The effect of drugs other than alcohol on severity of trauma remains unclear. Pooled data analyses in previous studies that grouped substances with opposite effects on the central nervous system (CNS) may have masked the influence of substances on injury severity. The aim was to analyze the effect of stimulant, hallucinogenic and depressant drugs other than alcohol on injury severity in trauma patients.
MethodsThe presence of alcohol, stimulant drugs (cocaine, amphetamines and methamphetamines), depressant drugs (benzodiazepines, opiates, methadone and barbiturates) and hallucinogenic drugs (THC and PCP) was analyzed in 1187 patients between 16 and 70 years old admitted to a trauma hospital between November 2012 and June 2015. Injury severity was determined prospectively as the Injury Severity Score. A multivariate analysis was used to quantify the strength of association between exposure to substances and trauma severity, using the presence of alcohol as a stratification variable.
ResultsDrugs other than alcohol were found in 371 patients (31.3%): 32 (2.7%) stimulants, 186 (15.3%) depressants, 78 (6.6%) hallucinogenics and 75 (5.6%) polydrug use. The presence of CNS depressant substances was associated with increased injury severity only in patients also exposed to alcohol, with an adjusted odds ratio of 4.63 (1.37-15.60) for moderate injuries and 7.83 (2.53-24.21) for severe.
ConclusionCNS depressant drugs had a strong influence on injury severity in patients who screened positive for alcohol consumption.
No está claro qué efecto tienen las drogas distintas del alcohol sobre la gravedad de los traumatismos. Los análisis incluidos en estudios previos, que agrupan sustancias con efectos opuestos sobre el sistema nervioso central (SNC), pueden haber enmascarado la influencia de estas sobre la gravedad. El objetivo fue analizar el efecto de las drogas alucinógenas, estimulantes y depresoras del SNC, diferentes del alcohol, sobre la gravedad de las lesiones en pacientes ingresados por traumatismos.
MétodosSe analizó la presencia de alcohol, drogas estimulantes (cocaína, anfetaminas y metanfetaminas), depresoras (benzodiacepinas, opiáceos, metadona y barbitúricos) y alucinógenas (THC y PCP) en 1187 pacientes de entre 16 y 70 años de edad ingresados por traumatismo de noviembre de 2012 a junio de 2015. La gravedad del traumatismo se determinó prospectivamente mediante la Injury Severity Score. Se cuantificó la fuerza de la asociación entre la exposición a sustancias y la gravedad del traumatismo mediante un análisis multivariante, utilizando la presencia de alcohol como variable de estratificación.
ResultadosSe encontraron drogas diferentes del alcohol en 371 pacientes (31,3%): 186 (15,3%) depresoras, 78 (6,6%) alucinógenas, 32 (2,7%) estimulantes y 75 (5,6%) combinadas. La presencia de sustancias depresoras del SNC se asoció con un aumento de la gravedad del traumatismo solo en pacientes también expuestos al alcohol, con una odds ratio ajustada de 4,63 (1,37-15,6) para lesiones moderadas y de 7,83 (2,53-24,21) para lesiones graves.
ConclusiónLas drogas depresoras del SNC tuvieron una fuerte influencia en la gravedad del traumatismo en los pacientes que además presentaban resultados positivos para consumo de alcohol.
The role of alcohol as a major causal factor in trauma has been highlighted in several studies.1–5 In recent years concern has spread to drugs other than alcohol,6–13, including prescribed or nonprescribed psychotropic drugs.14,15 Studies to date conclude that exposure to alcohol and drugs are associated with a higher risk of injury regardless of the mechanism of injury (traffic crashes, falls, etc.).
Although there appears to be agreement that alcohol and other drugs are important risk factors for injury, there is no consensus on the role of these substances in severity. Some studies found that the presence of these substances increases trauma severity,16–24 whereas others found no such association.14,25–27 However, studies that evaluated the effect of illicit or psychotropic drugs on trauma rarely focused on the use of these substances separately,14,24,27 because the main focus of study was usually alcohol consumption. This leads to important methodological deficiencies in assessing the association between substances other than alcohol and injury severity. For example, drugs with different effects, including opposite effects, on the central nervous system (CNS) are usually pooled for statistical analysis.21–23,26 Moreover, some studies systematically excluded patients with positive tests for benzodiazepines and opiates,21,24,26 because these drugs are frequently used in prehospital care for trauma patients. This makes it impossible to analyze the role of these substances in trauma severity. To these limitations must be added the fact that these studies were frequently based on data obtained from national, regional or hospital-based trauma registries.16,19,21,22,27 These registries record only patients whose medical care provider decided to request an alcohol and/or drug test at the time the patient was admitted to the emergency room.
The factors related to injury severity merit more in-depth analysis. Greater injury severity is strongly associated with increased mortality, more complications, longer hospital stays, and ultimately greater economic costs.28 We believe it is worthwhile to investigate the specific roles of drugs in trauma severity, based on the hypothesis that a separate analysis of the effect of each substance on the CNS (depressants, stimulants and hallucinogens) will indicate a greater magnitude of association for the group of depressant substances, due to the reduced awareness and impaired cognitive and motor function that these agents cause.29 The aims of the present study were thus to analyze the effect of stimulant, hallucinogenic and depressant drugs other than alcohol on injury severity in hospital patients admitted for trauma, and to determine the possible role of alcohol as a modifier of the effect of these drugs.
MethodsEnvironmentThe data for this study were from a cohort of patients admitted for traumatic injuries. This cohort was created as part of a Screening, Brief Intervention, and Referral to Treatment (SBIRT) project30 designed for trauma patients (MOTIVA project). The MOTIVA project was approved by the Granada Provincial Research Ethics Committee and was active during the 31 nonconsecutive months during which it received financial support from the Regional Andalusian Government and the Spanish National Traffic Directorate: November 2011 to October 2012, June 2013 to November 2013, and June 2014 to June 2015 at the University Hospital Virgen de las Nieves of Granada, Spain. Our Hospital is a public tertiary-care hospital with a separate trauma center that covers a population of more than 600,000 inhabitants.
Definition of exposureThe MOTIVA project involved screening for alcohol and drug use in all patients aged 16 to 70 years who were hospitalized for trauma independently of trauma severity. Informed consent was required before the screening. In sedated patients or unable to collaborate, informed consent was required when the clinical situation was reversed or, if it was not possible, to relatives.
Screening for drugs (tetrahydrocannabinol [THC], phencyclidine [PCP], cocaine, amphetamines, methamphetamines, benzodiazepines, opiates, methadone, barbiturates or tricyclic antidepressants) was done with urine testing by fluorescence immunoassay.31,32 Review of the patient's medical record was used to rule out patients who tested positive for benzodiazepines and opioids as a result of emergency treatment of their injuries. Alcohol consumption was screened by blood testing, and was considered positive when the blood alcohol level was higher than 0.3g/L (the same cutoff point established by the Spanish National Institute of Toxicology and Forensic Sciences)33 at the time of hospitalization or, given the short window of detection (6hours),34 if the patient reported exposure on interview. Therefore, personal interviews were conducted to confirm the status of alcohol exposure in patients screened 6hours after the trauma. The interviews were carried out at the moment in which the patients’ clinical conditions permitted it. The remaining study variables were collected from the medical records prospectively.
Definition of outcomeThe MOTIVA project contemplated the injury codification based on the Abbreviated Injury Scale (AIS)35 of all patients hospitalized with injury diagnosis (ICD9-CM). This anatomical-based coding system classifies injuries in each of nine body regions using an ordinal scale of 1-6, with 1 as least severe and 6 as most severe. For the present study, trauma severity was measured with the Injury Severity Score (ISS).36 The ISS is determined by summing the squares of the highest AIS rating (up to 5) for each of the three most severely injured body areas. If any of the three scores is a 6, the score is automatically set at 75. Consequently, ISS can take values between 1 and 75. Scores were recorded during the patient's hospital stay.
Analytic approachThe cases selected for this study were all screened patients from the MOTIVA project. For the data analysis, the variable for the presence of drugs other than alcohol was categorized into five strata: none, presence of CNS stimulant drugs (cocaine, amphetamines and methamphetamines), presence of CNS depressant drugs (benzodiazepines, opiates, methadone and barbiturates), hallucinogenic drugs (THC and PCP), and polydrug (any combination of substances in the above groups). The ISS was categorized into three strata: mild (1 to 8), moderate (9 to 15) and severe (≥16).
Continuous variables (age and days of hospital stay) are presented as medians with interquartile ranges. Between-group comparisons of these variables were carried out with the Kruskal-Wallis test. The chi-squared test was used to identify associations between categorical variables (sex, mechanism of injury and hospital mortality).
To quantify the strength of association between substance consumption and trauma severity, we used multinomial logistic regression in two models. In all analyses, trauma severity was the dependent variable and “mild” was used as the reference category. In model 1 the presence of substances was categorized into the five previously defined levels. The initial analysis was done with the entire sample, and in a second step, the sample was stratified according to the presence or absence of alcohol. In model 2 the same statistical analyses were repeated but the presence of substances was categorized dichotomously as presence or absence.
For both models, we calculated crude odds ratios (cOR), and adjusted odds ratio (aOR) estimates were obtained by adding age, sex, and mechanism of injury as independent variables. For all estimates, we calculated the corresponding 95% confidence intervals (95%CI). All analyses were done with the SPSS v. 20.0 for Windows (SPSS, Chicago, IL, USA).
ResultsOf all 1818 patients aged 16 to 70 years who were hospitalized for trauma during the study periods, 1187 (65.3%) could be screened for alcohol and drug use; 609 patients were not screened and 22 rejected it. Of all patients screened, 371 (31.3%) were positive for drugs other than alcohol: 32 (2.7%) for CNS stimulant drugs, 186 (15.7%) for CNS depressants, 78 (6.6%) for hallucinogenics and 75 (5.6%) for polydrug. Alcohol was the substance detected most frequently (295 patients; 24.9%), followed by THC (144; 12.2%), benzodiazepines (199; 16.8%), cocaine (81; 6.8%), opiates (26; 2.2%), methadone (25; 2.1%); barbiturates (7; 0.6%), amphetamines (9; 0.8%) and PCP (2; 0.2%).
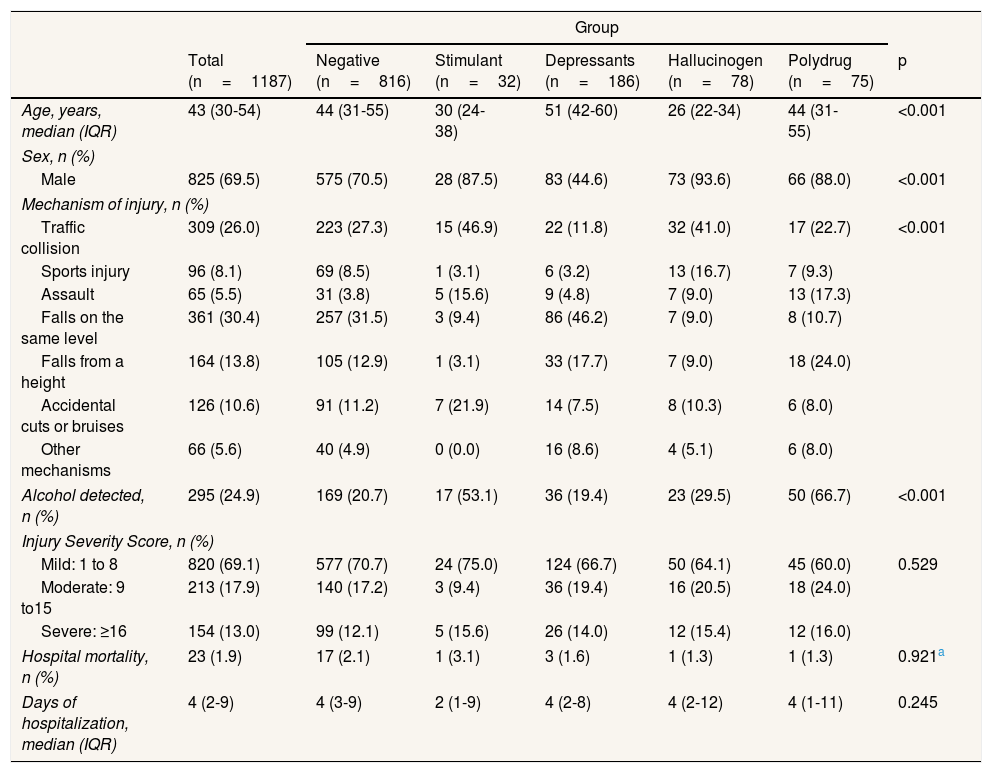
When we compared the demographic and clinical characteristics of the five groups according to type of drug consumed (Table 1), we found that age was oldest for consumers of depressant substances, with a median age (interquartile range) of 51 years (42-60), and much younger in patients who tested positive for hallucinogenics (median: 26 years [22-34]). The proportion of women was greater in the subgroup of individuals who tested positive for depressant drugs (44.6%) than in the other four groups. A fall on the same level was the most frequent mechanism of injury in this group (46.2%), in contrast to the stimulant drugs group, in which the most frequent mechanism was traffic crashes (43.5%). In the subgroup of polydrug, alcohol consumption was especially frequent (66.7%). There were no relevant differences between groups in the duration of hospital stay (in days) or mortality.
Demographic and clinical comparisons according to substance(s) detected.
| Group | |||||||
|---|---|---|---|---|---|---|---|
| Total (n=1187) | Negative (n=816) | Stimulant (n=32) | Depressants (n=186) | Hallucinogen (n=78) | Polydrug (n=75) | p | |
| Age, years, median (IQR) | 43 (30-54) | 44 (31-55) | 30 (24-38) | 51 (42-60) | 26 (22-34) | 44 (31-55) | <0.001 |
| Sex, n (%) | |||||||
| Male | 825 (69.5) | 575 (70.5) | 28 (87.5) | 83 (44.6) | 73 (93.6) | 66 (88.0) | <0.001 |
| Mechanism of injury, n (%) | |||||||
| Traffic collision | 309 (26.0) | 223 (27.3) | 15 (46.9) | 22 (11.8) | 32 (41.0) | 17 (22.7) | <0.001 |
| Sports injury | 96 (8.1) | 69 (8.5) | 1 (3.1) | 6 (3.2) | 13 (16.7) | 7 (9.3) | |
| Assault | 65 (5.5) | 31 (3.8) | 5 (15.6) | 9 (4.8) | 7 (9.0) | 13 (17.3) | |
| Falls on the same level | 361 (30.4) | 257 (31.5) | 3 (9.4) | 86 (46.2) | 7 (9.0) | 8 (10.7) | |
| Falls from a height | 164 (13.8) | 105 (12.9) | 1 (3.1) | 33 (17.7) | 7 (9.0) | 18 (24.0) | |
| Accidental cuts or bruises | 126 (10.6) | 91 (11.2) | 7 (21.9) | 14 (7.5) | 8 (10.3) | 6 (8.0) | |
| Other mechanisms | 66 (5.6) | 40 (4.9) | 0 (0.0) | 16 (8.6) | 4 (5.1) | 6 (8.0) | |
| Alcohol detected, n (%) | 295 (24.9) | 169 (20.7) | 17 (53.1) | 36 (19.4) | 23 (29.5) | 50 (66.7) | <0.001 |
| Injury Severity Score, n (%) | |||||||
| Mild: 1 to 8 | 820 (69.1) | 577 (70.7) | 24 (75.0) | 124 (66.7) | 50 (64.1) | 45 (60.0) | 0.529 |
| Moderate: 9 to15 | 213 (17.9) | 140 (17.2) | 3 (9.4) | 36 (19.4) | 16 (20.5) | 18 (24.0) | |
| Severe: ≥16 | 154 (13.0) | 99 (12.1) | 5 (15.6) | 26 (14.0) | 12 (15.4) | 12 (16.0) | |
| Hospital mortality, n (%) | 23 (1.9) | 17 (2.1) | 1 (3.1) | 3 (1.6) | 1 (1.3) | 1 (1.3) | 0.921a |
| Days of hospitalization, median (IQR) | 4 (2-9) | 4 (3-9) | 2 (1-9) | 4 (2-8) | 4 (2-12) | 4 (1-11) | 0.245 |
IQR: interquartile range.
Chi-squared exact test.
Negatives: negative for drugs other than alcohol; Stimulant: positive for cocaine, amphetamines and/or methamphetamines; Depressants: positive for benzodiazepines, opiates, methadone and/or barbiturates; Hallucinogen: positive for THC and/or PCP; Polydrug: positive for any combination of substances in the above groups.
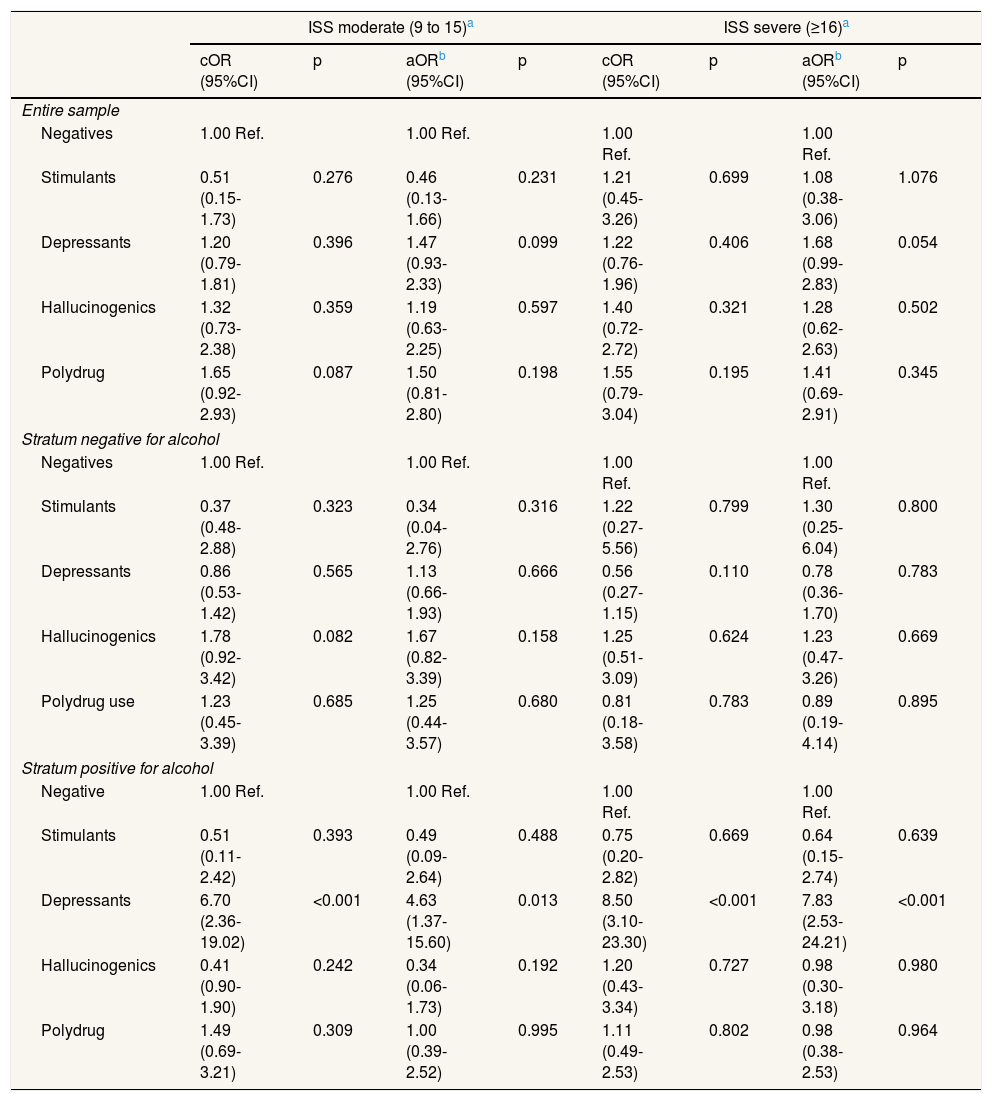
In the multivariate analysis (Table 2), the estimates of strength of association between each drug group and the frequency of moderate and severe injuries in model 1 showed that alcohol modified the association between depressant drugs and injury severity. This association was nonexistent in the group who had not been exposed to alcohol, whereas alcohol consumption was associated with an increase in injury severity in the group of patients exposed to CNS depressants, with an adjusted aOR of 4.63 (95%CI: 1.37-15.60) for moderate injuries and 7.83 (95%CI: 2.53-24.21) for severe injuries. This modifying effect did not appear in the other groups.
Multivariate analysis of drugs detected and injury severity in the entire sample and by stratums positive or negative for alcohol. Model 1: substances other than alcohol grouped according to their effect on the central nervous system.
| ISS moderate (9 to 15)a | ISS severe (≥16)a | |||||||
|---|---|---|---|---|---|---|---|---|
| cOR (95%CI) | p | aORb (95%CI) | p | cOR (95%CI) | p | aORb (95%CI) | p | |
| Entire sample | ||||||||
| Negatives | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | ||||
| Stimulants | 0.51 (0.15-1.73) | 0.276 | 0.46 (0.13-1.66) | 0.231 | 1.21 (0.45-3.26) | 0.699 | 1.08 (0.38-3.06) | 1.076 |
| Depressants | 1.20 (0.79-1.81) | 0.396 | 1.47 (0.93-2.33) | 0.099 | 1.22 (0.76-1.96) | 0.406 | 1.68 (0.99-2.83) | 0.054 |
| Hallucinogenics | 1.32 (0.73-2.38) | 0.359 | 1.19 (0.63-2.25) | 0.597 | 1.40 (0.72-2.72) | 0.321 | 1.28 (0.62-2.63) | 0.502 |
| Polydrug | 1.65 (0.92-2.93) | 0.087 | 1.50 (0.81-2.80) | 0.198 | 1.55 (0.79-3.04) | 0.195 | 1.41 (0.69-2.91) | 0.345 |
| Stratum negative for alcohol | ||||||||
| Negatives | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | ||||
| Stimulants | 0.37 (0.48-2.88) | 0.323 | 0.34 (0.04-2.76) | 0.316 | 1.22 (0.27-5.56) | 0.799 | 1.30 (0.25-6.04) | 0.800 |
| Depressants | 0.86 (0.53-1.42) | 0.565 | 1.13 (0.66-1.93) | 0.666 | 0.56 (0.27-1.15) | 0.110 | 0.78 (0.36-1.70) | 0.783 |
| Hallucinogenics | 1.78 (0.92-3.42) | 0.082 | 1.67 (0.82-3.39) | 0.158 | 1.25 (0.51-3.09) | 0.624 | 1.23 (0.47-3.26) | 0.669 |
| Polydrug use | 1.23 (0.45-3.39) | 0.685 | 1.25 (0.44-3.57) | 0.680 | 0.81 (0.18-3.58) | 0.783 | 0.89 (0.19-4.14) | 0.895 |
| Stratum positive for alcohol | ||||||||
| Negative | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | ||||
| Stimulants | 0.51 (0.11-2.42) | 0.393 | 0.49 (0.09-2.64) | 0.488 | 0.75 (0.20-2.82) | 0.669 | 0.64 (0.15-2.74) | 0.639 |
| Depressants | 6.70 (2.36-19.02) | <0.001 | 4.63 (1.37-15.60) | 0.013 | 8.50 (3.10-23.30) | <0.001 | 7.83 (2.53-24.21) | <0.001 |
| Hallucinogenics | 0.41 (0.90-1.90) | 0.242 | 0.34 (0.06-1.73) | 0.192 | 1.20 (0.43-3.34) | 0.727 | 0.98 (0.30-3.18) | 0.980 |
| Polydrug | 1.49 (0.69-3.21) | 0.309 | 1.00 (0.39-2.52) | 0.995 | 1.11 (0.49-2.53) | 0.802 | 0.98 (0.38-2.53) | 0.964 |
aOR: adjusted odds ratio; cOR; crude odds ratio; CI: confidence interval; ISS: Injury Severity Score.
Ajusted odds ratio using a multinomial logistic regression adding varibles age, sex and mechanism of injury.
Negatives: negative for drugs other than alcohol; Stimulant: positive for cocaine, amphetamines and/or methamphetamines; Depressants: positive for benzodiazepines, opiates, methadone and/or barbiturates; Hallucinogenic: positive for THC and/or PCP; Polydrug: positive for any combination of substances in the above groups.
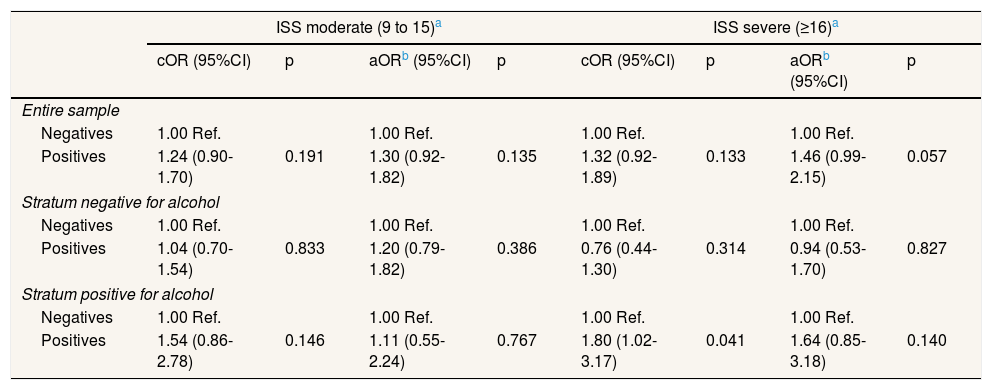
In model 2 (Table 3), when pooled data were analyzed by grouping drugs with opposite effects, no significant associations were found in the adjusted estimates.
Multivariate analysis of drugs detected and injury severity in the entire sample and by stratums positive or negative for alcohol. Model 2: grouping all drugs other than alcohol.
| ISS moderate (9 to 15)a | ISS severe (≥16)a | |||||||
|---|---|---|---|---|---|---|---|---|
| cOR (95%CI) | p | aORb (95%CI) | p | cOR (95%CI) | p | aORb (95%CI) | p | |
| Entire sample | ||||||||
| Negatives | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | ||||
| Positives | 1.24 (0.90-1.70) | 0.191 | 1.30 (0.92-1.82) | 0.135 | 1.32 (0.92-1.89) | 0.133 | 1.46 (0.99-2.15) | 0.057 |
| Stratum negative for alcohol | ||||||||
| Negatives | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | ||||
| Positives | 1.04 (0.70-1.54) | 0.833 | 1.20 (0.79-1.82) | 0.386 | 0.76 (0.44-1.30) | 0.314 | 0.94 (0.53-1.70) | 0.827 |
| Stratum positive for alcohol | ||||||||
| Negatives | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | 1.00 Ref. | ||||
| Positives | 1.54 (0.86-2.78) | 0.146 | 1.11 (0.55-2.24) | 0.767 | 1.80 (1.02-3.17) | 0.041 | 1.64 (0.85-3.18) | 0.140 |
aOR: adjusted odds ratio; cOR; crude odds ratio; CI: confidence interval; ISS: Injury Severity Score.
A separate analysis of drug subgroups defined according to their effect on the CNS allowed us to identify the specific influence of substances with CNS-depressant effects on injury severity, especially in patients who had consumed alcohol. The results of this study suggest that in the presence of alcohol, substances with a CNS-depressant effect have a strong influence on trauma severity.
We were able to distinguish between cases in which the substance was administered as part of the trauma patient's medical care and cases in which the patient had consumed the substance before the injury. This allowed us to quantify the effect of CNS-depressant substances on severity without the need to systematically exclude patients who screened positive for opiates or benzodiazepines, in contrast to similar studies that excluded these patients.21,24,26
There was a high prevalence of benzodiazepine exposure in our population of injured patients. The influence of benzodiazepines on injury prevention is an area of growing interest. Although the exact frequency of use of these nonprescribed substances is not known, it appears evident that the consumption of benzodiazepine and other psychotropic drugs is increasing.14,37
Particular attention should be given to motor vehicle crashes, which can cause serious injury. In Spain, the percentage of traffic deaths in which psychoactive drug use was detected alone or in combination with alcohol and/or other drugs has doubled in the last five years, and is now 33.3%.33 In this connection, drugs other than alcohol have begun to acquire particular relevance. The conclusions of the European DRUID (Driving Under the Influence of Drugs, Alcohol and Medicines) project38 highlight the need for increased monitoring of substances other than alcohol because their frequency of use is clearly increasing. According to the DRUID study, in some parts of Europe, drivers are more likely to be detected under the influence of drugs than under the influence of alcohol. Moreover, a systematic review by Smink et al.15 found sufficient evidence that exposure to benzodiazepines is related to a greater risk of accidents; although these authors recognize that more research is needed to clarify the relationship between the use of these drugs and injury severity. We found that the effect of benzodiazepines along with other depressants on trauma severity was very high, but only in patients who had also consumed alcohol. The biological interpretation of these results is likely to be related with the known synergistic interaction of combinations of these drugs in CNS depression. This effect impairs driving performance and the ability to react to a potential hazard by causing sedation and increasing risk-taking behavior. Driving under the combined influence of drugs and alcohol has been found to increase the risk of accidents in various ways due to their influence on the driver's vision, awareness, perception, reaction time and concentration.29
Statistical analysis with all patients who were positive for substances in a single group (model 2) allowed us to confirm that pooled data analysis by grouping drugs with opposite effects on the CNS is a potentially misleading strategy. Therefore, some associations between depressant drugs and injury severity may have been masked in previous studies.21,22,26
The profile of patients who tested positive for CNS depressant substances was different from other profiles: female sex was more frequent, age was substantially older, and falls were the most common mechanism of injury. These findings reveal the need for further analysis of the differences in these characteristics compared to the classic profile of individuals with trauma associated with alcohol and other drugs, i.e. young, male, and with injuries related to violence or traffic accidents.3,18,26,39–43 In any case, the results after adjustment for age, sex and mechanism of injury showed that these differences cannot be the cause of the heightened injury severity observed in the subgroup of patients exposed to CNS-depressant substances.
Our systematic analysis was based on all patients between 16 and 70 years of age who were admitted to a trauma hospital, with no other previous selection criteria. This sampling approach decreased the possibility of selection bias. Some previous studies were based on data obtained from national, regional or hospital trauma registries from which the authors selected records that included available information on the exposure to drugs and alcohol.16,19,21,22,27 If patient screening is not used consistently and systematically, the availability of data on substance use will depend on the physician's decision to use or omit the screening protocol at the time the patient is admitted to the emergency department. This uncertainly introduces an important source of selection bias, because physicians may be more likely to request substance use testing for more severely injured patients or for those with signs of alcohol or drug use.
Our study shares a common limitation with previous reports,14,17 i.e., the possible presence of false negative results for alcohol use in patients who were not tested for this substance at the time of admission and who subsequently denied alcohol consumption when interviewed. Fortunately, this was not the case for the other substances analyzed here, because all patients were screened with appropriate laboratory tests. On the other hand, our study could be affected by selection bias: we have not included those traumatized patients who died at the scene of the accident due to the extreme severity of their injuries; frequency of drug detection may be different in these subjects. However, statistics of substance distribution among all drivers killed in traffic accidents in Spain show that alcohol and/or psychotropic drugs are substances frequently found (29.1% of drivers killed in 2015).33 Finally, another selection bias could arise because not all hospitalized trauma patients could be screened. Nonetheless, we have no reasons to suspect an independent association between the presence of drugs and the probability of being screened.
ConclusionsWe detected an association between the presence of sedative drugs and injury severity in the subgroup of trauma patients who screened positive for alcohol consumption. We believe further knowledge is needed regarding the effect of drugs other than alcohol on trauma severity. Our results support the additional benefits of systematic screening programs for psychoactive drug use in all trauma patients. The information gained from testing would not only provide important data during clinical assessment, but would also enable the healthcare provider to offer appropriate education, counseling, or other types of intervention.
Although the effect of alcohol on the severity of the trauma and the occurrence of complications and mortality during hospitalization has been widely assessed in previous studies, the role of drugs other than alcohol remains unclear.
What does this study add to the literature?Our main finding is that in patients admitted for traumatic injuries under the influence of depressant drugs strongly increases the severity of the injuries, but only in patients also exposed to alcohol.
The corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Editor in chargeCristina Linares Gil.
Authorship contributionsAll authors contributed to the design of the study, writing and final approval of the version to be submitted. S. Cordovilla-Guardia contributed to the literature search, data analysis, data collection, data interpretation and editing. P. Lardelli-Claret contributed to the data analysis and data interpretation. R. Vilar-López contributed to the data analysis and data interpretation. F. López-Espuela contributed in the data interpretation. F. Guerrero-López contributed in the data collection and data interpretation. E. Fernández-Mondéjar contributed to the literature search, data analysis, data interpretation and editing.
FundingThis work was supported by the Dirección General de Tráfico, Spain [No. 0100DGT22389] and the Consejería de Salud, Junta de Andalucía, Spain [No. PI-0691-2013].
Conflicts of interestNone.
The results reported here are based on work done as part of the requirements for the PhD degree awarded to S. Cordovilla-Guardia. We thank K. Shashok for improving the use of English in the manuscript.