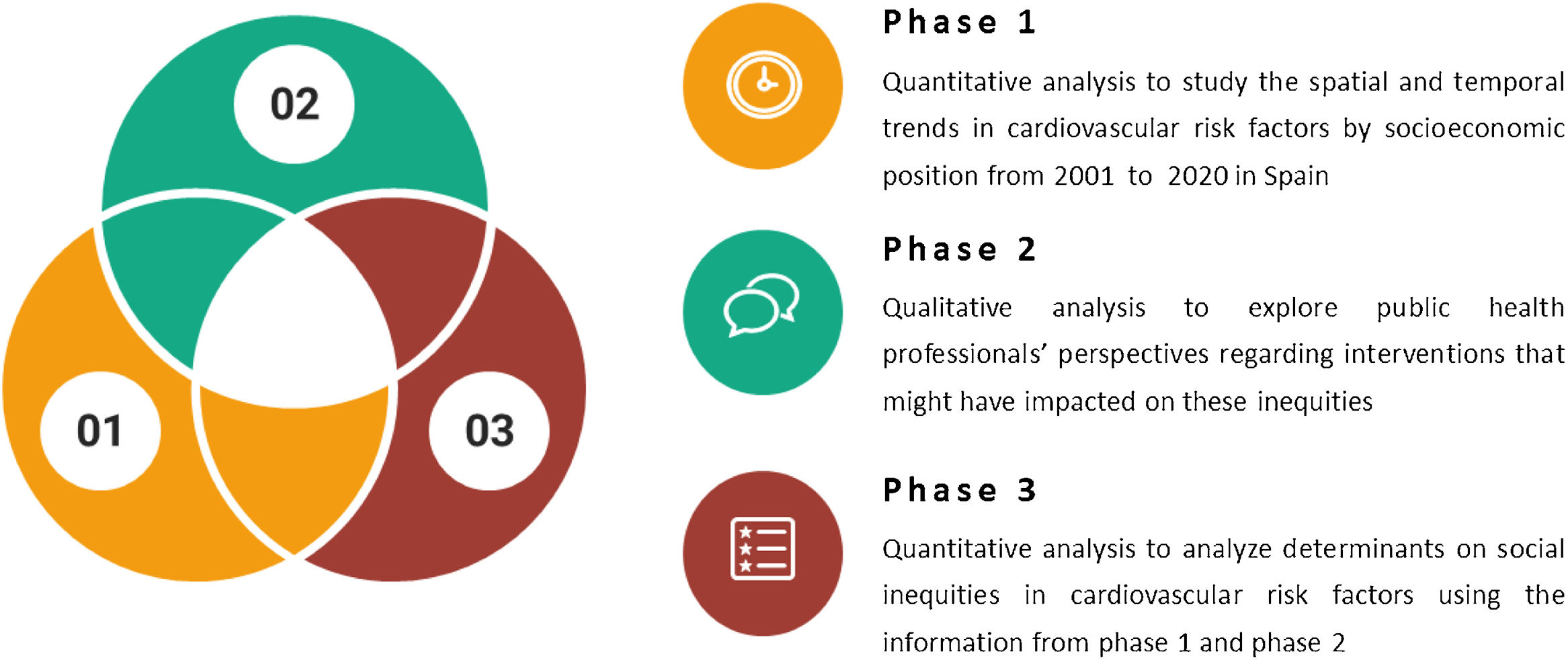
This sequential mixed-methods study aims to: 1) assess spatial and temporal trends in cardiovascular risk factors by socioeconomic position from 2001 to 2020 in Spain; 2) explore public health professionals’ perspectives regarding interventions that might have impacted these inequities; and 3) analyze determinants on social inequities in cardiovascular risk factors. First, we will measure the change in absolute and relative social inequities in eight cardiovascular risk factors through time trend analysis using repeated cross-sectional data from both National and European Health Surveys for Spain from 2001 to 2020. Second, we will interview key informants —both at the regional and national level—, to contextualize data obtained in phase 1 and capture the content and variation of policies across regions. Third, we will use econometric methods to analyze how these identified interventions have impacted these social inequities within and across regions.
Este estudio tiene por objetivos: 1) evaluar las tendencias espacio-temporales de los factores de riesgo cardiovascular en España, por posición socioeconómica, entre 2001 y 2020; 2) explorar las perspectivas de profesionales salubristas con respecto a las intervenciones que pueden influir en estas inequidades; 3) analizar los determinantes de las inequidades sociales en los factores de riesgo cardiovascular. Primero se medirá el cambio en las desigualdades, en términos absolutos y relativos, según ocho factores de riesgo mediante un análisis de tendencias temporales y datos de las encuestas nacionales y europeas de salud para España entre 2001 y 2020. Después se entrevistará a informantes clave, en los ámbitos de comunidad autónoma y nacional, para contextualizar los datos obtenidos en la primera fase y explorar la variabilidad entre comunidades autónomas. Por último, se analizará mediante métodos econométricos cómo influyen dichas intervenciones en las desigualdades sociales entre comunidades autónomas.
Cardiovascular diseases (CVD) are a major contributor to both morbidity and mortality imposing a huge economic burden on healthcare systems.1 Yet, previous studies have suggested that CVD mortality can be reduced up to 75% by improving major risk factors (e.g., blood pressure and cholesterol levels) at the population level.2 Reducing risk factors can be achieved through individual high-risk or population-level approaches.3 The latter aim to shift the entire distribution of risk factors and offer a greater potential for population-level impacts.3–5
CVD prevalence and mortality are inequitably distributed across socioeconomic groups.6,7 A recent analysis in Spain reported that most socially disadvantaged individuals present a higher prevalence of hypercholesterolemia, diabetes, hypertension, obesity, and smoking —which is independent of age.8 Yet, most evidence comes from cross-sectional studies so that time trends in inequities in the prevalence of CVD risk factors disaggregated by indicators that capture different socioeconomic circumstances in the Spanish population are lacking.9,10
Moreover, previous research in Spain has primarily focused on social inequities in CVD mortality.11 Thus, longitudinal studies monitoring the magnitude, direction, and change in risk factors by social groups in the adult population are needed. This data could help ensure that public health interventions for CVD prevention and control are tailored to reach vulnerable population groups at high risk of CVD and to properly address their specific needs and challenges. They also allow for the characterization of population-level drivers of these inequities.12,13
Using a mixed-methods approach, we will assess the trends in the prevalence of CVD risk factors by socioeconomic position from 2001 to 2020 in Spain and to monitor changes in absolute and relative inequities stratified by age and sex. Furthermore, we will explore public health professionals’ perspectives regarding which interventions (e.g., policies or changes in contextual variables) might have impacted these inequities. Third, we will use econometric methods to analyze how these identified interventions have impacted these social inequities within and across regions in Spain.
MethodStudy designThis study will use a sequential mixed-methods study and will be conducted in Spain from 2022 to 2024 (Figure 1).
Phase 11) Participants
In the first phase, we will include adults from the latest cycles (2001-2020) of the Spanish National Health Survey (ENSE) and the Spanish Module of the European Health Survey (EESE). These are nationally representative cross-sectional surveys of the Spanish non-institutional population, comparable with each other, and which design and methodology have been described in detail.14
2) Measures
- •
Cardiovascular risk factors: we will focus on the main cardiovascular risk factors: hypertension, diabetes, obesity, hypercholesterolemia, diet, physical inactivity, and alcohol and tobacco consumption (see online Appendix). In both surveys, data on these variables is self-reported.
- •
Socioeconomic and demographic variables: To measure socioeconomic status (SES), we will use occupational social class classified using the Spanish version of the International Standard Classification of Occupations. Social class categories will be ranked in ascending order of deprivation (I: higher grade professionals, administrators, and officials, managers in large industrial establishments; VI: unskilled workers).15 We will also use educational level as alternative proxies in sensitivity analyses.8. Demographic factors will include: 1) sex (defined as man/woman), 2) age; 3) country of origin, and 4) region of residence categorized into one of the 17 administrative regions of the country, equivalent to NUTS-2. All these variables will be also self-reported.
3) Statistical analysis
We will conduct stratified analyses by sex. To estimate the change in absolute socioeconomic inequities we will examine the slope index of inequality (SII) and relative socioeconomic inequities with the relative index of inequality (RII).16 To do so, we will perform additive and multiplicative Poisson models respectively. All models will have a multilevel structure, with individuals nested in each region and then in each survey and including a random slope at both levels to estimate SII and RII by region and survey. As sensitivity analysis to increase statistical power, we will analyze the results joining surveys (2001-2003; 2006-2009; 2011-2014; 2017-2020). All analyses will be conducted using R version 4.3.1 (R Project for Statistical Computing).
Phase 21) Participants
In this second phase, we will use a qualitative approach to 1) capture the content and variation of policies across regions, and 2) contextualize the data obtained in phase 1. Therefore, we will conduct semi-structured interviews with key informants —both at the regional and national level— who will help explain the dynamics related to all cardiovascular risk factors in every region. Specifically, we will aim to interview 1-3 key informants per region, who will selected using purposeful sampling and considering predetermined characteristics (e.g., sex, age, or professional experience).
2) Measures
We will meet at least three times with each key informant. First, we will present a general overview of the project and reflect on the prevalence of CVD risk factors in the region. Then, the key informant will identify specific interventions —both directly and indirectly health-related— that could have influenced the trends of the existing inequities in the region. Lastly, we will present and discuss the specific data for the region obtained in the phase 1.
3) Analysis
We will conduct a descriptive thematic qualitative analysis17,18 to 1) describe the knowledge and narratives regarding social inequities in CVD risk factors at the regional level; 2) describe the factors that might have influenced these inequities in terms of scope (national/regional/local), target population, or implementation level; and 3) explore how key informants contextualize the temporal trends of these social inequities related to each CVD risk factor in each region. Our analyses will undergo member checking with the participants and will be complemented with contextual variables from the atlas by Daponte-Codina et al.19
Phase 3This third phase will incorporate both quantitative and qualitative results to explore whether the identified interventions from phase 2 can explain changes in the spatial and temporal trends identified in phase 1 in each region.
1) Participants
Same participants as in sub-study 1.
2) Variables
We will use the same variables as in phase 1, to which we will add the interventions identified in phase 2. We will operationalize these into variables that can be fitted in quantitative analysis.
3) Analysis
We will use quasi-experimental models to analyze the impact of interventions on social inequities in CVD risk factors for each region. Specifically, we will use difference-in-differences and comparative interrupted time series techniques. This will allow exploring trends in inequities as described in phase 1, before and after their implementation, and comparing regions that have implemented them with those that did not. For national-level interventions, we will explore before- and after-implementation trends (uncontrolled interrupted time series).
Ethical considerationsThe study will be conducted according to the guidelines laid down by the Declaration of Helsinki and ethical approval was granted by the Ethics Committee of the Universidad de Alcalá (CEIP/2022/4/074). Participants will be assured of anonymity and confidentiality. We will obtain written consent for their participation and return results for their validation. All data exchanges will adhere to the most up-to-date EU and national data protection regulations.
DiscussionTo the best of our knowledge, few research projects on this topic have been conducted or are in progress in Spain. Specifically, this study will provide relevant evidence about the spatial and temporal trends of social inequities with CVD risk factors in Spain. This evidence will be particularly useful for decision-makers to inform future resource allocation and to implement preventive measures that not only target the entire population but also focus on socially disadvantaged groups.
Identifying variations across territories and socioeconomic groups is a key step in examining the barriers to reducing major CVD risk factors in Spain. Thus, this study will provide evidence regarding which interventions can improve this situation.
The mixed methods approach will allow deepening the interpretation of quantitative data with the knowledge of the context that is not available to researchers. It represents a methodological advantage because it will allow quantitatively exploring factors in phase 3 that would otherwise be difficult to identify. In addition, it also represents a paradigmatic change in the epistemological approach of similar investigations, since it suggests that quantitative data benefit from the interpretation of key informants who understand the context in which they are produced.
LimitationsThis study has limitations. First, data will be based on self-reports which may lead to potential biases and measurement errors. This will be especially problematic if the measurement error is differential by socioeconomic position; however, previous studies with some of the variables (e.g., diabetes) indicate that the risk of differential measurement bias is low.20 Although the identification of interventions may be subject to the social reality of key informants, we will try to minimize this potential bias through several sessions with the informants. Also, our repeated cross-sectional design will not allow us to examine how policies can individually modify CVD risk factors, since the surveys do not use the same population as a cohort.
ConclusionsThis mixed-methods study will evaluate the trends change in CVD risk factors by socioeconomic position among adults in Spain between 2001 and 2020, and quantify the magnitude, direction, and change in absolute and relative inequities stratified by sex. Thus, it will provide relevant evidence to influence future interventions promoting people's cardiovascular health while addressing social inequities.
Editor in chargeJorge Marcos Marcos.
Authorship contributionsJ. Díez: conceptualization, writing original draft, methodology, funding acquisition. G. Taulet: writing, review and editing, resources. M. Fontán-Vela: writing, review and editing, methodology. Y. González-Rábago: writing, review and editing, resources. L. Cereijo: writing, review and editing. M. Sandín-Vázquez: writing, review and editing. E. Rodríguez: writing, review and editing. M. Franco: writing, review and editing. C. Borrell: writing, review and editing, supervision, methodology. U. Bilal: writing, review and editing, methodology. P. Gullón: conceptualization, writing, review and editing, methodology, project administration, funding acquisition.
AcknowledgmentsWe would like to thank all the workers at the National Institute of Statistics for their public service collecting and providing data for health researchers.
FundingThis study has been funded by Instituto de Salud Carlos III (ISCIII) through the project “PI21/01868” and co-funded by the European Union. The funder had no role in study design, data collection and analysis, decision to publish, nor preparation of the manuscript. L. Cereijo was supported by a predoctoral fellowship (PFIS) from the Institute of Health Carlos III (Exp. FI19/00343).
Conflicts of interestsNone.