The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoSARS-CoV-2 has spread beyond the world and makes a new challenge in the breastfeeding issue. There is some disagreement among breastfeeding management in confirmed COVID-19 patients China consensus but no evidence shows the transmission via breastfeeding. This paper aims to know the risk of transmission through breastfeeding in COVID-19 patients and antibodies in breast milk.
MethodWe conducted a literature review of publicly available information to summarize knowledge about risk transmission through breastfeeding and antibody in mother confirmed COVID-19.
ResultA maternal woman was positive for COVID-19 in throat swabs show negative SARS-CoV-2 in breast milk. No evidence suggests the transmission of SARS-CoV-2 from mother to baby via vertical route or breast milk. IgG and IgA were detected in breast milk and potentially against SARS-CoV-2.
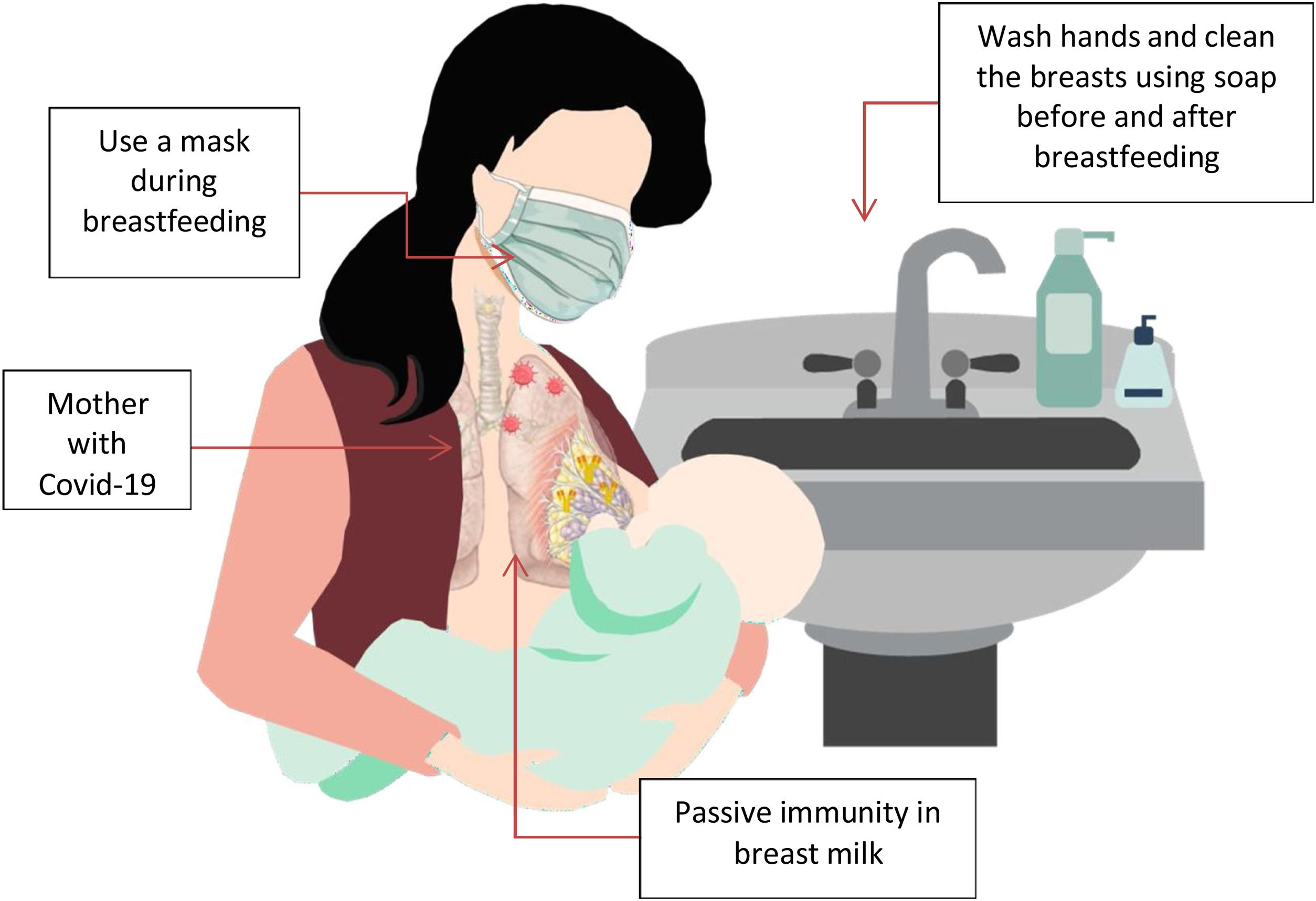
ConclusionMother with COVID-19 can continuing direct breastfeeding with appropriate hygiene precautions (using a mask and wash hand) and should remain separate (home isolation precautions) from other family members including the infant, except for breastfeeding.
The mother's own milk is considered the best source of infant nutrition.1 A large amount of evidence shows that breast milk contains a variety of bioactive agents, which can change the function of the gastrointestinal tract and immune system as well as brain development.2 Early breastfeeding has different health benefits, such as enhancing the ability to defend against infection, reducing the risk of diarrhea, and improving the survival rate of children. Starting breastfeeding as soon as possible can reduce the neonatal mortality rate by 33%.3–5 Indonesia has a program called “Inisiasi menyusui dini”, which aims to support the benefits of early breastfeeding, regardless of whether the delivery method is C-section or vaginal delivery, as long as there are no contraindications.6
But after the COVID-19, originated in Wuhan, China in December 2019 and unfortunately has spread all over the world to become a pandemic, health provider must to adjust the breastfeeding program. The International Council of Midwives (ICM) expressed concerns regarding the inappropriate protocols management of the human rights of women in childbirth and breastfeeding in perinatal period during the pandemic.7
Currently, it is uncertain whether the virus can be transmitted through breast milk; our understanding of viral transmission is limited and based on a few reports where they did not find traces of the virus in breast milk.8–10 The WHO, UNICEF, WABA, ILCA's, UNFPA, and ABM encourages women to breastfeed or to continue breastfeeding following certain recommendations and precautions based on the idea that through breast milk the babies would get antibodies and anti-infective factors that help protect newborns from getting infections.11–16 The Union of European Neonatal and Perinatal Societies advise direct breastfeeding under strict measures of infection control in asymptomatic COVID-19 mothers, but when the mothers are too sick, the neonates will be managed separately with fresh expressed breast milk.17 While CDC make a guideline that whether and how to start or continue breastfeeding should be determined by the mother in coordination with her family and healthcare providers and suggest pasteurized donor human milk.18
There is some disagreement in the literature among breastfeeding management in confirmed COVID-19 patients China's consensus violates existing evidence; they have confirmed the new coronavirus and the possibility of vertical transmission through breast milk; therefore, even in cases of suspicion, they recommend separating mother and child and interrupting breastfeeding. In their publication, they recommend that breastfeeding and/or breast milk extraction should only be permitted if the mother's PCR test result for COVID-19 is negative.10 In addition, neonatal isolation was recommended in newborns who had been suspected or confirmed SARS-CoV-2 infection.19
MethodA systematic search was conducted to identify relevant studies in the following databases: PubMed, Medline, nature, researchgate, Google Scholar, and medscape. The following search keyword were used “severe acute respiratory syndrome of coronavirus-2” or “SARS-CoV 2” or “COVID-19” or “coronavirus”, “breastfeeding” or “Transmission SARS-CoV-2 Through Breast Milk” and “antibody”. The reference lists were manually searched to identify additional relevant studies meeting inclusion criteria. We included any study that reports the epidemiology, clinical characteristics, outcomes of neonatal and detection of SARS-CoV-2 in human breast milk. No restrictions were applied.
DiscussionRisk and transmission SARS-COV-2 through breast milkBreast milk and its anti-infective and anti-inflammatory factors have become particularly important in alleviating infectious diseases. Breastfeeding also seems to be related to increased type I interferon production in infants infected with influenza virus, and in a study of 26 COVID-19 adult in an ICU environment, it was found that interferon production was compromised in 20%.20,21 The prognosis of patients and these patients is poor, the length of stay in the intensive care unit is longer, and the need for invasive ventilation is greater. A recent report found that 12 of 15 mothers (80%) previously infected with COVID-19 had a strong sIgA antibody SARS-CoV-2 immune response in their breast milk.22
A study by Chen et al. of 9 patients with pneumonia caused by COVID-19 did not find the virus in 6 patients’ samples, which came from amniotic fluid, cord blood, breast milk and oropharyngeal swabs. Three of these newborns presented molecular tests positive for COVID-19, and the authors questioned the existence of possible vertical transmission of the virus since all measures recommended for infection control were adopted. However, the samples of amniotic fluid, umbilical cord blood, and breast milk did not show the presence of the virus.19
A case study conducted at the University of Puerta Hierro with 22 mothers with neonatal COVID-19 infection showed that 20 out of 22 mothers (90.9%) chose to breastfeed their babies during hospitalization. During the follow-up period, there were no major complications and no newborn infections during breastfeeding.23 Yang et al. believe that SARS-CoV-2 is unlikely to be transmissible via breast milk, but the quality of evidence remains low.24
Therefore, the existing data so far, although not very reliable from a scientific point of view, show that the main route of COVID-19 transmission to newborns is droplet infection from caregivers, or secondly through contact with contaminated biomaterials. Vertical mother-to-fetus transmission seems to be possible, but it is not documented and does not seem to be very frequent.
As SARS-CoV-2 is transmitted via close contact and droplets, transmission from mother to infant may be possible while breastfeeding. A case series indicated that influenza infected breastfeeding women who washed hands thoroughly did not transmit to their children during a one-month follow-up, regardless of if the mothers wore a mask or not.25
Detection of SARS-CoV-2 in human breast milkSeveral case has been report supporting that SARS-CoV-2 does not transmit by breast milk.26–38 Case from Fenizia et al., Wu et al., and Gross et al., reports of positive SARS-CoV-2 RT-PCR in breast milk samples.39–41 A recent report from Italy described two maternal–infant dyads who presented with positive nasopharyngeal swabs for SARS-CoV-2 at 10 and 18 days after birth but breast milk of both mothers was negative for SARS-CoV-2 and they hypothesized that the mothers and infants were probably infected by a third person at the same time.8
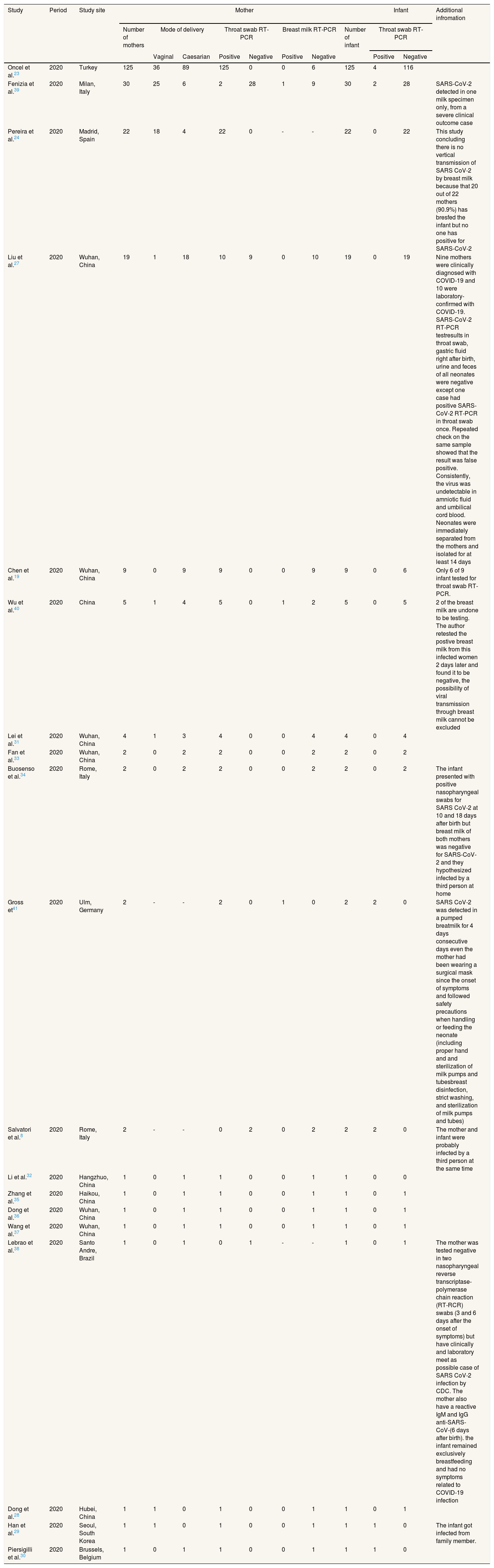
Our review (Table 1) shows that vertical mother to fetus transmission through breast milk is rare. There is no evidence novel coronavirus can pass to infants through breast milk, because the virus was not found in breast milk. This possibility cannot be completely ruled out, because the data available are based on limited clinical experience developed over few months during the novel COVID-19 pandemic, studies performed in women affected by COVID-19, and data collected during previous infectious outbreaks caused by other types of coronavirus, including severe acute respiratory syndrome, severe acute respiratory syndrome coronavirus. In 21 literature our review, we found there are 3 cases show positive SARS-CoV-2 detected in breast milk while the others literature shows no detected. In terms of associated mode in delivery there is no different between vaginal and caesarian for increase the risk of transmission. In Table 1 also show the number of infants who positive and negative in throat swab SARS-CoV-2 and we found only 3 cases have been reported positive in throat swab in infant and we also note additional information at some case with positive throat swab PCR.
Summary of characteristics of current case series and other reported cases of detection SARS-CoV-2 in human breast milk from the review of the literature.
| Study | Period | Study site | Mother | Infant | Additional infromation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of mothers | Mode of delivery | Throat swab RT-PCR | Breast milk RT-PCR | Number of infant | Throat swab RT-PCR | ||||||||
| Vaginal | Caesarian | Positive | Negative | Positive | Negative | Positive | Negative | ||||||
| Oncel et al.23 | 2020 | Turkey | 125 | 36 | 89 | 125 | 0 | 0 | 6 | 125 | 4 | 116 | |
| Fenizia et al.39 | 2020 | Milan, Italy | 30 | 25 | 6 | 2 | 28 | 1 | 9 | 30 | 2 | 28 | SARS-CoV-2 detected in one milk specimen only, from a severe clinical outcome case |
| Pereira et al.24 | 2020 | Madrid, Spain | 22 | 18 | 4 | 22 | 0 | - | - | 22 | 0 | 22 | This study concluding there is no vertical transmission of SARS CoV-2 by breast milk because that 20 out of 22 mothers (90.9%) has bresfed the infant but no one has positive for SARS-CoV-2 |
| Liu et al.27 | 2020 | Wuhan, China | 19 | 1 | 18 | 10 | 9 | 0 | 10 | 19 | 0 | 19 | Nine mothers were clinically diagnosed with COVID-19 and 10 were laboratory-confirmed with COVID-19. SARS-CoV-2 RT-PCR testresults in throat swab, gastric fluid right after birth, urine and feces of all neonates were negative except one case had positive SARS-CoV-2 RT-PCR in throat swab once. Repeated check on the same sample showed that the result was false positive. Consistently, the virus was undetectable in amniotic fluid and umbilical cord blood. Neonates were immediately separated from the mothers and isolated for at least 14 days |
| Chen et al.19 | 2020 | Wuhan, China | 9 | 0 | 9 | 9 | 0 | 0 | 9 | 9 | 0 | 6 | Only 6 of 9 infant tested for throat swab RT-PCR. |
| Wu et al.40 | 2020 | China | 5 | 1 | 4 | 5 | 0 | 1 | 2 | 5 | 0 | 5 | 2 of the breast milk are undone to be testing. The author retested the postive breast milk from this infected women 2 days later and found it to be negative, the possibility of viral transmission through breast milk cannot be excluded |
| Lei et al.31 | 2020 | Wuhan, China | 4 | 1 | 3 | 4 | 0 | 0 | 4 | 4 | 0 | 4 | |
| Fan et al.33 | 2020 | Wuhan, China | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 0 | 2 | |
| Buosenso et al.34 | 2020 | Rome, Italy | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 2 | 0 | 2 | The infant presented with positive nasopharyngeal swabs for SARS CoV-2 at 10 and 18 days after birth but breast milk of both mothers was negative for SARS-CoV-2 and they hypothesized infected by a third person at home |
| Gross et41 | 2020 | Ulm, Germany | 2 | - | - | 2 | 0 | 1 | 0 | 2 | 2 | 0 | SARS CoV-2 was detected in a pumped breatmilk for 4 days consecutive days even the mother had been wearing a surgical mask since the onset of symptoms and followed safety precautions when handling or feeding the neonate (including proper hand and and sterilization of milk pumps and tubesbreast disinfection, strict washing, and sterilization of milk pumps and tubes) |
| Salvatori et al.8 | 2020 | Rome, Italy | 2 | - | - | 0 | 2 | 0 | 2 | 2 | 2 | 0 | The mother and infant were probably infected by a third person at the same time |
| Li et al.32 | 2020 | Hangzhuo, China | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | |
| Zhang et al.35 | 2020 | Haikou, China | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | |
| Dong et al.36 | 2020 | Wuhan, China | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | |
| Wang et al.37 | 2020 | Wuhan, China | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | |
| Lebrao et al.38 | 2020 | Santo Andre, Brazil | 1 | 0 | 1 | 0 | 1 | - | - | 1 | 0 | 1 | The mother was tested negative in two nasopharyngeal reverse transcriptase-polymerase chain reaction (RT-RCR) swabs (3 and 6 days after the onset of symptoms) but have clinically and laboratory meet as possible case of SARS CoV-2 infection by CDC. The mother also have a reactive IgM and IgG anti-SARS-CoV-(6 days after birth). the infant remained exclusively breastfeeding and had no symptoms related to COVID-19 infection |
| Dong et al.28 | 2020 | Hubei, China | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | |
| Han et al.29 | 2020 | Seoul, South Korea | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | The infant got infected from family member. |
| Piersigilli et al.30 | 2020 | Brussels, Belgium | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | |
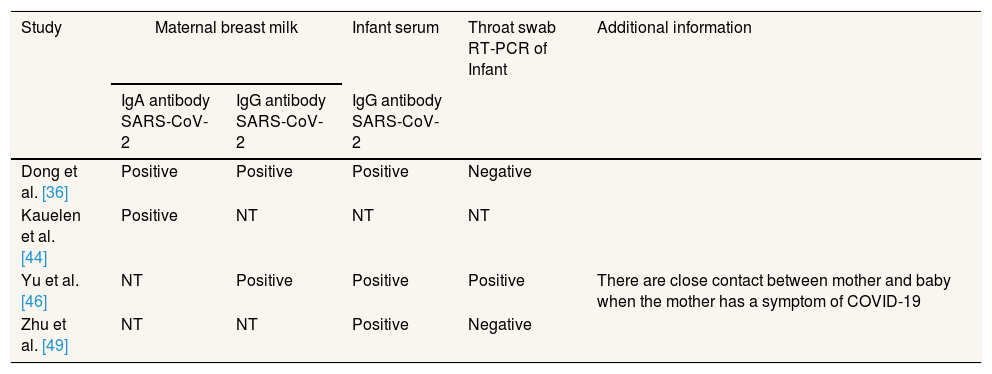
Breastfeeding has been proven to have many benefits for child especially the breast milk contains antibodies such as IgA, IgM, IgG. Circulating antibodies can diffuse into breast milk and pass on to offspring, giving them passive immunity. Newborns will rely on passive immunity from the mother. From this statement it becomes a hypothesis of several studies to see how to provide breast milk with COVID-19 on the health of newborns.
Dong et al. determined the antibody to SARS-CoV-2 in breast milk's mother who confirmed with COVID-19. The titers of IgA antibody in breast milk elevated in positive throat swabs SARS-CoV-2 mother. They also show that there is no detection of SARS-CoV-2 in the mother's body fluids (especially in breast milk) serially collected after delivery when her throat swabs showing positive. No neonate had positive result for SARS-CoV-2 RNA at the birth.28 Human milk IgA provides a key antibacterial defense Inhibition of pathogenic bacteria on neonatal gastrointestinal tract Attaches to the mucosal surface, neutralizes microbial toxins, and provides passive.8 IgA mostly produced in lamina propria adjacent to mucosal. Secretory immunoglobulin (sIgA) acts directly on the mucosal surface by inhibiting the binding of microbes to the host epithelial cell receptors and trapping pathogenic microorganisms in the mucus and increasing intestinal ciliary activity. In addition, sIgA can neutralize SARS-CoV-2 before they reach and bind the epithelial cellsWith this mechanism, sIgA breast milk can provides protection against the entry of the SARS-CoV-2 virus on the mucosal surface of the airways.42
Based on prospective case control study by van Keulen et al. explained that breast milk contains specific IgA antibody for SARS-CoV-2 on 24 of the 29 confirmed cases (83%) based on swab tests and 6 of the 9 suspected cases (67%).43 Besides IgA, some protective antibody can be passed by breastfeeding from the mother to the offspring, preventing or decreasing the severity the children's diseases such IgM and IgG. Case report by Yu et al., the mother's milk was positive for SARS-CoV-2 IgG and negative for IgM and on hospital day 14, the infant's serum was positive for both SARS-CoV-2 IgG and IgM, suggesting either breast milk transfer to the infant or infant de novo production of the IgG and/or IgM, or both mechanisms.44
In the study of Abuidhail et al. was found that IgG concentrations had a linear relationship with breastfeeding activity for 6 months. So the activity of breastfeeding can affect the concentration of IgG in breast milk to protect the baby from infection.45 IgG is the main antibody in secondary immune response if there is reinfection. IgGs such as IgG3 and IgG1 can attack the viral envelope glycoprotein so that this will provide an effective systemic antibody for viruses. IgG also acts as an antibody that degrades intracellular viruses by binding to a crystallizable cytosolic fragment (Fc) motif containing -21 tripartite receptor (TRIM21).46
Study of Kohler et al., 6 mothers with confirmed COVID-19, SARS-CoV-19 was not detected in the serum or throat swab by RT-PCR in any of their newborns. But virus-specific antibodies were detected in neonatal blood sera samples. The IgG concentrations were elevated in 5 infants.47
IgG is passively transferred across the placenta from mother to fetus beginning at the end of the second trimester and reaches high levels at the time of birth.47 All cases we shown in Table 2.
Summary of current case series and other reported cases of detection antibody SARS-CoV-2 in human breast milk from the review of the literature. (NT): Not tested.
| Study | Maternal breast milk | Infant serum | Throat swab RT-PCR of Infant | Additional information | |
|---|---|---|---|---|---|
| IgA antibody SARS-CoV-2 | IgG antibody SARS-CoV-2 | IgG antibody SARS-CoV-2 | |||
| Dong et al. [36] | Positive | Positive | Positive | Negative | |
| Kauelen et al. [44] | Positive | NT | NT | NT | |
| Yu et al. [46] | NT | Positive | Positive | Positive | There are close contact between mother and baby when the mother has a symptom of COVID-19 |
| Zhu et al. [49] | NT | NT | Positive | Negative | |
It has been explained that the risk of transmission and transmission of SARS-Cov-2 through breast milk is minimal. In addition, there are specific antibodies that can against SARS-CoV-2 as passive immunity for babies as body defense. WHO, UNICEF, WABA, ILCA's, UNFPA, and ABM recommend continuing to breastfeed mothers with COVID-19. We also recommend several provisions for breastfeeding in mothers with COVID-19.
Skin contact help effectiveness of breastfeeding and improve body temperature regulation, blood sugar control and mother–infant attachment, and reduce the mortality and risk of serious infections in low-birth-weight infants. Skin to skin contact also increase psycologic correlation between baby and mother. The important thing is skin to skin breastfeeding better than indirect breastfeeding such as use pumping equipment.48 Mother with moderate until severe illness cannot breastfeeds directly, so the best choice is indirect breastfeeding. The breast tube and container should be clean every time. Strict hand hygiene must be observed when pump and storage the breast milk.49
Infection control and prevention is very important while breastfeeding. Especially with direct breastfeeding, droplets containing viruses on the surface of the mother's body can increase the risk of the baby becoming infected. Based on previous study by Pandofi et al. concluded that mothers with symptoms should clean their hands thoroughly with soap and air before touching the baby and cover their nose and mouth with a tissue when sneezing or coughing when in contact with the baby.50 From a study by Cheema et al. also concluded that asymptomatic and mildly ill mothers are recommended for Mothers should wear a mask when breastfeeding and wash their hands and breasts with soap and water before breastfeeding. During intervals between feedings it is advisable to place the baby at least 2 meters apart.51
Based on study by Gilany concluded that mothers with COVID-19 should limit contact with their babies except while breastfeeding. When breastfeeding, babies are very vulnerable to droplets from the mother through respiratory secretions, so the mother must wear a mask when breastfeeding. Joint care is permitted provided that there are no other patients in the room and the baby is in a separate bed with a minimum distance of two meters from the mother's bed. There should be another healthy adult caring for the newborn in the room. If the mother is in moderate to severe condition it is recommended for use by the mother's baby. From all recommendation and literature, we conclude the recommendation breastfeeding for mother with explanation through Fig. 1.
ConclusionNo evidence suggests transmission of SARS-CoV-2 from mother to baby via vertical route or breast milk. A maternal woman was positive COVID-19 undergoing therapy tested in throat swabs but negative tested in other body fluids (including breast milk), and she had IgG and IgA detected in breast milk against SARS-CoV-2. Mother with COVID-19 can continuing direct breastfeeding with appropriate hygiene precautions and should remain separate (home isolation precautions) from other family members including the infant, except for breastfeeding.
FundingNo funding sources.
Ethical approvalNot required.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.