were to determine: (1) the prevalence of Colombian women having heard about HPV vaccination; (2) whether the probability of having heard about HPV vaccination differs by age group, educational level, socioeconomic (wealth quintile) and working status, type of health insurance, region and rural/urban area of residence, women having experienced intercourse, type of contraceptive method used, and women who have had children; and (3) whether the effect of predictors for having heard about HPV vaccination differs at different educational levels and rural/urban area of residence.
MethodsThe data were drawn from the 2010 National Demographic and Health Survey (NDHS), a national representative survey conducted among women between 13 and 49 years old living in Colombia. In total, 53,521 out of 56,886 women participated in the NDHS (response rate=94%).20 This survey evaluated socio-demographic characteristics of participants, as well as different aspects of their health.
All women were asked whether they had heard about the HPV and also if they had ever heard about a vaccine to prevent CC. Women who reported having heard about HPV and having heard about a vaccine to prevent CC were classified as “1=have heard about HPV vaccination;” otherwise, they were classified as “0=have not heard about HPV vaccination.” This was the dependent variable of our study. Self-reported factors considered as independent variables in the study were age group, educational level, wealth quintile, working status, type of health insurance, having experienced intercourse, type of contraceptive method used, having children, and region and rural/urban area of residence. Atlantic, Amazon-Orinoquía, Central, Eastern, and Pacific were the regions established in the Colombian NHDS; Bogotá (the capital) was included in the Eastern region. Chi-square tests were performed to test differences in the distribution of women in different categories of the independent variables.
A logistic regression model was built using the manual backward method at a 5% level of significance. Variables not included in the model were tested as confounders; the presence of confounding was considered if these variables changed the parameter estimates of predictors in the model by more than 10%. Additionally, educational level and rural/urban area of residence were tested as modifier effects.
Unadjusted (UORs) and adjusted odds ratios (AORs), 95% confidence intervals (95% CIs), and p-values were computed. Women with missing data were excluded from the multivariable analysis. Model diagnostics were examined through receiver-operating characteristic (ROC) curves and assessment of residuals. The analyses were performed using SAS software version 9.3 (SAS Institute Inc., Cary, NC, USA).
The Ethical Committee of the Asociación Probienestar de la Familia Colombiana (Profamilia) provided ethical approval for the 2010 NDHS; participants gave their consent before the administration of the survey. To use the 2010 NDHS data for the present study, the University of Saskatchewan Research Ethics Board provided an exception for ethics review.
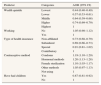
ResultsIn total, data from 53,521 women aged 13–49 years were obtained. The mean age of the women was 29.2 years (SD=10.8). The distribution of women's characteristics is presented in Table 1. Of the total women, 14,363 (26.8%, 95% CI 26.3–27.1%) reported having heard about HPV vaccination. The proportion of women who heard about HPV vaccination by age group was: 13–18 years, 12.9% (95% CI 11.4–14.4%); 19–24 years, 16.6% (95% CI 15.1–18.1%); 25–32 years, 23.9% (95% CI 22.5–25.3%); 33–40 years, 21.7% (95% CI 20.3–23.1%); and 41–49 years, 24.9% (95% CI 23.5–26.3%). Among the 14,363 women who have heard about HPV vaccination, 49% had secondary education, 23.9% belonged to the highest wealth quintile, 83.8% were working, 50.7% had contributory health insurance, 84.2% were living in urban areas, 27.4% lived in the Eastern region, 88% had experienced intercourse, 38.7% were not using contraceptive methods, and 67.4% had children. Statistically significant differences were found when comparing socio-demographic and sexual factors among women who had heard about HPV vaccination and those who had not. Bivariate analyses indicated that all the predictors were significantly associated with the dependent variable (p-values<0.001); UORs and their 95% CI are shown in Table 1.
Descriptive statistics for variables used in the model building, unadjusted odds ratios (UOR) and corresponding 95% confidence intervals (CI). National Demographic and Health Survey (NDHS), Colombia, 2010 (n=53,521).
| Variable | Categories | All womena | Have heard about human papillomavirus vaccinationa,b | UOR (95% CI) | |
|---|---|---|---|---|---|
| No (39,158) | Yes (14,363) | ||||
| Age group | 41–49 years old | 10,736 (20.1) | 7164 (18.3) | 3572 (24.9) | 2.61 (2.45–2.79) |
| 33–40 years old | 10,207 (19.1) | 7089 (18.1) | 3118 (21.7) | 2.31 (2.16–2.46) | |
| 25–32 years old | 11,513 (21.5) | 8075 (20.6) | 3438 (23.9) | 2.23 (2.10–2.38) | |
| 19–24 years old | 9508 (17.7) | 7124 (18.2) | 2384 (16.6) | 1.76 (1.64–1.88) | |
| 13–18 years old | 11,557 (21.6) | 9706 (24.8) | 1851 (12.9) | 1 | |
| Educational level | None | 1145 (2.1) | 997 (2.6) | 148 (1.0) | 0.15 (0.13–0.18) |
| Primary | 13,550 (25.3) | 11,524 (29.4) | 2026 (14.1) | 0.18 (0.17–0.19) | |
| Secondary | 28,393 (53.1) | 21,357 (54.5) | 7036 (49.0) | 0.34 (0.32–0.35) | |
| Higher | 10,433 (19.5) | 5280 (13.5) | 5153 (35.9) | 1 | |
| Wealth quintile | Lowest | 13,203 (24.7) | 11,507 (29.4) | 1696 (11.8) | 0.15 (0.14–0.17) |
| Lower | 13,642 (25.5) | 10,608 (27.1) | 3034 (21.2) | 0.30 (0.28–0.32) | |
| Middle | 11,001 (20.6) | 7908 (20.2) | 3093 (21.5) | 0.41 (0.38–0.43) | |
| Higher | 8662 (16.2) | 5554 (14.2) | 3108 (21.6) | 0.58 (0.55–0.62) | |
| Highest | 7013 (13.1) | 3581 (9.2) | 3432 (23.9) | 1 | |
| Working status | No | 12,061 (22.5) | 9729 (24.8) | 2332 (16.2) | 0.59 (0.56–0.62) |
| Yes | 41,460 (77.5) | 29,429 (75.2) | 12,031 (83.8) | 1 | |
| Type of health insurance | Non-affiliated | 6180 (11.5) | 4739 (12.1) | 1441 (10.0) | 0.44 (0.42–0.48) |
| Subsidized | 27,970 (52.3) | 22,864 (58.4) | 5106 (35.6) | 0.33 (0.31–0.34) | |
| Special | 1454 (2.7) | 917 (2.3) | 537 (3.7) | 0.86 (0.77–0.96) | |
| Contributory | 17,917 (33.5) | 10,638 (27.2) | 7279 (50.7) | 1 | |
| Area of residence | Rural | 14,636 (27.3) | 12,366 (31.6) | 2270 (15.8) | 0.41 (0.39–0.43) |
| Urban | 38,885 (72.7) | 26,792 (68.4) | 12,093 (84.2) | 1 | |
| Region | Atlantic | 11,474 (21.4) | 8322 (21.3) | 3152 (21.9) | 0.79 (0.74–0.83) |
| Amazon-Orinoquía | 9117 (17.0) | 7826 (20.0) | 1291 (9.0) | 0.34 (0.32–0.37) | |
| Central | 13,096 (24.5) | 9197 (23.5) | 3899 (27.1) | 0.88 (0.83–0.93) | |
| Pacific | 7737 (14.5) | 5651 (14.4) | 2086 (14.5) | 0.77 (0.72–0.82) | |
| Eastern | 12,097 (22.6) | 8162 (20.8) | 3935 (27.4) | 1 | |
| Had experienced intercourse | Yes | 44,249 (82.7) | 31,607 (80.7) | 12,642 (88.0) | 1.76 (1.66–1.86) |
| No | 9272 (17.3) | 7551 (19.3) | 1721 (12.0) | 1 | |
| Contraceptive method | Condoms | 3633 (6.8) | 2440 (6.2) | 1193 (8.3) | 1.60 (1.48–1.73) |
| Hormonal methods | 8866 (16.6) | 6305 (16.1) | 2561 (17.8) | 1.33 (1.26–1.40) | |
| Female sterilization | 11,790 (22.0) | 8330 (21.3) | 3460 (24.1) | 1.36 (1.29–1.43) | |
| Other methods | 5491 (10.3) | 3898 (10.0) | 1593 (11.1) | 1.34 (1.25–1.43) | |
| Not using | 23,741 (44.4) | 18,185 (46.4) | 5556 (38.7) | 1 | |
| Have had children | Yes | 35,126 (65.6) | 25,439 (65.0) | 9687 (67.4) | 1.12 (1.07–1.16) |
| No | 18,395 (34.4) | 13,719 (35.0) | 4676 (32.6) | 1 | |
In the model building, age was found to be not linearly related to the log odds of the outcome (p<0.001); therefore, it was included as a five-category variable which was created according to age distribution. Working status and having experienced intercourse were variables initially removed from the model (p-values>0.05); notwithstanding, working status was found to be a confounding variable and was included as a covariate in the model. Also, significant interactions were found between educational level and age group (p=0.002), educational level and region (p<0.001), and rural/urban area of residence and region (p<0.001).
Table 2 presents AORs and their corresponding 95% CIs of predictors not interacting in the logistic regression model. Regarding wealth quintile, women in the lowest (AOR=0.44, 95% CI 0.40–0.49) and lower (AOR=0.57, 95% CI 0.53–0.61) quintiles were less likely to have heard about HPV vaccination in comparison to women from the highest quintile. Similarly, women in the middle (AOR=0.64, 95% CI 0.59–0.68) and higher (AOR=0.74, 95% CI 0.69–0.79) wealth quintiles were less likely to have heard about HPV vaccination. The type of health insurance was also significantly associated with having heard about HPV vaccination. Women with subsidized health insurance (AOR=0.69, 95% CI 0.66–0.73) and those non-affiliated to any health insurance (AOR=0.73, 95% CI 0.68–0.79) were less likely to have heard about HPV vaccination than women in the contributory group. Women using condoms (AOR=1.19, 95% CI 1.10–1.29), hormonal methods (AOR=1.20, 95% CI 1.13–1.28), or who were sterilized (AOR=1.10, 95% CI 1.03–1.17) were more likely to have heard about HPV vaccination than those not using any contraceptive method. Furthermore, women with children were less likely to have heard about HPV vaccination compared to women with no children (AOR=0.87, 95% CI 0.81–0.92).
Adjusted odds ratio (AORs) and corresponding 95% confidence intervals (CI) of having heard about human papillomavirus vaccination by non-interacting predictors (n=53,520). National Demographic and Health Survey (NDHS) Colombia, 2010.
| Predictor | Categories | AOR (95% CI) |
|---|---|---|
| Wealth quintile | Lowest | 0.44 (0.40–0.49) |
| Lower | 0.57 (0.53–0.61) | |
| Middle | 0.64 (0.59–0.68) | |
| Higher | 0.74 (0.69–0.79) | |
| Highest | 1 | |
| Working | No | 1.05 (0.98–1.12) |
| Yes | 1 | |
| Type of health insurance | Non-affiliated | 0.73 (0.68–0.79) |
| Subsidized | 0.69 (0.66–0.73) | |
| Special | 0.91 (0.81–1.02) | |
| Contributory | 1 | |
| Contraceptive method | Condoms | 1.19 (1.10–1.29) |
| Hormonal methods | 1.20 (1.13–1.28) | |
| Female sterilization | 1.10 (1.03–1.17) | |
| Other methods | 1.05 (0.97–1.13) | |
| Not using | 1 | |
| Have had children | Yes | 0.87 (0.81–0.92) |
| No | 1 |
Predictors interacting in the model are depicted in Figs. 1–3. The probabilities of having heard about HPV vaccination were higher among older age groups and women with better levels of education; however, differences in these probabilities by age group were more evident among educated women compared to non-educated ones (Fig. 1). Comparing the level of education by region (Fig. 2), it was observed that women with no education had the lowest probabilities of having heard about HPV vaccination in all regions, and that the probability gap between these women and the highly educated ones was wider in the Eastern than in the Amazon-Orinoquía region. Also, among women with high educational levels, those living in the Amazon-Orinoquía region had the lowest probability of having heard about HPV vaccination; however, highly educated women of the Amazon-Orinoquía region were more likely to have heard about vaccination than those with lower levels of education in any other region. Furthermore, women living in rural areas had lower probabilities of having heard about HPV than those living in urban areas (Fig. 3); notwithstanding, women living in urban areas of the Amazon-Orinoquía region had similar probabilities than those living in rural areas of the Eastern region. Also, narrower gaps between women in rural and urban areas were observed in the Atlantic and Amazon-Orinoquía regions.
In the model diagnostics, the ROC curve showed that the logistic model correctly classified 72.5% of the women who had heard about HPV vaccination, which could be considered as satisfactory. Also, the assessment of residuals showed that they were within an adequate range of ±3 standard deviations from zero.
DiscussionThe low prevalence of women who had heard about HPV vaccination found in our results is in accordance with a previous study claiming a poor awareness of HPV vaccination among adolescents in Cartagena, Colombia.21 This lack of awareness of HPV vaccination in the country could be resulting from poor national “HPV educational efforts”.8 Other authors in Colombia have reported a higher proportion of individuals aware of HPV and HPV vaccination;8,15 however, their samples included patients attending health care centers. The participants of these studies could have more access to HPV-related information which could increase their level of HPV awareness. Also, these studies did not include women below 18 years and data were drawn from larger cities, such as Medellín8 and Bogotá.15 Our study included not only nationwide data of women aged 18–49 years but also incorporated data of women from 13 to 17 years which represented 18.2% of the total sample. We identified that women in the youngest age group had the lowest prevalence of having heard about HPV vaccination. Studies in other countries have reported higher awareness of HPV vaccination.22,23 A recent study in developed countries identified that more than 80% of women had heard about HPV vaccination;23 in contrast, after a mass media advertisement campaign to promote HPV vaccination in Argentina, 36% of the women had an adequate knowledge about HPV vaccination.22
Different studies have considered the existence of variations in the level of awareness of HPV vaccination by socioeconomic8,15,21–25 and educational status.7–10,15,22,24,25 We identified that the prevalence of having heard about HPV vaccination was low among women who belonged to deprived socioeconomic levels, non-insured individuals, and women covered by the subsidized health insurance. These findings are in agreement with other studies showing socioeconomic disparities in knowledge of HPV vaccination in Colombia.8,15,21 A study conducted among individuals with genital warts in Bogotá identified that participants without health insurance coverage, and beneficiaries of the subsidized health insurance were less aware of HPV vaccination.15 In fact, individuals in the subsidized health insurance receive about 40% less health benefits than those in the contributory one,18 and most of the non-insured people belong to the lowest income group.17 Therefore, barriers to access health care experienced by disadvantaged groups in Colombia could be affecting knowledge about HPV and HPV vaccination, since health care professionals are an important source of information about HPV vaccination and a motivating factor for HPV vaccine intake.9,10,22,24,26
Our results show novel information regarding modifier effects of education and rural/urban residence on the awareness of HPV vaccination. In Colombia, researchers have identified that individuals living in rural areas are more likely to report a poor health status,27 and that these individuals are highly impacted by economic, political, and social problems of the country compared to people living in urban areas.28 Furthermore, low educational levels and high poverty indicators have been reported in departments located in the Amazon-Orinoquía, Pacific, and Atlantic regions.29 These findings agree with our results that show low probabilities of having heard about HPV vaccination among women living in these three regions of Colombia, specifically if they have rural residence and low educational levels. Thus, there is a need to reduce these gaps when designing and implementing educational initiatives about HPV vaccination. Further programs educating the general population about CC and its relation to HPV are critical to increase knowledge about HPV vaccination.8,9,15,30
Although it is known the role that parents have in approving participation of their daughters in HPV vaccination programs,7,9,25,31,32 we identified that women with children were less likely to have heard about HPV vaccination compared to women with no children, adjusting by age and other factors. This lack of awareness suggests that parents could be experiencing limitations to obtain information about HPV vaccination. A qualitative study conducted in four Colombian regions showed that parents were unaware of HPV vaccination and that receiving information was central to decide vaccinating their daughters.31 Additionally, it needs to be recognized that the socioeconomic context of parents impacts on their ability to support HPV vaccination of their family members.25,31 Given that discussions about HPV vaccination between parents and children are a starting point to approach sexuality issues,31,32 continuous efforts to educate about CC prevention and HPV vaccination are definitely needed not only for young women10,30 but also for older populations (i.e. parents and grandparents). Women need multiple sources of information about HPV vaccination, including the advice that they could receive from other women they trust.30
We propose that CC prevention and education programs recognize and overcome existing inequities – “inequalities considered unfair or stemming from some form of injustice”33 – in the awareness of HPV vaccination. Therefore, national and local campaigns should be encouraged to change the paradigm of insufficient commitment to improve prevention and health promotion programs within the Colombian SGSSS.19 These campaigns should ensure the reception of educational messages about HPV vaccination in the general population, emphasizing socially disadvantaged groups.22,24,25 Furthermore, working with health care professionals, schools, and community organizations might help develop better health promotion and preventive strategies to overcome difficulties related to area and region of residence, educational level, and health insurance coverage. We also recommend studies that evaluate successful experiences about HPV vaccination awareness and CC prevention campaigns to adjust and replicate them across the country. These studies should also include an assessment of the knowledge about HPV infection and HPV vaccination using validated instruments.23,34 Given that HPV vaccination is an insured service and that the Colombian Ministry of Health is leading CC prevention strategies,14 awareness of HPV vaccination in upcoming studies could be compared to our results to explore persistence of inequities.
Limitations of this study are primarily due to its cross-sectional design, which only provides information about associations. In addition, our study evaluated whether women had heard about HPV and a vaccine to prevent CC, which could be considered as a proxy of HPV vaccination awareness. Also, it needs to be acknowledged that social desirability could have an impact on the findings.
In conclusion, almost three quarters of the women in Colombia had not heard about HPV vaccination. The socio-demographic variations found on having heard about HPV vaccination indicate the presence of inequities and a social gradient in the awareness of HPV vaccination in Colombia. These findings suggest that programs raising awareness of vaccination to prevent CC have had a poor impact and that they could be neglecting marginalized groups of women in Colombia. Hence, further educational programs about CC prevention and HPV vaccination should target the general population, although specific strategies are also necessary to reach disadvantaged groups (low socioeconomic strata, individuals with subsidized health insurance, women with no education, and those living in isolated or rural regions).
Cervical cancer (CC) is the most frequent cancer affecting women in Colombia. A lack of awareness of HPV vaccination, critical for vaccination uptake and CC prevention, has been described among disadvantaged groups. There are no nationwide studies about socioeconomic factors associated with awareness of HPV vaccination among Colombian women.
What does this study add to the literature?Our nationwide results show the presence of inequities and a social gradient on having heard about HPV vaccination among women in Colombia, identifying a key role of education and rural residence on HPV awareness. HPV vaccination programs should include specific strategies to reach women with low socioeconomic status, subsidized health insurance, no insurance, no education, low education, and those living in isolated and rural areas.
Pere Godoy.
Contributions of authorshipS. Bermedo-Carrasco designed the study, conducted the analyses, interpreted the results, and drafted the manuscript; CX Feng contributed to the study design and interpretation of the results; JN Peña-Sánchez collaborated in the data analysis and interpretation of the results; and, R Lepnurm contributed to interpretation of the results. All authors critically reviewed the manuscript and approved the final version submitted for publication.
FundingNo funding.
Conflicts of interestThe authors declare no conflicts of interest.
We express our gratitude to Profamilia Colombia and the U.S. Agency for International Development that facilitated access to the 2010 NDHS. Also, we thank Profamilia for the guidance received, as well as Adriana Pulido and Jacqueline Kurmey for their support. Finally, we acknowledge the Western Regional Training Centre for Health Services Research (WRTC) for supporting the doctoral studies of S Bermedo-Carrasco and JN Peña-Sánchez.