To evaluate the efficacy of a healthcare education program for patients with hypertension.
MethodsA multicenter, prospective, cluster-randomized trial was conducted. Randomization was by primary care center; 18 of 36 urban primary care centers in Barcelona and its metropolitan area were randomized to the intervention group (IG) and 18 to the control group (CG). The study sample consisted of patients with hypertension (n=996; 515 in the IG and 481 in the CG) receiving outpatient treatment with antihypertensive drugs. The intervention consisted of personalized information by a trained nurse and written leaflets. Questionnaires on knowledge and awareness of hypertension and its medication, treatment adherence, healthy lifestyle habits, systolic and diastolic blood pressure, and body mass index were assessed at each visit, with a 12-month follow-up. An intention-to-treat analysis was applied.
ResultsKnowledge of hypertension increased by 27.8% in the IG and by 18.5% in the CG, while that of medication increased by 10.1% in the IG and 5.5% in the CG. Treatment adherence measured by the Morisky-Green test increased by 9.6% (95% CI: 5.5–13.6) in the IG and 8.8% (95% CI: 4.9-12.6) in the CG. There were no differences in adherence on the other tests used. No differences were observed between the IG and CG in clinical variables such as blood pressure or BMI at the end of the trial.
ConclusionsThe educational intervention had no significant impact on patients’ adherence to the medication.
Evaluar la eficacia de un programa de educación sanitaria en pacientes con hipertensión.
MétodosSe diseñó un estudio multicéntrico prospectivo y aleatorizado de conglomerados. La unidad de aleatorización fueron los centros de atención primaria (CAP) situados en Barcelona y su área metropolitana, con 18 CAPs urbanos asignados al grupo intervención (GI) y 18 al grupo control (GC). La muestra de pacientes hipertensos que recibían tratamiento con antihipertensivos ambulatoriamente fue de 996 (GC=481 y GI=515). La intervención consistió en información personalizada mediante enfermera entrenada y material educativo escrito. Se midió en cada visita la presión arterial, el índice de masa corporal, el conocimiento de la enfermedad y de la medicación, la adherencia al tratamiento y los hábitos saludables; el seguimiento fue de 12 meses. Para el análisis de los datos se aplicó el criterio de intención del tratar.
ResultadosEl conocimiento de la enfermedad aumentó un 27,8% en el GI y un 18,5% en el GC, así como el de la medicación un 10,1% en el GI y un 5,5% en el GC. La adherencia al tratamiento mediante la prueba de Morisky-Green aumentó un 9,6% en el GI y un 8,8% en el GC. No se observaron diferencias entre GI y GC en las otras medidas de adherencia, ni en las variables clínicas relativas a la presión arterial o el índice de masa corporal al final del ensayo.
ConclusionesLa intervención educativa no mostró un impacto significativo en el la adherencia a la medicación de la hipertensión.
Control of hypertension is associated with long term health outcomes.1,2 Adherence to pharmacological and non pharmacological therapy is essential in order to achieve such control.3–5 Adherence can be defined as the extent to which a person's behavior corresponds with agreed recommendations from a health care provider.6 Problems with follow-up of therapeutic recommendations are common in almost all pathologies7 and highly impacts the effectiveness of the treatment.8 The main factors related to adherence are the complexity of the therapeutic regimen and the adaptability of the recommendations to the usual habits of the patient. Also, the patient's knowledge about the pathology, previous experience with the health-care system, adherence to other previous recommendations, the doctor-patient relationship, patient's perception of health, and the benefits of the proposed recommendations are factors associated with adherence.6,9,10
Several interventions are proposed to improve adherence. Critical reviews have highlighted significant methodological problems,11-16 but the overall conclusion is that no single intervention is, per se, better than any other. A further conclusion is that combined cognitive and behavioural strategies are the most effective ones, and the evidence indicates that these aspects need to be incorporated into the design of strategies to improve adherence in the treatment of hypertension.12,13 Haynes et al.13 suggested that the interventions used need to be easy to apply in the health-care practice, and maintained over extended periods of time.
In the case of the hypertension, a condition that can exist for years without clinical symptoms, the problem of non-adherence and how to cope with it has long been recognized, and different recommendations have been introduced.3,15 In Spain,17,18 the percentage non-adherence to hypertension treatments is around 50%, a level similar to that of other countries and/or pathologies. Hypertension is a risk-factor for cardiovascular disease and is detected, evaluated, and treated mostly in the primary health-care setting. In Spain, the long-term control and follow-up of the hypertensive patient on an established treatment program is usually carried-out by clinic nurses under the direction and close supervision of the attending physician.19 This is also the case for other chronic pathologies such as diabetes or chronic bronchitis, as well as giving advice about diets and healthy lifestyle habits.20
The hypertensive patient with a long disease history can benefit from interventions that focus on improving adherence to the drug treatment in the primary health care setting as well as non-pharmacologic measures to improve control of hypertension. Nurses take care of the long term follow up of hypertensive patients in the primary health care setting.
We assessed the impact of information provided to patients in a personalized way by the clinic nurse with the objective of improving the patient's knowledge of the disease and adherence to the medication prescribed as well as the incorporation of healthy lifestyle habits. Also, we assessed the potential impact on systolic and diastolic blood pressure and body mass index (BMI).
Materials and MethodsStudy designThe study was designed as multi-centre, prospective, cluster-randomised, controlled clinical trial, using the primary healthcare centre as a randomization unit. Patients under anti-hypertensive drug therapy receiving the intervention (Intervention Group; IG) were compared with a control group (CG) receiving the usual clinical care.
SettingThe trial was conducted in Primary Health Care Centres (PHCC) located in Barcelona, Spain, and its metropolitan area. There were 36 centres involved (18 in the CG and 18 in the IG). One hundred ten nurses participated in the study, with 54 participating in the IG.
Study populationEligible patients were consecutively selected by their nurse, who informed them about the study objectives, and recruited all patients who agreed to participate. Patients were included if they had hypertension, were aged between 18 and 80 years, visiting the clinic for long-term follow-up and control of hypertension using anti-hypertensive drug therapy, and had attended the clinic for a minimum period of 6 months.
Individuals who had serious psychiatric, physical, or sensory alterations were excluded. The study protocol was approved by the Ethics and Research Committee of the Institut d’Investigació en Atenció Primària Jordi Gol i Gurina (Institute of Research in Primary Health Care in Catalonia).
The sample size requirement was estimated assuming a percentage of self-declared non-adherence to the hypertensive treatment. Given that previous studies observed a high degree of variability in this percentage (range, 16–60%), the sample was calculated using a non-compliance value of 40%. This implied a sample size of 487 individuals in each group were needed to detect a minimum of 10% reduction (at the end of the instructions/intervention) in the percentage non-compliers between the two groups (an alpha error of 5% and a beta error of 20%, with a loss to follow-up estimation of 20%).
Patients allocated to the control group received the usual clinical care without any standardized intervention, which usually implies a high inter-individual variability.
Intervention designIntervention was developed during the 3 phases described below.
1) Nurse training: the IG nurses took part in a 10-hour workshop focused on the anti-hypertension medications with an emphasis on adverse effects, pharmacological interactions, and patient centring with a special focus on comorbidity issues and other clinical variables. Between 6 and 10 nurses participated in each workshop. The programme consisted of two 4-hour sessions and one 2-hour session. To assure standardisation of the group sessions, 4 qualified pharmacists with extensive expertise in training activities, as well as in hypertension therapies and patient education, conducted the sessions. Specifically designed educational material was provided to all participating nurses.
2) Developing guidelines to standardize the information given to patients: guidelines to standardize the information that nurses should provide to patients were developed by the research team. These contained key information about the disease, healthy lifestyle habits, and messages targeted to each group of antihypertensive drugs used (mechanism of action, dosage, what to do if a pill is missed, adverse effects, and other recommendations). Also, the guidelines were designed as leaflets that allowed the development of a personalised therapeutic plan; general health messages aimed at promoting the good utilization of drugs.
3) Direct intervention with the patient: four visits were planned by the nurse to carry out the intervention, using the standardised guidelines developed for the intervention. Each visit lasted for an average of 15minutes. The information provided to the patient was personalized according to the needs of the patient.
Furthermore, schedule sheets with the treatment plan were provided, which contained information on the drugs prescribed, the dosage and schedule, and basic advice on how to maximize the treatment schedules. The purpose of these sheets was to reinforce the nurse's verbal instructions and advice to the patient.
Measurement and data collectionAll the information was obtained from a questionnaire administered at the start and at the 3-, 6- and 12-month follow-up visits. The interview was conducted by the nurse using forms specifically designed for the purpose. Clinical data were extracted from the clinical record by the nurse. The variables recorded at the initial visit (V0) and at the end of the 12-month follow-up (V4) included the following: sociodemographic (gender, age, education level); knowledge area (knowledge of hypertension and the anti-hypertension medications, recommendations regarding healthy lifestyle habits); patient adherence area (self-declared adherence to medication intake, pill count, and adherence to lifestyle recommendations); clinical (years since diagnosis of hypertension, systolic and diastolic blood pressure control of hypertension, BMI, number of anti-hypertensive drugs, other drugs taken, total number of drugs).
Blood Pressure (BP) was measured using a regularly-calibrated mercury sphygmomanometer. The mean of 2 determinations was noted in the control arm (highest BP) with at least 2minutes separating the measurements. A value of <140/90 mmHg was considered indicative of good blood pressure control.
The BMI was calculated as the weight (in kg) divided by the height (in m2).
The drug therapies prescribed for each participant were codified according to the ATC.21
The patient's knowledge or awareness of hypertension was evaluated using the Batalla test.22 Good knowledge of the disease required correct responses to the 4 questions on this topic in the questionnaire. Similarly, the patient's knowledge of anti-hypertensive drugs and recommendations for healthy lifestyle habits were obtained from the specific questions on these topics in the questionnaire.
Self-reported adherence to the medication was measured using the Haynes-Sackett and Morisky-Green tests, which were previously translated and validated,23,24 together with the patient's recall of the medications taken over the previous 3 months. The level of adherence on the Haynes-Sackett test was considered good if the patient answered «I had no difficulties with medication intake»; for the Morisky-Green test, adherence was assessed as the combined positive agreements to the following statements: «I do not forget to take a pill», «I take it at the scheduled time», and «I do not miss any pill when I am in good health”, and the declaration of having taken the pills over the previous 3 months «every day or most days». Adherence to medication was also evaluated based on pill counts, in which good compliance was considered to have occurred if the medication taken was between 80% and 110% of the pills prescribed.
Statistical analysisThe analyses were performed under the intention-to-treat criteria. To address potential biases caused by incomplete follow-up, we analyzed patients with incomplete data using the baseline value carried forward to replace missing values.
Differences between groups and within visit data were analyzed using statistical tests for independent data. Changes within the same groups between the initial and final clinic visits were evaluated using tests for related data. Cluster randomization was taken into account in the analysis using either a robust method for the calculation of standard errors. This analysis was carried out using the software R. The remaining analyses were carried out using the SPSS statistical package for Windows, version 13 (SPSS Inc., Chicago, IL).
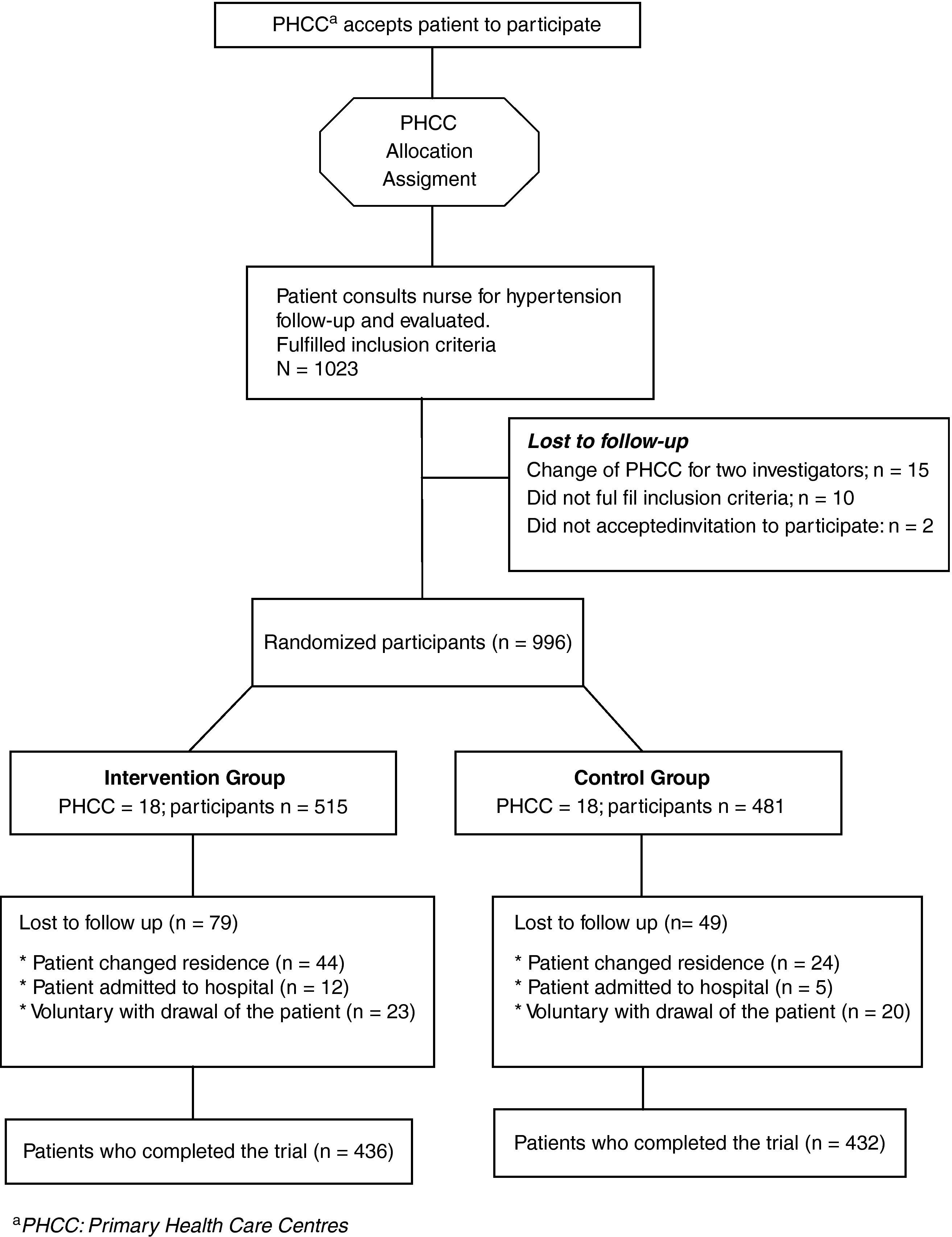
ResultsThe sample population included 515 subjects in the IG and 481 in the CG. During the follow-up, 79 patients in the IG (15.3%) and 49 (10.2%) in the CG exited the study (Fig. 1). No significant differences were observed between those who completed the study and those who did not (data not shown).
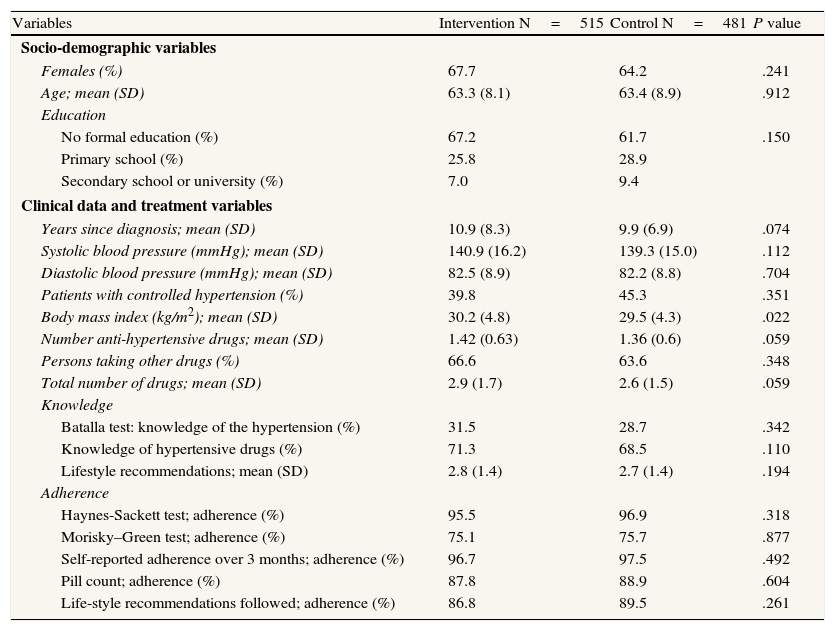
At the initial outpatient visit, the groups were comparable except that the BMI was significantly higher in the IG than the CG (Table 1). The mean age was 63 years, most participants were female, and two thirds of the participants had no formal education. About half of the participants had poor control of their hypertension, and the BMI in both groups indicated considerable obesity. The mean time since diagnosis of hypertension was 10 years. According to the Batalla test, one of every three patients was aware of hypertension as a disease. The majority of the participants knew about the anti-hypertension medications they had been prescribed and remembered more than two recommendations for healthy lifestyle habits.
Characteristics of the control and intervention groups at the first visit to the healthcare clinic
| Variables | Intervention N=515 | Control N=481 | P value |
| Socio-demographic variables | |||
| Females (%) | 67.7 | 64.2 | .241 |
| Age; mean (SD) | 63.3 (8.1) | 63.4 (8.9) | .912 |
| Education | |||
| No formal education (%) | 67.2 | 61.7 | .150 |
| Primary school (%) | 25.8 | 28.9 | |
| Secondary school or university (%) | 7.0 | 9.4 | |
| Clinical data and treatment variables | |||
| Years since diagnosis; mean (SD) | 10.9 (8.3) | 9.9 (6.9) | .074 |
| Systolic blood pressure (mmHg); mean (SD) | 140.9 (16.2) | 139.3 (15.0) | .112 |
| Diastolic blood pressure (mmHg); mean (SD) | 82.5 (8.9) | 82.2 (8.8) | .704 |
| Patients with controlled hypertension (%) | 39.8 | 45.3 | .351 |
| Body mass index (kg/m2); mean (SD) | 30.2 (4.8) | 29.5 (4.3) | .022 |
| Number anti-hypertensive drugs; mean (SD) | 1.42 (0.63) | 1.36 (0.6) | .059 |
| Persons taking other drugs (%) | 66.6 | 63.6 | .348 |
| Total number of drugs; mean (SD) | 2.9 (1.7) | 2.6 (1.5) | .059 |
| Knowledge | |||
| Batalla test: knowledge of the hypertension (%) | 31.5 | 28.7 | .342 |
| Knowledge of hypertensive drugs (%) | 71.3 | 68.5 | .110 |
| Lifestyle recommendations; mean (SD) | 2.8 (1.4) | 2.7 (1.4) | .194 |
| Adherence | |||
| Haynes-Sackett test; adherence (%) | 95.5 | 96.9 | .318 |
| Morisky–Green test; adherence (%) | 75.1 | 75.7 | .877 |
| Self-reported adherence over 3 months; adherence (%) | 96.7 | 97.5 | .492 |
| Pill count; adherence (%) | 87.8 | 88.9 | .604 |
| Life-style recommendations followed; adherence (%) | 86.8 | 89.5 | .261 |
SD: standard deviation.
In relation to the self-declared compliance, there was a divergence of findings depending on the test employed; 4% of patients declared difficulties with compliance on the Haynes-Sackett test, whereas non-compliance was 25% with the Morisky-Green test, and 12% with pill counting.
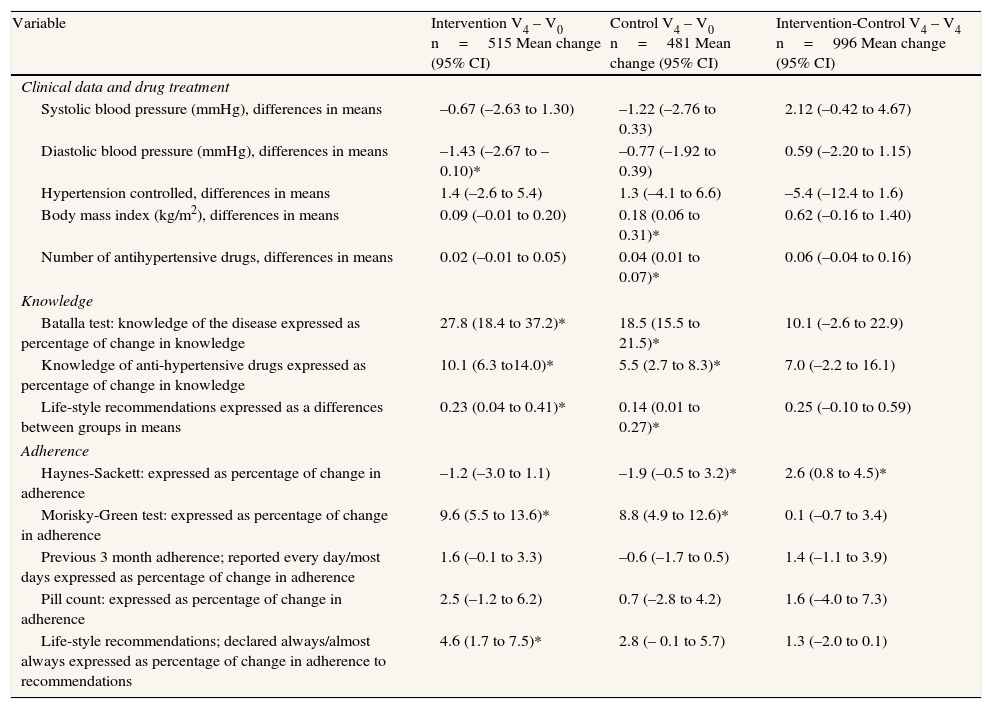
Table 2 summarises the changes observed within each group, presenting the intra-group differences (first and second columns in Table 2) comparing the data at the beginning and end of the study for each group separately, and inter-group differences (third column in Table 2) between the IG and the CG after 12 months of follow-up, including the 95%confidence interval (CI) of the difference. In both groups, all the variables in the awareness category improved significantly. The magnitude of the increase in knowledge of hypertension was much greater in the IG, according to the Batalla test. Indirect measures of adherence did not show improvement following the intervention, with the exception of the Morisky-Green test. At the end of the study, there were no statistically significant differences between the IG and CG groups, except in the Haynes-Sackett measure of adherence.
Differences within groups and between groups with respect to knowledge, compliance, and clinical variables
| Variable | Intervention V4 – V0 n=515 Mean change (95% CI) | Control V4 – V0 n=481 Mean change (95% CI) | Intervention-Control V4 – V4 n=996 Mean change (95% CI) |
| Clinical data and drug treatment | |||
| Systolic blood pressure (mmHg), differences in means | –0.67 (–2.63 to 1.30) | –1.22 (–2.76 to 0.33) | 2.12 (–0.42 to 4.67) |
| Diastolic blood pressure (mmHg), differences in means | –1.43 (–2.67 to –0.10)* | –0.77 (–1.92 to 0.39) | 0.59 (–2.20 to 1.15) |
| Hypertension controlled, differences in means | 1.4 (–2.6 to 5.4) | 1.3 (–4.1 to 6.6) | –5.4 (–12.4 to 1.6) |
| Body mass index (kg/m2), differences in means | 0.09 (–0.01 to 0.20) | 0.18 (0.06 to 0.31)* | 0.62 (–0.16 to 1.40) |
| Number of antihypertensive drugs, differences in means | 0.02 (–0.01 to 0.05) | 0.04 (0.01 to 0.07)* | 0.06 (–0.04 to 0.16) |
| Knowledge | |||
| Batalla test: knowledge of the disease expressed as percentage of change in knowledge | 27.8 (18.4 to 37.2)* | 18.5 (15.5 to 21.5)* | 10.1 (–2.6 to 22.9) |
| Knowledge of anti-hypertensive drugs expressed as percentage of change in knowledge | 10.1 (6.3 to14.0)* | 5.5 (2.7 to 8.3)* | 7.0 (–2.2 to 16.1) |
| Life-style recommendations expressed as a differences between groups in means | 0.23 (0.04 to 0.41)* | 0.14 (0.01 to 0.27)* | 0.25 (–0.10 to 0.59) |
| Adherence | |||
| Haynes-Sackett: expressed as percentage of change in adherence | –1.2 (–3.0 to 1.1) | –1.9 (–0.5 to 3.2)* | 2.6 (0.8 to 4.5)* |
| Morisky-Green test: expressed as percentage of change in adherence | 9.6 (5.5 to 13.6)* | 8.8 (4.9 to 12.6)* | 0.1 (–0.7 to 3.4) |
| Previous 3 month adherence; reported every day/most days expressed as percentage of change in adherence | 1.6 (–0.1 to 3.3) | –0.6 (–1.7 to 0.5) | 1.4 (–1.1 to 3.9) |
| Pill count: expressed as percentage of change in adherence | 2.5 (–1.2 to 6.2) | 0.7 (–2.8 to 4.2) | 1.6 (–4.0 to 7.3) |
| Life-style recommendations; declared always/almost always expressed as percentage of change in adherence to recommendations | 4.6 (1.7 to 7.5)* | 2.8 (– 0.1 to 5.7) | 1.3 (–2.0 to 0.1) |
V0: initial visit; V4: visit at 12 months.
The educational intervention carried out in this study was directed towards improving knowledge and adherence in individuals regularly attending an educational program during outpatient visits scheduled by the primary care nurse. The aim was to achieve better control of hypertension. The study population had a long history of hypertension and a high BMI. The strengths of the study were the larger than usual study sample13 and the 12-month intervention period, which was also longer than those reported in the literature. However, the outcomes of this study were negative. This could be partially explained by the study population characteristics and the intervention itself.
Regarding the study population, although adherence to prescribed medication and the non-pharmacological methods is a key element in the control of hypertension,3,4,25,26 the long-term evolution of the condition in our study population implied a high risk of non-adherence, since there is evidence that adherence decreases with time elapsed since diagnosis.9 Nevertheless, the level of non-compliance declared by the patients was much lower than that observed in other samples of hypertensive patients in Spain. A meta-analysis by Puigventós et al.17 of the studies carried out in Spain and using the Morisky-Green test for comparison indicated a percentage of self-declared non-compliers of 55%, whereas this was 25% in our study. This difference could be partially explained because our study sample included individuals who were regular attendees of the follow-up visits scheduled by the primary health-care team, and who had a long history of hypertension, and the questionnaire was administered at their own health-care centre. In fact, the prevalence of non-adherence in hypertension has been considered highly dependent on the study population.15
Baseline data indicated that a control of hypertension of 40% was lower than that observed in other studies conducted in Spain as part of the MONICA project,27 indicating that there was room for improvement. However, after the intervention, no improvement in the control of the hypertension was observed. Studies performed in Spain that impacted compliance and control of hypertension were those focusing on recently-diagnosed patients with high blood pressure and, as such, were more likely to be predisposed towards greater adherence. Our results are consistent with the small effects of interventions aimed at improving adherence, with HTA observed in two meta-analysis,28,29 a recent review15, or in chronic conditions in general.30 However, the results obtained in this study, especially the sub-optimal control of blood pressure and the elevated BMI, underline the need for specific interventions with special emphasis on diet and exercise, which are not easy to carry out effectively in practice.31
The intervention was planned within the context of standard clinical practice and the criteria suggested by Haynes et al.13 This study was carried out with the aim of ease of application in the primary care setting, >80% follow-up of patients, and with clinically relevant outcomes in a large sample population that was maintained over a relatively long period. Our intervention was directed towards inducing a higher level of knowledge and behavioural changes in the patient, mostly through an intervention delivered by a trained nurse on the primary care team,32 which has been shown to be feasible but ineffective in HTA patients with long term evolution of the condition.
Several limitations of this study should be considered. Firstly, contamination of the CG. The majority of the outcomes improved in both groups over the 12-month follow-up. The randomization to the intervention according to the Primary Health-care Centre decreases the possibility of contamination between the groups; also, cluster randomisation was taken into account in the analysis. However, the administration of the follow-up questionnaire at each clinic visit, the protocol of scheduled clinic visits in both groups, and the effect of participating in a clinical trial could explain the improvements observed in the CG.33 Secondly, the nurse-led intervention had the advantage of proximity to the patient, but also the long-term clinical relationship these patients had with their nurse provider could have made changing their behaviour, which had been present for several years, during the study period difficult. Thirdly, it is clear that measures of adherence are not consistent, and it is not clear which of the instruments currently available is the most appropriate.16,34,35
In conclusion, our study evaluated an intervention based on repeated information given to the HTA patient by the clinic nurse within a primary care setting with negative results regarding HTA adherence and control. Further studies are warranted to define and reinforce adherence, and to design more specific interventions directed towards improving adherence among long term HTA patients in the primary health care framework that are feasible and easy to apply in every day practice.
ContributorsEAG and JMB planned the study, discussed the results and wrote the manuscript. EP and VPG analysed the data, discussed the results, and contributed to the writing of the manuscript. All authors reviewed and approved the final version of the manuscript. EAG and VPG had full access to the data used in this manuscript, and take the responsibility for the integrity of the data and accuracy of the data analysis.
Conflict of interestNone declared.
The long-term funding of the project came from the Fundación Jordi Gol i Gurina. The present study was funded by a grant from the Agency for the Evaluation of Medical Technology and Research [Agencia de Evaluación de Tecnología Médica y de Investigación; AATMR 2/51/98]. Also, support from the Instituto de Salud Carlos III is acknowledged (RD06/0020/089)