To examine the relationship between maternal intelligence-mental health and neuropsychological development at age 14 months in a normal population, taking into account maternal occupational social class and education.
MethodsWe prospectively studied a population-based birth cohort, which forms part of the INMA (Environment and Childhood) Project. Cognitive and psychomotor development was assessed at 14 months using Bayley Scales of Infant Development. Maternal intelligence and mental health were assessed by the Cattell and Cattell test and the General Health Questionnaire-12 respectively.
ResultsWe observed a crude association between maternal intelligence and cognitive development in children at 14 months but this association disappeared when maternal education was included. The associations were stratified by maternal education and occupational social class. Within the manual maternal occupational social class, there was a significant difference in cognitive development between children whose mothers scored in the highest tertile of maternal IQ and those whose mothers scored in the lowest tertile. In contrast, no differences were observed among children whose mothers were in the non-manual occupational social class.
ConclusionsThe association between maternal intelligence and child cognitive development differed by occupational social class. While this association was not confounded by education or other variables in manual occupational social classes, maternal education explained this association among advantaged occupational social classes.
Este estudio exploró la relación entre inteligencia y salud mental materna y desarrollo neuropsicológico infantil a los 14 meses de edad en población normal, teniendo en cuenta la clase social basada en la ocupación y el nivel educativo maternos.
MétodosEstudio prospectivo de cohortes de nacimiento englobado dentro del proyecto INMA (Infancia y Medio Ambiente). El desarrollo cognitivo y psicomotor fue evaluado mediante la escala Bayley de desarrollo infantil. La inteligencia y la salud mental maternas se evaluaron usando el Test de Cattell y Cattell, y el Cuestionario de Salud General de 12 ítems, respectivamente.
ResultadosSe observó una asociación cruda entre inteligencia materna y desarrollo cognitivo infantil a los 14 meses de edad. Sin embargo, esta asociación desaparecía cuando la educación materna era incluida. Las asociaciones fueron estratificadas por educación y clase social basada en la ocupación materna. En el estrato de clase social manual materna se observó una diferencia significativa en la escala mental de la escala Bayley entre esos niños cuyas madres puntuaron en el tercil más alto de inteligencia materna, comparado con el tercil más bajo. No obstante, no se observaron diferencias entre aquellos niños de clase social no manual materna.
ConclusionesExiste un patrón diferente en la asociación entre inteligencia materna y desarrollo cognitivo infantil según la clase social materna. Mientras la asociación no es confundida por la educación ni por otras variables en las clases sociales manuales, el nivel educativo materno explica esta asociación en las clases sociales no manuales.
The developing brain is exceptionally sensitive to environmental influences, such as chemical agents, nutrition and medical care, as well as to education, experiences and the social environment.1–5 The social environment is composed of familial and cultural characteristics that exist in society and impact on neuropsychological development.6 Early development is recognized as a policy priority since ‘the early childhood period is considered to be the most important developmental phase in an individual's lifespan’.7 A review of proximal risk factors for child development in the context of developing countries identified inadequate cognitive stimulation as the most important psychosocial determinant, along with maternal depression and exposure to violence.8 In developed countries, poor cognitive stimulation at early ages may produce a wide range of non-adaptive neurobehavioral outcomes.9
Early parental influences are crucial in the early stages of brain maturation, and are specifically related to sensitivity and early cognitive stimulation.10 Among these influences, maternal intelligence is an important determinant in the early stages of child neuropsychological development. On average, about 50% of the variance in intelligence is due to genetic differences.11 Apart from the genetic contribution, mothers with higher scores in an intelligence test probably have better parenting skills, involving factors such as dietary patterns, health care, housing, and the provision of a cognitively-stimulating environment. A fundamental characteristic of brain development is that environmental experiences are as important as inherited factors.12 Tong et al.13 found that maternal intelligence quotient (IQ) was positively predictive of children's cognitive development. The same study also found that socioeconomic position and the domestic environment were positively associated with child neuropsychological development. Income, education and occupation have been found to be positively associated with better parenting.14 A cross-cultural review found that socioeconomic indicators were strongly related to cognitive development from infancy to middle childhood.15
In contrast, maternal depression may be considered a risk factor for child development, including impairments in the areas of social-emotional development, behavior, and cognitive development.16–19 The effects of depression on the parenting practices of mothers may include disruption in displays of affection, inadequate attention to basic safety, care and sleep regulation, use of harsh discipline, less utilization of primary care and greater utilization of emergency care.20
The aim of this study was to disentangle the direct effects of maternal IQ and mental health on early childhood neuropsychological development. To reduce residual confounding in the associations, and because of the strong relationship between maternal intelligence and mental health and socioeconomic variables, maternal education and occupational social class were treated as confounders and potential effect modifiers in the analyses. Moreover, a large number of potentially confounding variables, especially those related to child stimulation, were also included.
MethodsA population-based birth cohort was established in the city of Sabadell (Barcelona, Catalonia, Spain) as part of the INMA (Environment and Childhood) Project21. Between July 2004 and July 2006, 657 pregnant women who visited the public health center of Sabadell for an ultrasound scan in the first trimester were recruited. These women were then followed-up during pregnancy. A total of 619 (94.2%) children were enrolled at birth, and 588 (89.5%) were followed-up until 14 months. The main analyses in this report are based on 523 children with complete information on maternal IQ-mental health and neuropsychological development assessment. Information on maternal education, socioeconomic background, parity, alcohol consumption, dietary intake, and smoking during pregnancy was obtained through questionnaires administered during pregnancy (first and third trimesters). Anthropometric measures, sex, and gestational age were obtained at birth from clinical records. Data on breastfeeding were based on questionnaires administered to the mothers at 6 and 14 months after delivery. The study was approved by the Clinical Research Ethical Committee of the Municipal Institute of Healthcare (CEIC-IMAS), and all the participating mothers gave informed consent.
Neuropsychological development assessmentNeuropsychological development was assessed at 14 months (range 12 to 17 months) using the mental and psychomotor scales of the Bayley Scales of Infant Development (BSID).22 All testing was done at the primary care center in the presence of the mother by two specially trained neuropsychologists who were unaware of any exposure to information. Four-hundred and fifty-nine children were assessed by psychologist 1 and 102 children by psychologist 2. Nine children's tests were excluded because of specific abnormalities in the child [immaturity (n = 4), Down's syndrome, very low preterm, autistic traits (n = 2) and hypotonia].
The mental scale consisted of 163 items that assessed age-appropriate cognitive development in areas such as performance ability, memory, and first verbal learning. The psychomotor scale consisted of 81 items assessing fine and gross motor development. Index scores were computed based on the assumption of a normal distribution with a mean of 100 corresponding to the mean of the raw scores, and a standard deviation of 15.
To limit inter-observer variability, a strict protocol was applied, including inter-observer-training and three sets of quality controls (inter-observer reliability tests) done during the fieldwork. The inter-rater reliability was estimated by an intra-class correlation of 0.93 for the mental test score and an intra-class correlation of 0.96 for the psychomotor scale. Cronbach's alpha coefficient was used to determine the internal consistency of the mental and psychomotor scales. The alpha coefficient was 0.78 for the mental test score and was 0.73 for the psychomotor scale.23
Finally, the psychologists also flagged the tests that might be difficult to evaluate because of less than optimal cooperation of the child (n = 24), classified as behavioral problems (e.g., bad moods, nervousness, etc.) or a particular situation (e.g., tiredness, colds, asleep, etc.) in a new variable designated “quality of neuropsychological test”.
Maternal intelligence quotient and mental healthTwo maternal factors were considered in this study: maternal IQ and mental health, assessed at the same time as the child's neuropsychological developmental tests (14 months).
Maternal IQ was assessed by two psychologists using the 2 and 3 scales of Factor “G” of Cattell and Cattell,24 which is a nonverbal test of fluid intelligence.22 The test was administered in 532 of the recruited women. Mean and standard deviation data of our sample were used to compute index scores assuming a normal distribution. Raw scores were standardized to a mean of 100 with a standard deviation of 15.
Maternal mental health was assessed using the Spanish version of the General Health Questionnaire-12 items (GHQ-12) as a self-reported questionnaire.25,26 Each of the 12 items assesses the severity of a mental problem over the past few weeks using a 4-point Likert-type scale (from 0 to 3). The score was used to generate a total score ranging from 0 to 36, where higher scores indicated poorer mental health.
For the GHQ-12, 79 mothers were randomly selected to calculate the 1-month test-retest reliability using the Kappa value. We obtained Kappa coefficients of agreement of around 0.87 for the GHQ-12. Cronbach's alpha coefficients showed acceptable internal congruence (0.79). Spearman's coefficients were used to analyze the correlation between maternal IQ and mental health, and obtained a correlation between maternal IQ and maternal mental health of rho = -0.09 (p = 0.038). Paternal IQ and mental health were also assessed using the same methodologies, but IQ was available for only 104 participants.
Other variablesEducational level was defined using three categories: primary or less, secondary school, and university. Occupational social class was coded from the longest-held job during the pregnancy or, if the mother did not work in this time period, the last job prior to pregnancy. A few of the mothers had never worked and in these cases the father's last job was used (n = 22). Occupations were coded using the four-digit Spanish National Classification of Occupations (Clasificación Nacional de Ocupaciones, CNO94), which is closely related to the international ISCO88 coding system.27 Five social class categories were then created following the methodology proposed by the Spanish Epidemiological Society.28 These categories were regrouped into manual and non-manual jobs.
Predominant breastfeeding was defined as an infant receiving breast milk only (but allowing supplementation of non-milk liquids): drinking water or water-based drinks (sweetened and flavoured water, teas, infusions, etc), fruit juice, oral rehydration salts or solutions, drops, and syrup forms of vitamins, minerals, and medicines.29 The duration of predominant breastfeeding was categorized into four groups (<2 weeks, 2-16, 16-24, >24). Other variables were maternal work status at the time of the BSID assessment (employed, unemployed), parental country of birth (Spain, foreign), child's sex (girls, boys), low birth weight (<2,500g), preterm birth (<37 weeks), Apgar score at 1minute (<8 considered non-optimal), number of siblings at the time of birth (0, 1, 2 or more), and maternal smoking during pregnancy (never, former, current).
Statistical analysisUnivariate descriptive analysis of the neuropsychological test (mental and psychomotor scales of the BSID), predictive variables (maternal IQ and mental health), socioeconomic characteristics of the parents, and anthropometric measures of children were carried out to describe the population.
Bivariate associations (t-test or ANOVA) between parental sociodemographic covariates and child clinical measures and outcomes (mental and psychomotor scales) were analyzed to detect potential confounders (p <0.25).
Multivariable linear regression models were built for mental and psychomotor test scores considering all potential confounding variables using backward stepwise regression methods. Any covariate either with a p-value of less that 0.25 or resulting in a change in estimate of predictive variables (maternal IQ or mental health) of 10% or more was retained in the model.
For each predictive variable, we fitted three multiple linear regression models: 1) adjusting only for the psychologist, the child's age in days, and the quality of the neuropsychological test; 2) also adjusting for potential confounders plus maternal occupational social class; and 3) also adjusting for maternal education. Predictive variables were examined in tertiles taking the lowest tertile as the reference group. This categorical approach allowed us to explore the differences in infant neuropsychological development between extreme groups. To study the combined impact of both the predictive variables, we also fitted a model in which they were mutually adjusted.
Finally, maternal education and occupational social class were considered as potential effect modifiers (p for interaction <0.10) for the relationship between maternal IQ-mental health and child cognitive and psychomotor development. Statistical analyses were done using Stata 8.2 (Stata Corporation, College Station, Texas).
ResultsThe mean age of the children was 14.8 months (range: 12-17 months). Four percent of the children had low birth weight, 2% with a gestational age of less than 37 weeks (preterm), and 5% with a non-optimal score in the Apgar test at 1minute (table 1). Forty-two percent of the mothers had secondary education and 32% had university education. Fifty-three percent were classified as belonging to a non-manual occupational social class. Ten percent of mothers were immigrants and 15% were current smokers during pregnancy. Paternal educational level was similar to that in mothers, but the occupational social class distribution was markedly different. More than 50% of the fathers in the sample were classified as belonging to the manual occupational class. In general, the mothers who participated in the psychological profile tests had higher levels of education than those who did not participate (data not shown). For occupational social class no differences were found.
Description of the sample (n = 523).
| Child characteristics | |
| Age (months), mean (SD) | 14.80 (0.67) |
| Sex | |
| Girls | 260 (49.7) |
| Boys | 263 (50.3) |
| Predominant breastfeeding | |
| <2 weeks | 117 (22.5) |
| 2-16 weeks | 155 (29.8) |
| 16-24 weeks | 196 (37.7) |
| >24 weeks | 52 (10.0) |
| Low birth weight (<2500 g) | 23 (4.4) |
| Preterm (<37 weeks) | 13 (2.5) |
| Apgar score at 1 minute (≥8, optimal) | 493 (95.4) |
| Siblings at birth | |
| 0 | 306 (58.7) |
| 1 | 186 (35.7) |
| 2 or more | 29 (5.6) |
| Maternal characteristics | |
| Age (years), mean (SD) | 32.8 (4.3) |
| Occupational social class | |
| Manual | 242 (46.3) |
| Non-manual | 281 (53.7) |
| Education | |
| Primary or less | 130 (25.0) |
| Secondary school | 223 (42.9) |
| University | 167 (32.1) |
| Work status at child's 14 months (employed) | 368 (70.9) |
| Country of birth (foreign) | 51 (9.9) |
| Smoking during pregnancy | |
| Never | 220 (42.5) |
| Former | 217 (42.0) |
| Current | 80 (15.5) |
| Paternal characteristics | |
| Age (years), mean (SD) | 34.7 (4.9) |
| Occupational social class | |
| Manual | 290 (58.7) |
| Non-manual | 204 (41.3) |
| Education | |
| Primary or less | 170 (32.8) |
| Secondary school | 225 (43.4) |
| University | 123 (23.8) |
| Country of birth (foreign) | 58 (11.2) |
Values are n (percentages) unless otherwise stated. Differences in the number of observations for some of the variables presented in the table are due to missing values.
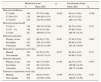
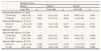
Distributions of the BSID scores by maternal IQ and mental health, and parental socioeconomic characteristics were plotted (table 2). A positive trend was observed in child mental test score related to maternal intelligence, but not to psychomotor scores. There was a positive trend in the distribution of maternal IQ related to maternal education and occupational social class (table 3). Mothers who had a university degree or who belonged to the non-manual occupational social class scored significantly higher in the IQ test.
Distribution of the child mental and psychomotor test scores by maternal intelligence and mental health and parental socioeconomic characteristics.
| Mental test score | p | Psychomotor Scale | |||
| n | Mean (SD) | Mean (SD) | p | ||
| Maternal intelligence | |||||
| T1 (≤94) | 194 | 97.79 (14.98) | 0.029 | 99.61 (14.01) | 0.769 |
| T2 (94-107) | 175 | 100.58 (14.33) | 99.27 (15.25) | ||
| T3 (≥107) | 154 | 101.95 (15.68) | 100.4 (15.36) | ||
| Maternal mental health | |||||
| T1 (≥11) | 156 | 100.22 (15.59) | 0.302 | 99.75 (14.03) | 0.171 |
| T2 (8 – 11) | 149 | 98.23 (15.20) | 97.80 (15.63) | ||
| T3 (≤8) | 201 | 100.66 (15.18) | 100.76 (14.35) | ||
| Maternal education | |||||
| Primary or less | 130 | 96.28 (17.52) | 0.002 | 97.20 (15.39) | 0.062 |
| Secondary | 223 | 100.13 (13.65) | 99.98 (14.50) | ||
| University | 167 | 102.43 (14.36) | 101.24 (14.65) | ||
| Maternal occupational social class | |||||
| Manual | 242 | 98.70 (14.76) | 0.077 | 99.48 (14.47) | 0.717 |
| Non-manual | 281 | 101.03 (14.35) | 99.96 (15.24) | ||
| Paternal education | |||||
| Primary or less | 170 | 99.17 (15.05) | 0.165 | 98.37 (15.47) | 0.353 |
| Secondary | 225 | 99.13 (14.19) | 100.08 (14.28) | ||
| University | 123 | 102.09 (16.38) | 100.72 (14.98) | ||
| Paternal occupational social class | |||||
| Manual | 290 | 98.85 (14.92) | 0.046 | 99.27 (15.36) | 0.311 |
| Non-manual | 204 | 101.60 (14.92) | 100.65 (14.29) | ||
T: tertile.
Differences in the number of observations for some of the variables presented in the table are due to missing values.
Distribution of maternal IQ and mental health by maternal education and occupational social class.
| Intelligence | Mental Health | |||||
| n | Mean(SD) | p | n | Mean(SD) | p | |
| Maternal education | ||||||
| Primary or less | 130 | 89.82 (12.76) | <0.001 | 121 | 10.62 (4.34) | 0.088 |
| Secondary | 223 | 99.39 (13.17) | 220 | 10.37 (4.44) | ||
| University | 167 | 108.83 (12.26) | 162 | 9.59 (3.78) | ||
| Maternal occupational social class | ||||||
| Manual | 242 | 93.03 (13.52) | 232 | 10.52 (4.42) | 0.101 | |
| Non-manual | 281 | 106.05 (12.73) | <0.001 | 274 | 9.90 (4.02) | |
Differences in the number of observations for some of the variables presented in the table are due to missing values.
The crude associations between parental and child characteristics and mental and psychomotor scales were plotted (fig. 1). In the multivariate regression models, the mental test score significantly increased with higher maternal IQ; after adjusting for all potential confounders except maternal education, the association remained marginally statistically significant (table 4). However, the association disappeared when maternal education was included. No association was observed between the mental test score and maternal mental health. None of the three specific factors of mental health were associated with the mental test score (p >0.10, not shown). No associations were found between the scores of the psychomotor tests and maternal profile variables. Paternal mental health had no effect in the models.
Adjusted association between child mental and psychomotor test scores and maternal intelligence and mental health.
| Mental test score | ||||||
| Model 1 | Model 2 | Model 3 | ||||
| Coef. (SE) | p | Coef. (SE) | p | Coef. (SE) | p | |
| Maternal IQ (reference T1 ≤94) | ||||||
| T2 (94-107) | 2.69 (1.38) | 0.052 | 1.91 (1.45) | 0.188 | 0.88 (1.52) | 0.563 |
| T3 (≥107) | 4.31 (1.43) | 0.003 | 3.13 (1.54) | 0.043 | 1.39 (1.69) | 0.411 |
| Maternal MH (reference T1 ≥11) | ||||||
| T2 (8-11) | -1.31 (1.43) | 0.360 | -1.33 (1.45) | 0.357 | -1.43 (1.44) | 0.321 |
| T3 (≤8) | 0.60 (1.40) | 0.672 | -2.68 (1.56) | 0.094 | -2.58 (1.56) | 0.099 |
| Mutually adjusted | ||||||
| Maternal IQ (reference T1 ≤94) | ||||||
| T2 (94-107) | 2.70 (1.40) | 0.054 | 1.82 (1.47) | 0.217 | 0.81 (1.53) | 0.598 |
| T3 (≥107) | 4.59 (1.47) | 0.002 | 3.34 (1.58) | 0.035 | 1.49 (1.74) | 0.392 |
| Maternal MH (reference T1 ≥11) | ||||||
| T2 (8-11) | -1.55 (1.44) | 0.280 | -1.34 (1.47) | 0.365 | -1.32 (1.47) | 0.372 |
| T3 (≤8) | 0.87 (1.43) | 0.542 | -2.86 (1.59) | 0.072 | -2.65 (1.60) | 0.098 |
| Psychomotor scale | ||||||
| Model 1 | Model 4 | Model 5 | ||||
| Coef. (SE) | P | Coef. (SE) | p | Coef. (SE) | p | |
| Maternal IQ (reference T1 ≤94) | ||||||
| T2 (94-107) | -0.38 (1.46) | 0.797 | -0.59 (1.49) | 0.693 | -1.48 (1.56) | 0.343 |
| T3 (≥107) | 0.95 (1.52) | 0.533 | -0.13 (1.57) | 0.932 | -1.47 (1.74) | 0.397 |
| Maternal MH (reference T1 ≥11) | ||||||
| T2 (8-11) | 0.98 (1.46) | 0.503 | 0.97 (1.48) | 0.513 | -1.82 (1.52) | 0.230 |
| T3 (≤8) | -1.46 (1.58) | 0.357 | -0.89 (1.59) | 0.575 | -0.79 (1.49) | 0.594 |
| Mutually adjusted | ||||||
| Maternal IQ (reference T1 ≤94) | ||||||
| T2 (94-107) | 0.21 (1.47) | 0.884 | -0.09 (1.50) | 0.953 | -0.88 (1.56) | 0.575 |
| T3 (≥107) | 1.37 (1.55) | 0.374 | 0.26 (1.60) | 0.871 | -0.97 (1.77) | 0.584 |
| Maternal MH (reference T1 ≥11) | ||||||
| T2 (8-11) | 0.75 (1.50) | 0.615 | 0.93 (1.52) | 0.539 | -1.92 (1.54) | 0.215 |
| T3 (≤8) | -1.84 (1.62) | 0.255 | -1.12 (1.63) | 0.491 | -0.80 (1.52) | 0.597 |
Coef.: coefficient; Maternal MH: maternal mental health; SE: standard error; T: tertile.
Model 1: adjusted for psychologist, child's age in days and quality of neuropsychological test.
Model 2: adjusted for variables in model 1 plus parental occupational social class, sex of the child, parental country of birth, maternal age and maternal work status at child's 14 months.
Model 3: adjusted for variables in model 2 plus maternal education.
Model 4: adjusted for variables in model 1 plus Apgar score at 1minute, preterm birth, maternal work status at child's 14 months and maternal age.
Model 5: adjusted for variables in model 4 plus maternal education.
Finally, these associations were stratified by maternal education and occupational social class (table 5). Within maternal manual occupational social class, there was a significant difference (coef = 7.92) in the mental test score between children whose mothers scored in the highest tertile of maternal IQ compared with children whose mothers scored in the lowest tertile. No such differences were observed, however, among children whose mothers were in the non-manual occupational social class. These differences between strata showed a significant interaction (p for interaction = 0.044). A similar result was found among children whose mothers had primary education (coef = 6.75), but this difference was not statistically significant (p = 0.18), also contrasting with no differences among children whose mothers were highly educated. Maternal mental health showed no difference between different occupational social classes. Maternal education and occupational social class did not modify the relationship between maternal IQ-mental health and infant psychomotor development (data not shown).
Adjusted association between child mental test score and maternal intelligence and mental health with stratification by maternal education and maternal occupational social class.
| Primaryb | Secondary and university | Manualc | Non-manual | |||||||
| Coef. (SE) | p | Coef. (SE) | p | p for interaction | Coef. (SE) | p | Coef. (SE) | p | p for interaction | |
| Referencea | 94.86 | 101.74 | 97.63 | 94.35 | ||||||
| Maternal IQ - T2 (94-107) | 1.35 (3.72) | 0.689 | -0.18 (1.70) | 0.918 | 0.696 | 0.38 (1.98) | 0.847 | 0.09 (2.33) | 0.971 | 0.044 |
| Maternal IQ - T3 (≥107) | 6.75 (5.03) | 0.183 | 0.63 (1.82) | 0.729 | 7.92 (2.79) | 0.005 | -0.95 (2.31) | 0.680 | ||
| Maternal MH - T2 (8 – 11) | -2.98 (3.37) | 0.380 | -0.47 (1.60) | 0.771 | 0.527 | -1.74 (2.14) | 0.417 | -1.54 (1.99) | 0.441 | 0.966 |
| Maternal MH - T3 (≤8) | 1.35 (3.55) | 0.705 | 0.66 (1.56) | 0.674 | 1.05 (2.06) | 0.609 | 0.72 (1.99) | 0.718 | ||
Coef.: coefficient; Maternal MH: maternal mental health; SE: standard error; T: tertile.
In this population-based birth cohort, the effect of maternal intelligence on child cognitive development at 14 months of age was stronger than the effect of maternal mental health; this relationship was found to be mostly explained by maternal education. However, in more disadvantaged occupational social classes, maternal intelligence appeared to be the best predictor of optimal child cognitive development, exceeding both maternal education and mental health.
In previous research,13 an independent association was found between maternal IQ and the cognitive development of toddlers, along with socioeconomic status (SES) and the home environment. In our study, the association observed between maternal IQ and child cognitive development disappeared after adjustment for maternal education, but persisted when maternal occupational social class was included. Some authors have pointed out that general intelligence is highly predictive of educational level.30 This might imply that IQ should exceed educational level, perhaps due to a strong hereditary component, and to some extent should predict educational attainment in life. If this were the case, the scores of children in mental test scores should be strongly associated with maternal IQ and, to a lesser degree, with maternal education. However, our data does not support such a hypothesis. Other authors31 have pointed out that the proportion of variability in a population's IQ that is attributable to genetic factors is unclear. We found that maternal educational attainment was strongly related to child neuropsychological development. Along with SES, low maternal education has been found to be an important predictor of neuropsychological developmental problems in different contexts.10 It has been hypothesized that women with higher IQ scores and higher educational level offer better parenting, involving factors such as lifestyle, healthcare, housing, and the provision of a cognitively-stimulating environment. A relationship between maternal education and dietary patterns in infancy has been found.32 In turn, studies suggest that mothers with low education lack the intellectual skills required to stimulate their children.33
Within manual occupation social classes, maternal IQ appears to be an important predictor of child cognitive development. The children of mothers belonging to a manual occupational social class with high scores in IQ tests scored significantly higher on the BSID mental test than the children of less intelligent mothers belonging to the same occupational social class. Previous studies have found that SES is an important predictor of neuropsychological development, especially for language and executive function.30 There is some support for the hypothesis that less cognitive stimulation is provided by parents and the environment in deprived areas, and that this mechanism may produce disparities in neuropsychological development between different social classes.34 In our study, those mothers belonging to manual occupational social classes but with higher intelligence than the group average represented a special subgroup within the manual class. This finding could indicate that mothers with higher intelligence have children with higher intelligence, irrespective of their educational level. By way of explanation, these mothers might offer their children a more stimulating environment within which they have greater opportunities to develop their cognitive functions.
We found no association between maternal mental health and child neuropsychological development. A possible explanation could be that this study was performed in a non-clinical population in which mothers were not suffering from major depressive disorders or any other serious psychiatric disorders. The distribution of GHQ-12 scores had low variability and did not reveal any subclinical symptomatology. Nevertheless, throughout the school years, cognitive development becomes more specific and, in turn, neuropsychological testing is more precise, reliable and valid than at previous ages.34 The follow-up of the birth cohort will allow us to explore whether an effect on cognitive development appears at older ages, and whether this affects children's social behaviour.
No associations were found between maternal IQ and mental health and child psychomotor development at 14 months. The psychomotor scale showed a stronger association with preterm birth, Apgar scores at 1minute, maternal work status at 14 months, and maternal age. Very preterm infants scored significantly lower than full-term infants on the psychomotor scale of the BSID but no significant differences were found between the groups on the mental test score.35 In other studies, negative Apgar scores have been found to be related to neurological disability.36 Maternal employment at the ninth month was found to be linked to lower scores in a cognitive test at 36 months.37
A major strength of this study is its large sample size. We studied a population-based cohort of 559 children using field staff, interviewers, laboratory technicians, and project pediatricians, all of whom were specifically trained for the project. For the neuropsychological assessments, several quality controls were introduced (inter-observer reliability tests) and the psychologists who assessed children with the BSID questionnaire received extensive training in this questionnaire.
Our study was limited by a number of factors. Although we included a large number of covariates, we were unable to control for some factors that may affect children's cognition, such as the quality of their home environment, nutrition, maternal postpartum depression or maternal stress during pregnancy. Omitting these factors may have introduced residual confounding.38 Moreover, we used self-reported questionnaires for the parents to assess sociodemographic characteristics and mental health, which could have introduced a response bias. However, such a bias would most likely be non-differential and lead to reduced statistical power. Despite the importance of maternal characteristics during the first years of life, information on the father is also valuable. Unfortunately, such information was not available and we could not assess paternal IQ or mental health across the entire sample. Finally, measurements of mental health vary with time. For the assessment of long-term effects, repeated measurements during and just after pregnancy are required.
We conclude that in this general population, variations in maternal mental health were low and their effects on neuropsychological development were not detected at 14 months of age. Maternal IQ plays an important role in the first stages of cognitive development in children in more disadvantaged occupational social classes. For the other groups, the effects of maternal IQ on cognitive development were mostly explained by maternal education. Future research should assess whether these findings continue to be observed at a later stage of development when phenotypes are more highly developed.
Several observational studies have reported negative associations between some chemical agents or an impoverished social environment and children's cognitive development. Maternal intelligence and mental health seem to be related to child neuropsychological development, especially in specific populations (clinical, exposed to chemicals agents, etc.). The effect of maternal intelligence and mental health on child neuropsychological development at early ages and in a non-risk population is unknown. Moreover, the differential effects of these factors among distinct occupational social classes have not been determined.
What does this study contribute to the literature?To our knowledge, this is the first large population-based study to assess the joint association between maternal intelligence and mental health and children's neuropsychological development. Moreover, this research examines the role of occupational social class in this association. Globally, maternal intelligence seems to play an important role in child cognitive development; however, when maternal education is taken into account, this role becomes minor and non-significant. In manual occupational social classes, the association between maternal intelligence and child cognitive development was not confounded by maternal education or other variables.
J. Forns analyzed the data, drafted the manuscript and gave final approval of the version to be submitted. J. Julvez, M. Vrijheid, M. Guxens, M. Ferrer and J. Sunyer designed the study, developed the questionnaires, supervised the survey and revised the manuscript critically. J. Grellier revised the manuscript critically, contributed to drafting the manuscript, and corrected the quality of the written English. R. Garcia-Esteban contributed to the statistical analyses and read the manuscript critically. All the authors have read and approved the final manuscript.
FundingThis work was supported by grants from the Spanish Ministry of Health [FIS-PI041436]; Instituto de Salud Carlos III [Red INMA G03/176 and CB06/02/0041]; the Generalitat de Catalunya-CIRIT [1999SGR 00241]; the EU sixth framework project NEWGENERIS [FP6-2003-Food-3-A-016320]; and Fundació Roger Torné.
Conflict of interestsNone.
The authors would like to acknowledge all the study participants for their generous collaboration. We are also grateful to Silvia Folchs, Anna Sànchez, Maribel López, Nuria Pey, and Muriel Ferrer for their assistance in contacting the families and administering the questionnaires. A full roster of the INMA-Sabadell Study Investigators can be found at http://www.proyectoinma.org/cohorts/sabadell/en_membres-sabadell.html