To estimate the waiting time since a suspected an occupational disease (OD) is identified, notified and recognized in Spain.
MethodA series of 34 patients attended at Occupational Diseases Unit (ODU) of Hospital del Mar in Barcelona were follow up since their identification until final resolution by the National Institute of Social Security (INSS). Median, and 25 and 75 percentiles (interquartile range [IQR]) were calculated in weeks by total time (n=27), ODU time (n=34), patient time (n=31) and INSS time (n=27).
ResultsTotal time was 51 weeks (IQR: 33.6 and 122.6), of which 42 weeks (17.6-99.5) corresponded to the waiting period at the INSS.
ConclusionsThe disproportionately long waiting time since INSS receives a case could impact on the under-recognition of OD. Urgent improvement of the administrative process is needed to reduce the patient waiting time for the recognition of OD.
Estimar el tiempo de espera desde que se identifica hasta que se notifica y reconoce una enfermedad profesional (EP) en España.
MétodoSe siguió a una serie de 34 pacientes atendidos en la Unidad de Enfermedades Profesionales (UPL) del Hospital del Mar de Barcelona, desde su identificación hasta la resolución por parte del Instituto Nacional de la Seguridad Social (INSS). Se calcularon las medianas y los percentiles 25 y 75 (rango intercuartílico [RIC]) en semanas para el tiempo total (n=27), el tiempo UPL (n=34), el tiempo paciente (n=31) y el tiempo INSS (n=27).
ResultadosEl tiempo total fue de 51 semanas (RIC: 33,6-122,6), de las que 42 semanas (17,6-99,5) correspondieron al periodo de espera en el INSS.
ConclusionesLa larga espera para la resolución del INSS podría impactar en el infrarreconocimiento de las EP. Es urgente mejorar el proceso administrativo para reducir el tiempo de espera de los pacientes para el reconocimiento de las EP.
Occupational disease (OD) usually refers to both a medical and legal concept.1,2 In Spain, as in other countries, the procedure for recognition is open to several stakeholders and a suspected case of occupational disease (OD) can be reported to the National Institute of Social Security (INSS Spanish acronym) by the patient once a physician from the National Health Service identified a suspected OD.3 The final resolution by the INSS, recognising or not, close the administrative process.
Recognition has important implications, including economic benefits equivalent to 100% of the salary base, coverage of all health expenses, economic bonus to the company when workplace adjustments are made, and improvement of working conditions to protect workmates.4 However, OD underreporting is common in Spain and in other countries.5
Since 2010, the Hospital del Mar (Barcelona, Spain) has an Occupational Disease Unit (ODU), where all clinicians can refer their patients if they suspect that their disease was caused by exposures at work. When a suspected occupational disease is identified by the ODU, patients are encouraged to notify it to INSS for recognition. We analysed the time elapsed since a suspected OD is identified by the ODU until final resolution by the INSS.
MethodThis study is a cases series of 34 patients with respiratory cancer (n=18) and musculoskeletal disorders (MSD) (n=16) who were identified by the ODU at Hospital del Mar as suspected cases of OD.3 Twenty-three were male (17 respiratory cancers and 6 MSD), 22 were younger than 70 years (6 respiratory cancers and 16 MSD) and 23 were manual workers (12 respiratory cancers and 11 MSD). Of those, 31 patients started the process for OD recognition and 27 had a final resolution by the INSS.
The “total time” was defined as the period elapsed since a patient was identified by the ODU until final resolution by INSS (n=27), and it was divided into three subperiods: 1) “ODU time” as the period while the ODU evaluated the patients to confirmed the suspected OD (n=34); 2) “patient time” as time it took the patient to decide and report his/her case to the INSS (n=31); and 3) “INSS time” as the time elapsed while INSS evaluated the case until final recognition, or not, the OD (n=27). Percentages were calculated regarding the previous step.
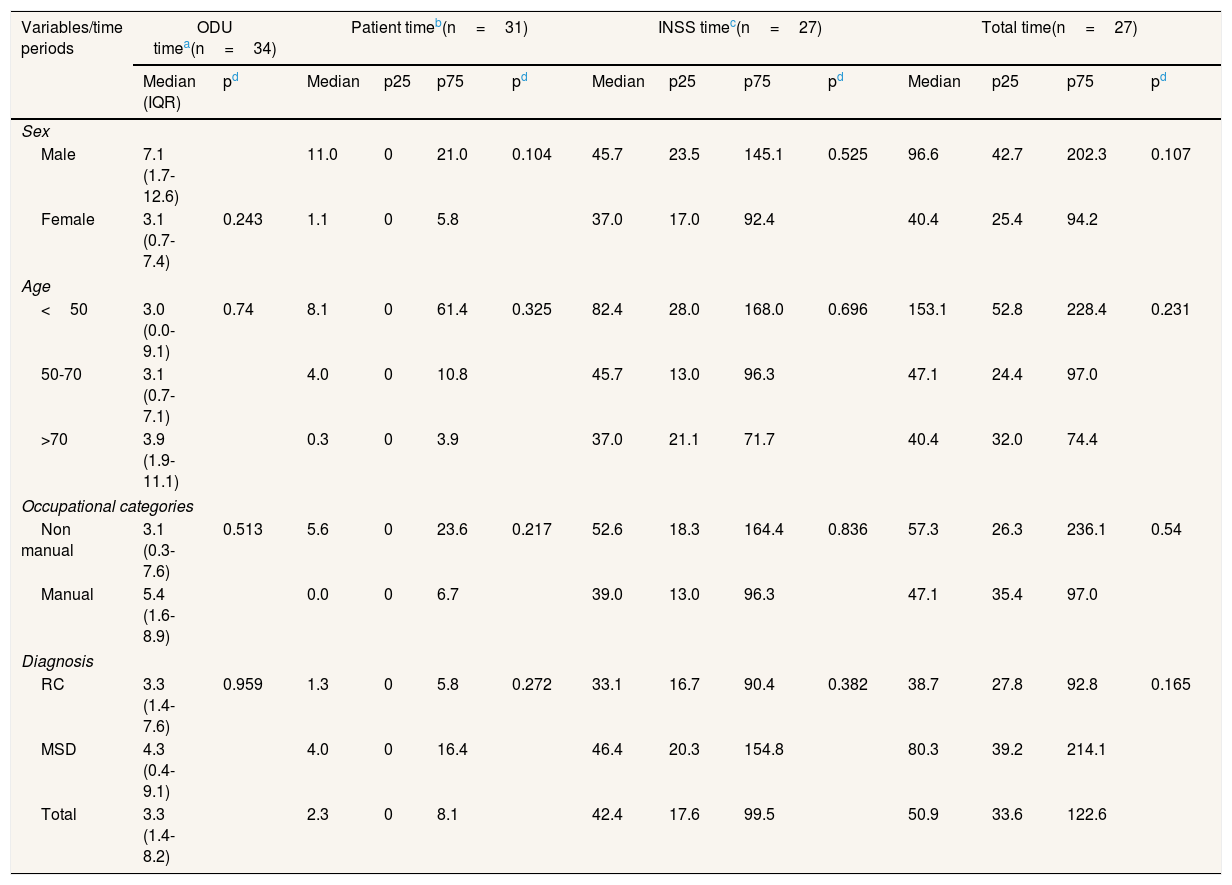
Each period was quantified by weeks using the median, and percentiles 25 and 75 (interquartile range [IQR]) according to sex, age (less than 50, 50 to 70, and more than 70 years), and occupational category (non-manual and manual). Median differences were tested by the Mann-Whitney U and Kruskal-Wallis tests with R software.
The clinical research ethics committee from Hospital del Mar approved this project on 20th January 2017, number 2016/6822/I, and data are available on request.
ResultsOut of 18 identified respiratory cancer cases of possible OD, 16 (89%) were reported to the INSS, of those 15 (94%) finished the recognition INSS process, and 12 (86%) were finally recognized by the INSS. Among the 16 identified MSD cases, 15 (94%) started the recognition process, 12 (80%) finalized it, and only 2 (17%) were recognized. Seventeen (94%) respiratory cases were men, most (67%) were 70 years or older, and 67% were manual workers. Ten MSD cases (63%) were women, 56% were 50 to 70 years of age and 69% were manual workers.
The median total time for the 27 cases who had final resolution by INSS was 51 weeks (IQR 34-123 weeks). The ODU time was 3 weeks (1-8), the patients time 2 weeks (0-8) and the INSS time was 42 weeks (18-100). There were no statistically significant differences for sex, age or occupational category for any of the analysed periods (p>0.10) (Table 1).
Process for the recognition of suspected occupational diseases: time periods (weeks) for patients (n=34) from referral by a hospital clinician to the Occupational Disease Unit (ODU) to its final resolution of recognition by the INSS (Spanish National Institute of Social Security). Occupational Health Service, Hospital del Mar (Barcelona, Spain), 2010-2019.
| Variables/time periods | ODU timea(n=34) | Patient timeb(n=31) | INSS timec(n=27) | Total time(n=27) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | pd | Median | p25 | p75 | pd | Median | p25 | p75 | pd | Median | p25 | p75 | pd | |
| Sex | ||||||||||||||
| Male | 7.1 (1.7-12.6) | 11.0 | 0 | 21.0 | 0.104 | 45.7 | 23.5 | 145.1 | 0.525 | 96.6 | 42.7 | 202.3 | 0.107 | |
| Female | 3.1 (0.7-7.4) | 0.243 | 1.1 | 0 | 5.8 | 37.0 | 17.0 | 92.4 | 40.4 | 25.4 | 94.2 | |||
| Age | ||||||||||||||
| <50 | 3.0 (0.0-9.1) | 0.74 | 8.1 | 0 | 61.4 | 0.325 | 82.4 | 28.0 | 168.0 | 0.696 | 153.1 | 52.8 | 228.4 | 0.231 |
| 50-70 | 3.1 (0.7-7.1) | 4.0 | 0 | 10.8 | 45.7 | 13.0 | 96.3 | 47.1 | 24.4 | 97.0 | ||||
| >70 | 3.9 (1.9-11.1) | 0.3 | 0 | 3.9 | 37.0 | 21.1 | 71.7 | 40.4 | 32.0 | 74.4 | ||||
| Occupational categories | ||||||||||||||
| Non manual | 3.1 (0.3-7.6) | 0.513 | 5.6 | 0 | 23.6 | 0.217 | 52.6 | 18.3 | 164.4 | 0.836 | 57.3 | 26.3 | 236.1 | 0.54 |
| Manual | 5.4 (1.6-8.9) | 0.0 | 0 | 6.7 | 39.0 | 13.0 | 96.3 | 47.1 | 35.4 | 97.0 | ||||
| Diagnosis | ||||||||||||||
| RC | 3.3 (1.4-7.6) | 0.959 | 1.3 | 0 | 5.8 | 0.272 | 33.1 | 16.7 | 90.4 | 0.382 | 38.7 | 27.8 | 92.8 | 0.165 |
| MSD | 4.3 (0.4-9.1) | 4.0 | 0 | 16.4 | 46.4 | 20.3 | 154.8 | 80.3 | 39.2 | 214.1 | ||||
| Total | 3.3 (1.4-8.2) | 2.3 | 0 | 8.1 | 42.4 | 17.6 | 99.5 | 50.9 | 33.6 | 122.6 | ||||
IQR: interquartile range (p25-p75); MSD: musculoskeletal disorder; RC: respiratory cancer.
For respiratory cancer cases, the median total time was 39 weeks (28-93), and for MSD cases 80 weeks (39-214). For both groups, the largest subperiod was the INSS time (respiratory cancer: 33 weeks; MSD: 46 weeks) and the shortest was the ODU time (respiratory cancer: 3 weeks; MSD: 4 weeks). These differences were not statistically significant.
DiscussionAccording to our study, patients must wait almost a whole year to get official recognition, or not, since a first suspicion is made by a hospital physician hospital in Spain. This time seems to be determined both by the institution involved in the process, and the type of disease, although differences were not statistically significant.
The INSS is the administrative institution where the process took much longer, both for respiratory cancer and MSD cases. INSS requests a compulsory declaration during the four following working days from the Mutua, and ten days from the patient5. However, from then onwards, there is no deadline for the INSS to resolve while a medical tribunal investigates and makes a report to guide the final resolution.
Differences in disease severity and multicausality could also explain the differences observed in our study between diagnostic groups. Logically, it may be easier to establish a specific risk factor association between, for instance, a mesothelioma case and asbestos exposure6 than for epicondylitis case and repetitive movement.7 Differences do not seem to be influenced by sex, age or occupation category, suggesting that the social protection system does not initially contribute to health inequalities.8
We cannot compare our results with previous studies, as to the best of our knowledge there are no published studies in Spain or elsewhere measuring the length of time it takes patients to obtain OD recognition from identification.9 However, this information is relevant because the length of the process and other barriers surely discourage patients to start the process for their OD recognition.10 There is a need to better understand the process and try to facilitate it. Qualitative methods could contribute to identify specific characteristics of the process for improvement.
In our study, detailed data were recorded along the recognition process for a small series of cases of suspected OD. Larger series of patients are needed to complement and confirm our results in Spain and other countries with similar OD social protection systems.
In conclusion, the process until official recognition of ODU in our series appears to be much longer than it should reasonably be, and it could be one reason for underreporting OD in Spain and other countries with similar recognition processes. Some recommendations can be raised such as the improvement of the administrative process to reduce patients’ waiting time for the recognition of their occupational disease and encourage patients and stakeholders to start the process. A better approach of the procedure, such as establishing deadlines to solve claims, with maintained feed-back information to patients would also contribute.
Editor in chargeCarlos Álvarez-Dardet.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Recognition of occupational disease has important implications for the worker, for the prevention of occupational risks and for the public health system. The under-recognition of occupational diseases is largely known and widespread. The duration of the process for recognition of occupational diseases is unknown.
What does this study add to the literature?The process since an occupational disease is suspected by a physician until its official recognition is very long. The longest subperiod time appears to be while waiting the final resolution from the Social Security system.
What are the implications of the results?The administrative process must be improved to reduce patients’ waiting time for the recognition of their occupational disease and encourage patients and stakeholders to start the process.
F.G. Benavides and A. Pelegrí conceived the study, carried out the analyses and drafted the first version of the manuscript. J.M. Ramada and C. Palma-Vásquez participated in the data collection and the revision of the manuscript. C. Serra participated in the design of the study, and revised the manuscript. All authors have read and approved the final version.
FundingThis work was partly supported by Instituto de Salud Carlos III through the Fondo de Investigación Sanitaria FIS/FEDER FIS P016/00061, and an agreement between Parc de Salut Mar and the University Pompeu Fabra (Barcelona, Spain).
Conflicts of interestsThe authors declare they have no conflicts of interest. The funders do not have any involvement in the study design, in the collection, analysis, and interpretation of the data, nor in the writing of the report, and the decision to submit the paper for publication.
We would like to thank the entire research team for project planning, data collection, handling, and management. Special thanks to Olga Martinez and Anna Amat for the continuous follow-up of the patients, and all physicians of Hospital del Mar who referred their patients to the Occupational Disease Unit, and to all participant patients and their families.