To analyze changes in users’ awareness of the healthcare system and of their rights to healthcare in Colombia in the last 10 years, as well as the factors that influence users’ awareness.
MethodsWe carried out a descriptive study to compare the results of two cross-sectional studies based on two surveys of users of the Colombian healthcare system. The first survey was performed in 2000 and the second in 2010. The municipalities of Tuluá (urban area) and Palmira (rural area) were surveyed. In both surveys, a stratified, multistage probability sample was selected. There were 1497 users in the first sample and 1405 in the second. Changes in awareness of the healthcare system and associated factors in each year were assessed through multivariate logistic regressions.
ResultsUsers’ awareness of the healthcare system was limited in 2000 and was significantly lower in 2010, except for that relating to health insurers and providers. In contrast, more than 90% of users in both surveys perceived themselves as having healthcare rights. The factors consistently associated with greater awareness were belonging to a high socioeconomic stratum and having higher education.
ConclusionsThe most underprivileged users were less likely to be aware of the healthcare system, hampering their ability to make informed decisions and to exercise their health rights. To correct this situation, health institutions and the government should act decisively to reduce social inequalities.
Analizar cambios en el conocimiento y en los factores que influyen en este conocimiento de los usuarios del sistema de salud (SGSSS) y de sus derechos a la atención en salud en Colombia en los últimos 10 años.
MétodosEstudio descriptivo que compara resultados de dos estudios transversales basados en dos encuestas realizadas a usuarios del sistema de salud de Colombia, una en 2000 y otra en 2010. El área de estudio fueron los municipios de Tuluá (zona urbana) y Palmira (zona rural). En ambas encuestas se realizó un muestreo probabilístico estratificado multietápico, conformándose en la primera una muestra de 1497 usuarios y en la segunda de 1405. Se analizó el cambio en el conocimiento y los factores asociados en cada año mediante regresión logística multivariada.
ResultadosEl conocimiento del sistema de salud en 2000 era limitado y en 2010 disminuyó significativamente, excepto en relación con las aseguradoras y los proveedores. En contraste, los resultados muestran que más del 90% de los usuarios en ambas encuestas se perciben poseedores del derecho a la atención en salud. Pertenecer a estratos socioeconómicos altos y estudios superiores se asocia consistentemente a un mayor grado de conocimiento.
ConclusionesLos usuarios más desfavorecidos tienen menor posibilidad de conocer el SGSSS, lo cual es una barrera para tomar decisiones informadas y para hacer cumplir y ejercer sus derechos a la salud. Para revertir esta situación es necesaria una intervención decidida de las instituciones de salud, así como del gobierno en general, para reducir las inequidades sociales.
During the late 1980s and 1990s, and under the influence of multilateral organizations like the World Bank and the International Monetary Fund,1 numerous nations undertook reforms based on market models in their social sectors, including healthcare; Colombia was not removed from this. Thus, in 1993 the General System of Social Security in Health (Sistema General de Seguridad Social en Salud, SGSSS) was created,2 frameworked in the Political Constitution of 1991,3 that did not grant healthcare the status of a fundamental human right but regarded it merely as an essential public service of obligatory compliance to be provided under state direction, coordination, and control. Stated principles of the SGSSS are2: universality, solidarity, comprehensiveness, equity, freedom of choice of health insurer and of healthcare provider, quality of service, and social participation.
With this reform, Colombia became one of the first middle-income countries to adopt a model of managed competition.4 It created an extraordinarily complex healthcare system, made up of two insurance schemes: the contributory regime, for formal-sector employees and individuals with ability to pay, financed by mandatory contributions; and subsidized regime, for people unable to pay, funded by resources from the contributory scheme and other sources of financing, such as taxes. Health insurers were introduced to manage the contributory regime (empresas promotoras de salud, EPS) and the subsidized regime (empresas promotoras de salud - subsidiadas, EPS-S). Private insurers compete to enrol the population and public and private healthcare providers (instituciones prestadoras del servicio, IPS) for contracts with insurers. In 1994, a comprehensive policy for social participation in health was also formulated, which established participation in management, planning, and evaluation at various levels: from information to decision making5 and through different types of health participation: citizen participation (based on a market approach), community participation and participation within healthcare institutions. In neoliberal models, participation is central: private enterprises are called upon to participate in managing and providing services, and citizens to participate, among others, in quality control: the latter is the focus of this article.
Users’ awareness of the healthcare system, and of their rights to healthcare, empowers them for effective interaction with health services: for participating in various aspects of the healthcare system6; for making informed health decisions7;8; as well as for accessing services9 and hence, it is one of the fundamental conditions for users to exercise their right to healthcare,10 among others.
Therefore, user awareness of the healthcare system and policies, and of their rights are relevant social determinants of healthcare use, which are closely related to other social determinants, such as socioeconomic level, education levels, gender, and living in rural or urban areas, among others, and can lead to inequities in health.11,12 Nevertheless, analysis of user awareness has been limitedly conducted, in general.6 This also applies to Latin America with few researches available on user awareness of healthcare systems, their functioning, or their healthcare rights. Studies conducted in Colombia indicate that individuals of higher socioeconomic and education levels are those that best know the SGSSS,13 and their right to healthcare.14 Moreover, according to a recent analysis,15 user's awareness of mechanisms for social participation in health in Colombia did not improve, but rather, tended to diminish during the last decade. This article seeks to analyze changes in factors that influence the users’ awareness of the SGSSS and their rights to health care in Colombia in the last ten years.
MethodsDesignThis descriptive study analyses trends16 based on two cross-sectional studies carried out by means of two surveys among healthcare users who had used services within three months prior to the survey in 2000 and 2010.
Area of the studyThe study area comprised two municipalities in the Department of Valle del Cauca in Colombia's Southwest: Tuluá, with 194,446 inhabitants and Palmira with 294,800 inhabitants.17 Selection criteria were: having implemented the reform of the healthcare sector; including populations from all socioeconomic levels; high percentages of enrolment to the SGSSS; provision of all care levels; and, rural and urban areas.
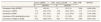
SamplingSample size was calculated based on population size and expected rate of use of health participation mechanisms (estimated at 24% in year 2000, according to the pilot study, and at 25% in year 2010, according to results from the year 2000 study) and yielded a 95% confidence interval (95%CI) with 3% precision. The final sample was 1495 users in 2000; and 1405 users in 2010. The final sample comprised male and female users from different ages, socioeconomic and educational levels, and occupations (Table 1).
Socio-demographic characteristics of the samples: 2000 and 2010.
| Survey 2000 | Survey 2010 | |||
| N=1495 | N=1405 | |||
| n | (%) | n | (%) | |
| Area | ||||
| Rural | 727 | (48.6) | 689 | (49) |
| Urban | 768 | (51.4) | 716 | (51) |
| Sex | ||||
| Male | 543 | (36.3) | 618 | (44) |
| Female | 952 | (63.7) | 787 | (56) |
| Socio-economic level | ||||
| Low | 635 | (42.7) | 992 | (71) |
| Medium | 626 | (41.8) | 282 | (20) |
| High | 235 | (15.6) | 131 | (9) |
| Education level | ||||
| No schooling-primary | 702 | (47.8) | 918 | (65.4) |
| Intermediate | 628 | (42.8) | 426 | (30.3) |
| University | 138 | (9.4) | 61 | (4.3) |
| Age (years) | ||||
| 13-19 | 92 | (6.2) | 79 | (5.3) |
| 20-30 | 311 | (20.9) | 272 | (19.4) |
| 31-40 | 337 | (22.6) | 345 | (24.6) |
| 41-65 | 587 | (39.4) | 564 | (40.6) |
| >65 | ||||
In both surveys, a stratified multistage probability sampling was conducted. In the first stage, neighborhoods –in the urban area–, and corregimientos (villages) in rural areas from different socioeconomic levels were randomly selected, without replacement. In the second stage, users were systematically selected. The sample range was calculated according to sample size and number of homes in each neighborhood; the initial home was randomly selected. The home was considered the primary sampling unit to avoid the effect of associated samples18 in individuals belonging to a family. Efforts were made to interview the same number of men and women.
QuestionnaireFor the 2000 survey, the questionnaire was adapted from a previous study19 which was discussed with experts, and prior to its final version, it was submitted to a pretest and two pilot studies. It was a five-section structured questionnaire referring to: a) perceived quality of the services; b) awareness of the Healthcare System, participation policy, and healthcare rights; c) awareness of participation mechanisms; d) utilization and experience with such; e) a participation attitudes scale. For the second survey, questions on perceived healthcare quality were eliminated. In this article, we analyze responses from part b of the questionnaire.
Data collectionData were collected through face-to-face interviews conducted over weekends to increase the probability of finding adults at home for the interview. Previously trained psychology students carried out the interviews. Because this was a minimum-risk study, and pursuant to Resolution 8430 of 1993, each person was required an oral informed consent for the interview, and protection and confidentiality of data was guaranteed by treating and analyzing them anonymously.
VariablesThe outcome (dependent) variables were: awareness level of the SGSSS –regarding basic characteristics of the SGSSS, characteristics and functions of health insurers (EPS), healthcare providers (IPS) and participation policy– and awareness of healthcare rights. It was defined that an individual was aware of the SGSSS when, besides responding affirmatively to the question “Do you know the SGSSS?”, in the question “Can you tell me what you know?”, these individuals described at least three basic characteristics (a third) of the SGSSS. Likewise, a person was defined with awareness when able to describe at least two (a third) main functions for questions “What are health insurers for (EPS)?” and “What are healthcare providers for (IPS)?”. Although awareness of EPS and IPS is part of being aware of the SGSSS, these questions are treated separately in the analysis because they are the institutions with which users interact on a regular basis in healthcare services. It was defined that an individual was aware of the participation policy when, besides responding affirmatively to the question “Do you know any policy for social participation in the healthcare system?”, these individuals mentioned at least one of the existing norms (the policy for social participation, Act 100, the Political Constitution). Also, they were asked “What do you consider are your healthcare rights?”, giving them free options to answer. Explanatory (independent) variables were: area (rural, urban), sex (male, female), socio-economic level of the home (low, middle, high) declared by the informant (based on the classification of the Municipal Planning office) and level of education (no schooling- primary, intermediate, university).
Data analysisThrough a univariate analysis, frequencies and percentages were estimated for each year. Further, we estimated three logistic regression models: one to compare changes in levels of knowledge for both years together (2000 as reference and adjusted by all other explanatory variables); and one for each year to determine factors associated with the level of awareness of the SGSSS and of health rights, setting p<0.05 and a 95%CI as significance criteria. Data were analyzed with SPSS v 17.
Data qualityAll questionnaires were individually reviewed in both surveys and 15% were randomly re-interviewed in the first, and 20% in the second, to analyze response consistency. Inconsistencies were not detected. During data entry, inconsistencies were controlled through the double-entry method, enabling automatic revision of inconsistencies.
ResultsIn the 2000 survey, 51.4% of respondents resided in urban areas; 63.7% were female; 42.7% reported to belong to the lower socioeconomic strata; and 47.8% had no schooling or primary education. In the 2010 survey, 51% resided in urban areas; 56% were female; 71% reported to belong to the lower socioeconomic strata and 65.4%, had no schooling or primary education (Table 1).
Changes in level of awareness of the SGSSS and of healthcare rightsA low level of awareness of the SGSSS, of EPSs, of IPSs, and of the participation norm is noted in the results of both surveys. In 2000, approximately 12% of participants were aware of some system's characteristics (they mentioned at least three), while in 2010 only 8% (Fig. 1). Moreover, responses provided tended to be quite limited, describing very general characteristics of the SGSSS like “to offer healthcare services for everyone”, “to provide healthcare for the poor”, or “you must have your membership card”. Freedom of choice of healthcare institutions or the right to participate in health was only rarely mentioned; in 2010, awareness of healthcare institutions had slightly increased –EPS 14.6% and IPS 15.4% versus EPS 11.3% and IPS 11.7% in 2000– (Table 2). The level of awareness of social participation in health norms was 9.4% in 2000, and 6.1% in 2010. Also, for the question “What do you consider are your healthcare rights?”, more than 90% in both surveys mentioned some rights, and the most common response continued being, the right to health care: “to receive healthcare” and “to be attended to”, 61% in 2000 and 68.3% in 2010; relating the rest to some aspects of health care. Participation was rarely mentioned as a healthcare right (Fig. 1). In the logistical regression model, differences in levels of knowledge between both years were statistically significant, once adjusted by the other explanatory variables (area, sex, level of education and socioeconomic strata) except in the knowledge of healthcare rights (Table 2).
Change in the level of awareness: bivariate (prevalence and confidence interval of awareness) and multivariate association between awareness and year.
| Survey 2000N=1495 | Survey 2010N=1405 | aOR | (95%CI) | |||
| % | (95%CI) | % | (95%CI) | |||
| Awareness of the SGSSS | 12 | (10-14) | 8 | (5-11.4) | 0.90 | (0.88-0.98) |
| Awareness of EPSs | 11.3 | (8.9-13.9) | 14.6 | (10.5-18.7) | 1.71 | (1.12-2.23) |
| Awareness of IPSs | 11.7 | (9.1-14.1) | 15.4 | (11.2-19.4) | 1.20 | (1.05-1.69) |
| Awareness of the participation norm | 9.4 | (7.2-11.6) | 6.1 | (3.3-8.9) | 0.65 | (0.47-0.89) |
| Awareness of rights to health | 91.5 | (89.2-93.5) | 89.5 | (87.7-91.2) | 0.98 | (0.95-1.02) |
Reference level year 2000.
aOR: odds ratios adjusted for area, sex, socioeconomic and educational level; 95%CI: confidence interval of 95%; SGSSS: general system of social security in health; EPS: health insurers; IPS: healthcare providers.
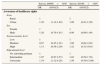
In 2000, being female, having a low socioeconomic and educational level was significantly associated with lower odds of knowing the SGSSS (Table 3). In 2010, being from rural areas, having a low socioeconomic and educational level, was associated with lower odds of knowing the SGSSS (Tables 3 and 4).
Factors associated with awareness of SGSSS in 2000 and 2010.
| Survey 2000N=1495 | Survey 2010N=1405 | |||
| OR | (95%CI) | OR | (95%CI) | |
| Awareness of SGSSS | ||||
| Area | ||||
| Rural | 1 | 1 | ||
| Urban | 1.10 | (0.59-1.21) | 1.47 | (1.18-1.96) |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 2.11 | (1.58-2.83) | 1.04 | (0.74-1.48) |
| Socioeconomic level | ||||
| Low | 1 | 1 | ||
| Medium | 1.36 | (0.89-1.58) | 1.23 | (1.04-1.56) |
| High | 2.06 | (1.26-2.12) | 2.85 | (1.44-8.65) |
| Educational level | ||||
| No schooling-primary | 1 | 1 | ||
| Intermediate | 2.72 | (1.92-3.85) | 2.02 | (1.27-3.20) |
| University | 10.00 | (7.27-18.98) | 9.09 | (5.67-15.35) |
| Awareness of EPS | ||||
| Area | ||||
| Rural | 1 | 1 | ||
| Urban | 1.11 | (0.62-1.24) | 1.03 | (0.81-1.13) |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 1.09 | (0.88-1.62) | 0.91 | (0.53-1.55) |
| Socioeconomic level | ||||
| Low | 1 | 1 | ||
| Medium | 0.90 | (0.83-1.64) | 1.28 | (1.07-1.45) |
| High | 1.12 | (0.89-2.06) | 2.14 | (1.10-7.25) |
| Educational level | ||||
| No schooling-primary | 1 | 1 | ||
| Intermediate | 1.57 | (1.13-2.17) | 3.02 | (1.12-6.18) |
| University | 3-21 | (1.15-4.18) | 11.03 | (2.84-18.04) |
| Awareness of IPS | ||||
| Area | ||||
| Rural | 1 | 1 | ||
| Urban | 1.13 | (0.68-1.46) | 1.12 | (0.81-1.41) |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 1.12 | (0.95-1.55) | 0.94 | (0.83-2.00) |
| Socioeconomic level | ||||
| Low | 1 | 1 | ||
| Medium | 0.80 | (0.61-1.05) | 1.33 | (1.08-1.68) |
| High | 1.36 | (1.02-1.42) | 1.80 | (1.42-6.55) |
| Educational level | ||||
| No schooling-primary | 1 | 1 | ||
| Intermediate | 1.94 | (1.26-2.13) | 3.22 | (1.39-4.66) |
| University | 4.78 | (1.71-6.02) | 4.28 | (2.56-9.22) |
| Awareness of norm | ||||
| Area | ||||
| Rural | 1 | 1 | ||
| Urban | 0.58 | (0.39-0.87) | 0.90 | (0.79-1.24) |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 1.77 | (1.22-2.57) | 1.08 | (0.54-1.52) |
| Socioeconomic level | ||||
| Low | 1 | 1 | ||
| Medium | 1.38 | (1.08-1.72) | 1.50 | (1.06-2.83) |
| High | 2.04 | (1.79-2.34) | 3.83 | (1.48-9.90) |
| Educational level | ||||
| No schooling-primary | 1 | 1 | ||
| Intermediate | 2.01 | (1.28-3.14) | 3.55 | (1.58-7.98) |
| University | 5.49 | (3.05-9.88) | 6.04 | (1.95-14.68) |
OR: odds ratio; 95%CI: confidence interval of 95%; SGSSS: general system of social security in health; EPS: health insurers; IPS: healthcare providers.
Factors associated with levels of awareness of healthcare rights in 2000 and 2010.
| Survey 2000N=1495 | Survey 2010N=1405 | |||
| OR | (95%CI) | OR | (95%CI) | |
| Awareness of healthcare rights | ||||
| Area | ||||
| Rural | 1 | 1 | ||
| Urban | 1.39 | (1.14-1.65) | 1.09 | (0.43-1.20) |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 1.20 | (0.79-1.81) | 0.98 | (0.66-1.46) |
| Socioeconomic level | ||||
| Low | 1 | 1 | ||
| Medium | 0.67 | (0.45-1.01) | 1.09 | (0.64-3.02) |
| High | 1.13 | (0.58-2.20) | 1.22 | (0.32-10.6) |
| Educational level | ||||
| No schooling-primary | 1 | 1 | ||
| Intermediate | 1.07 | (0.87-2.57) | 1.03 | (0.59-1.70) |
| University | 1.34 | (1.12-4.28) | 1.50 | (0.39-13.86) |
OR: odds ratio; 95%CI: confidence interval of 95%.
In the year 2000, having no schooling or primary education was significantly associated with a lower odds of knowing EPSs than users of higher education levels (Table 3). In 2010, users of lower educational and socioeconomic levels had lower odds of knowing EPSs (Table 3).
Factors associated with awareness of health providers (IPSs)In 2000, being a user with low and medium socioeconomic and educational levels was associated with lower odds of knowing them (Table 3). In 2010, users of lower educational and socioeconomic levels had lower odds of knowing IPSs.
Factors associated with awareness of the social participation normIn 2000, being from urban areas, being a woman, belonging to low socioeconomic and educational levels, was associated with lower odds of knowing the standard (Table 3). In 2010 only belonging to middle and low socioeconomic strata and having no schooling/primary or secondary education was associated with lower odds of knowing the social participation norm.
Factors associated with awareness of rights to health servicesIn 2000, belonging to rural areas and not having an education or having a basic education, was significantly associated with lower odds of knowing their rights to health services (Table 4). In 2010, all users presented a high level of awareness of rights in health services, without observing any factor significantly associated with this fact (Table 4).
The logistic analysis of both samples together show a trend of factors associated with awareness, similar to that which was noted in the models for each year (Table 5).
Factors associated with the level of awareness in the analysis of both samples together.
| OR | (IC 95%) | |
| Awareness of SGSSS | ||
| Area | ||
| Rural | 1 | |
| Urban | 1.26 | (1.06-1.52) |
| Sex | ||
| Female | 1 | |
| Male | 1.59 | (1.27-1.99) |
| Socioeconomic level | ||
| Low | 1 | |
| Medium | 1.63 | (1.26-2.03) |
| High | 3.24 | (2.48-4.35) |
| Educational level | ||
| No schooling-primary | 1 | |
| Intermediate | 2.2 | (1.36-3.56) |
| University | 5.28 | (2.84-12.09) |
| Year | ||
| 2000 | 1 | |
| 2010 | 0.9 | (0.88-0.98) |
| Awareness of EPS | ||
| Area | ||
| Rural | 1 | |
| Urban | 1.12 | (0.87-1.42) |
| Sex | ||
| Female | 1 | |
| Male | 1.05 | (0.81-1.36) |
| Socioeconomic level | ||
| Low | 1 | |
| Medium | 1.28 | (1.02-1.74) |
| High | 1.98 | (1.41-2.79) |
| Educational level | ||
| No schooling-primary | 1 | |
| Intermediate | 2.75 | (1.52-4.94) |
| University | 4.18 | (2.08-8.39) |
| Year | ||
| 2000 | 1 | |
| 2010 | 1.51 | (1.12-2.23) |
| Awareness of IPS | ||
| Area | ||
| Rural | 1 | |
| Urban | 1.02 | (0.38-1.62) |
| Sex | ||
| Female | 1 | |
| Male | 1.15 | (0.93-1.42) |
| Socioeconomic level | ||
| Low | 1 | |
| Medium | 1.05 | (0.58-1.02) |
| High | 1.56 | (1.10-2.23) |
| Education level | ||
| No schooling-primary | 1 | |
| Intermediate | 1.57 | (1.31-2.95) |
| University | 3.46 | (2.05-5.83) |
| Year | ||
| 2000 | 1 | |
| 2010 | 1.2 | (1.05-1.69) |
| Awareness of norm | ||
| Area | ||
| Rural | 1 | |
| Urban | 0.7 | (0.32-0.94) |
| Sex | ||
| Female | 1 | |
| Male | 1.39 | (1.03-1.87) |
| Socioeconomic level | ||
| Low | 1 | |
| Medium | 1.11 | (0.75-1.64) |
| High | 1.8 | (1.11-2.93) |
| Educational level | ||
| No schooling-primary | 1 | |
| Intermediate | 3.42 | (1.58-7.42) |
| University | 8.51 | (3.62-20.00) |
| Year | ||
| 2000 | 1 | |
| 2010 | 0.65 | (0.47-0.89) |
| Awareness of healthcare rights | ||
| Area | ||
| Rural | 1 | |
| Urban | 1.13 | (1.02-0.24) |
| Sex | ||
| Female | 1 | |
| Male | 1.1 | (0.83-1.46) |
| Socioeconomic level | ||
| Low | 1 | |
| Medium | 0.89 | (0.64-1.68) |
| High | 1.12 | (1.04-3.41) |
| Educational level | ||
| No schooling-primary | 1 | |
| Intermediate | 1.1 | (0.94-3.25) |
| University | 1.25 | (1.02-3.67) |
| Year | ||
| 2000 | 1 | |
| 2010 | 0.98 | (0.95-1.01) |
SGSSS = General System of Social Security in Health; EPS = Health insurers; IPS = Healthcare providers. Source: author's.
Reforms to healthcare systems that are based on the application of market mechanisms to improve service quality include, as an inherent element, good awareness and information of users about the healthcare system to participate in its control and to make informed decisions, in addition to accessing the services and to demand their rights. The results of this study show that in the last ten years, and 17 years after the implementation of the SGSSS in Colombia, the level of awareness of the healthcare system is limited and shows a tendency to decrease; only a small improvement was observed in the awareness of health insurers and providers, which was expected as they are the institutions with which users relate to on a daily basis in pursuit of healthcare. The most underprivileged –in general terms– are those with lower odds to be aware of the SGSSS and its institutions. This result indicates a major weakness of the system, which contradicts its fundamental principles. Previous studies19,20 about awareness of participation in health, conducted in Colombia, had observed very limited “users’ awareness” of the healthcare system. The results of this study also show that few users –with a tendency to decrease in the second survey– are aware of the existence of a norm that establishes the right to participate in the control of the system, in accordance to previous studies19,21; these users were men in the high and medium socioeconomic level, and higher and intermediate education. These indicate that awareness of the SGSSS and of the opportunities for participation in its control in order to influence, among others, the quality of healthcare services, is far from improving, and even less in low-income groups. This is especially relevant, considering that these population groups are precisely the ones which suffer most from healthcare services of poor quality, as demonstrated by several studies.1,22–24
Awareness of the healthcare system and its functioning is also a determinant of access to services, with limited awareness being a significant barrier to care.9 The results of this study show that the most disadvantaged groups (those of low socioeconomic and educational levels) are the ones who are the least likely of being aware of the SGSSS, in both surveys. The most disadvantaged population groups are also those who face the greatest barriers to accessing healthcare services.22,24–26 Thus, these results seem to indicate a tendency to increase inequities in access to healthcare, as users of higher strata and educational levels, besides having a better understanding of the SGSSS, tend to improve it, meaning probably a better relationship with it. This probably relates to the perception of users of upper strata of no barriers to access, found in another study.27
The limited awareness of the SGSSS that is broadly observed in this study also indicates, that health authorities and institutions responsible for promoting awareness and keeping users informed, as established by the Ministry of Health,28 still do not comply with this function, and that State agencies responsible for monitoring that these tasks are carried out, do not comply either.1,24,29 These results are in concordance with some studies of recent years that suggest little call for users to know the system, its functions, norms, and participation mechanisms, among others, both on the part of the SGSSS's institutions as well as on the local authorities.14,29–31
Fundamental rights have been socially and progressively built based on perceptions, life experiences, and above all, on the concept of human nature that individuals and social groups have developed.32 Thus, from the individual consciousness built in modernism, fundamental rights are currently presented as universal, that is, extensive to all members of society and supported by the moral principle of equal respect that all people deserve due to their human nature.33 But the validity of fundamental rights in a particular society32 will be given by three circumstances: by the strength of the collective consciousness of its existence; by the ability of society to create a must be or a recognition of rights in the legal order; and, by the ability of social groups to enforce them and exercise them in everyday's life. In our results, in contrast with the limited awareness of the SGSSS, the vast majority of users, about 90% in both surveys, reveal an awareness of some healthcare rights, but above all, of their right to receive healthcare (more than 60%); which clearly coincides with a recent study in Colombia.14 The understanding of the inter-subjective elements and processes, based on which users of the SGSSS, without knowing it well symbolically build their health rights, those which often are denied to them, requires further research.
In conclusion, after 17 years of the SGSSS implementation, users, and above all the most underprivileged, still do not know it, similarly to what had happened in other low income countries.34 This limited awareness not only weakens users individually for accessing services, but also weakens them politically as key players of the system when it comes to participating in its control. In contrast, an element that favors the possibility of exercising the right to healthcare in Colombia is awareness of it among a vast users’ majority; which has been recently strengthened also in the legal field, with recognition of healthcare as a fundamental right.35 The empowerment of the user begins with their awareness, and in order to redress the inequality of awareness of the healthcare system –which affects access and the quality of health services for people who are the most underprivileged–, it is urgent that health institutions comply with their constitutional obligation of informing users. Moreover, governments of low and middle income countries, such as Colombia, should begin to introduce effective measures outside the health sector12; to fight the unequal distribution of power, to improve opportunities to access education and worthy and better paid employment for men and women in order to achieve better health for all.
In any healthcare system, but particularly in those based on market mechanisms –managed competition, as is the case of Colombia–, the awareness of users about the system, the policies, and their rights to healthcare, are essential for making informed decisions about their health and the choice of insurer and service provider, in order to access services and, ultimately, to exercise their right to healthcare. However, studies conducted on the awareness of users of the healthcare system are very limited and specific in nature. Few studies in Colombia indicate that users from higher socioeconomic strata, and with higher education levels, are the ones who know the most about the SGSSS and their rights to healthcare.
What does this study add to the literature?This study presents the first analysis of the evolution of factors that influence awareness of the General System of Social Security in Health in Colombia, based on managed competition. The results show, those 17 years after the reform, users’ awareness necessary to influence it and use it is still low and even less in the most underprivileged. These results also question the model's ability to improve inequalities in access to healthcare and point to the need to deepen into the factors that are limiting the process, and developing policies and strategies for redressing it.
M.E. Delgado Gallego has contributed to the study conception, design, implementation and interpretation of data analysis and the writing of the paper, she was also responsible for the supervision of the fieldwork. M.L. Vázquez-Navarrete has contributed to the study conception, design and implementation, the supervision of all phases of the research and the writing of the article.
FundingThis research was partially financed by Universidad del Valle and the DG XII European Commission (IC18-CT98-0340).
Conflicts of interestsNone.
The 2000 survey was part of the research conducted by the Institute of Psychology at Universidad del Valle (Colombia) in association with the Institute for Health Sector Development (UK), Universidad Federal de Pernambuco and Instituto Materno Infantil de Pernambuco (IMIP Brazil), Escuela Andaluza de Salud Pública (Spain) and with the collaboration from the Consorci Hospitalari de Catalunya (now Consorci de Salu ti Social de Catalunya), the Health Secretaries of the municipalities of Tuluá and Palmira in Colombia, and the Secretary of Health of the Department of Valle del Cauca in Colombia. We thank Irene García for her advise on the statistical analysis and the two anonymous reviewers for their comments of the previous versions that contributed to improve the paper all people interviewed in these two municipalities who accepted to share their opinions, ideas, and experiences with the researchers.