Opioid overdose is still the first cause of preventable death among young men in Barcelona. Sound knowledge of opioid overdose prevention is important to avoid complications and deaths. This study aimed to identify the factors associated with limited knowledge of overdose prevention and to assess the possible effect of treatment and overdose prevention training programs on this variable.
MethodsFrom October 2008 to March 2009, current injecting opioid users attending harm reduction centers in Catalonia (Spain) were interviewed. Crude and adjusted prevalence ratios of limited knowledge about overdose prevention were calculated by adjusting Poisson regression models with a robust variance.
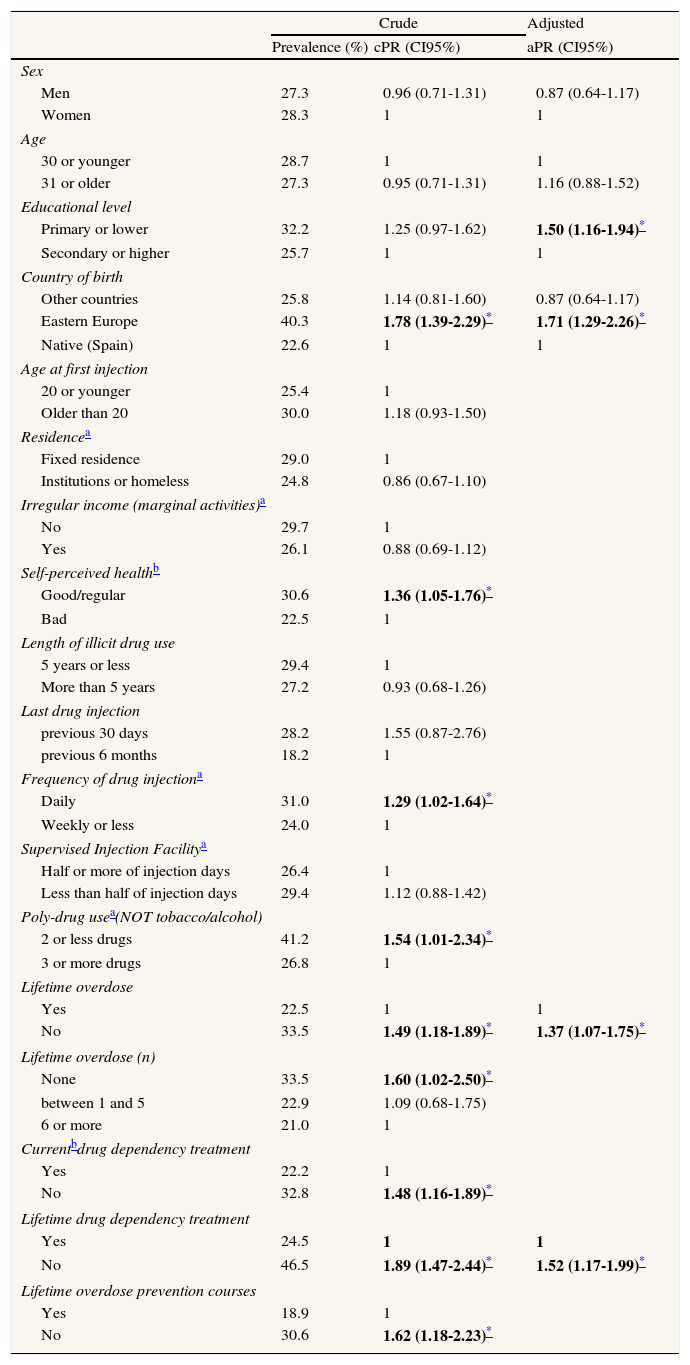
ResultsIn this sample, 28.7% of clients had limited knowledge of overdose prevention. Factors associated with limited knowledge were country of origin, never having received treatment for drug dependency, having a low educational level, and never having experienced an overdose. In contrast, treatment at the time of the interview was not associated with a lower prevalence of limited knowledge about overdose prevention.
ConclusionsThese findings suggest that preventive programs would benefit from accounting for linguistic and educational limitations and from participation in every treatment episode. Comprehensiveness and broad coverage of such programs could help to maximize their impact.
La sobredosis por opioides sigue siendo la primera causa de muerte prevenible entre hombres jóvenes en Barcelona. El conocimiento profundo acerca de la prevención de sobredosis es importante a fin de evitar complicaciones y muertes. Los objetivos de este estudio fueron la identificación de aquellos factores asociados a un conocimiento limitado acerca de la prevención de sobredosis, y la evaluación del posible efecto sobre dicha variable del tratamiento y de la asistencia a talleres de prevención de sobredosis.
MétodosEstudio transversal, mediante encuesta a usuarios de opioides por vía parenteral que acudieron a centros de reducción de daños de Cataluña entre octubre de 2008 y marzo de 2009. Se obtuvieron ratios de prevalencia crudas y ajustadas de Conocimiento limitado sobre prevención de sobredosis mediante la realización de modelos de regresión de Poisson con varianza robusta.
ResultadosEl 28,7% de los usuarios entrevistados presentaba Conocimiento limitado sobre prevención de sobredosis. Los factores asociados a dicho Conocimiento limitado fueron el país de origen, no haber recibido tratamiento por el consumo de drogas, tener un menor nivel educativo, y nunca haber sufrido una sobredosis. El hecho de estar en tratamiento en el momento de la entrevista no se asoció a una menor prevalencia de conocimiento limitado sobre prevención de sobredosis.
ConclusionesEstos hallazgos sugieren que los programas de prevención de sobredosis se verían beneficiados por tener en cuenta posibles limitaciones lingüísticas y educacionales, así como por estar integrados en todos los episodios de tratamiento. La exhaustividad y una cobertura elevada pueden ayudar a maximizar el impacto de dichos programas.
Overdose is a major cause of avoidable death among young people, and the main cause of death among injecting drug users (IDUs). Overdose accounts for about 6500 deaths per year in the European Union (EU).1 In Spain, injected opioid use has progressively declined due to the HIV/AIDS epidemic, as well as to cultural and market changes.2 However, Catalonia, an autonomous region within Spain, still presents a relatively high proportion of injecting heroin users, as compared with the rest of the country.3
Opioid overdose can be fatal or non-fatal, and both can be prevented. Non-fatal overdose is very frequent among opioid users, with an annual prevalence ranging from 9 to 22%.4,5 Opioid overdose can be prevented by avoiding certain risk factors and risky behaviors, such as combining heroin with other drugs, especially central nervous system depressants, and resuming heroin use after an abstinence period. Opioid users employing the injected route of administration are at higher risk of suffering an overdose than those using other administration routes.4,6 Other risk factors for suffering an opioid overdose have been extensively described elsewhere.4,7–10 Once an overdose does occur, witnesses may engage in certain interventions to minimize its consequences, such as searching for help and responding to overdose.8,11–15 Most overdose-related deaths occur in the presence of others, frequently other opioid users. The prevention of fatal consequences of an overdose depend at least partially on how rapidly medical assistance is provided.16,17 Preventive programs aim to increase knowledge about overdose risk factors, enhance recognition of an overdose, and train in first aid techniques and in the use of naloxone (an opioid antagonist which can safely and effectively revert overdoses).14 However, various interventions are needed at several levels (individual, community, service providers, and society as a whole) in order to have a significant impact in reducing the level of fatal overdose.18
The present study focuses on self-reported knowledge about overdose prevention among injecting opioid users attending harm reduction centers in Catalonia. It aims to quantify the level of knowledge about overdose prevention in injecting opioid users, to assess to what extent do treatment episodes and overdose prevention training programs affect this level of knowledge, and to identify which other factors are associated with limited knowledge about overdose prevention in this population.
MethodsStudy design and SubjectsBetween October 2008 and March 2009, injecting drug users attending harm reduction centers in Catalonia (Spain) were interviewed. Inclusion criteria were having used opioids (heroin, methadone or other opioids) and injecting any drug in the 6 months prior to the interview, and having signed an informed consent form. This informed consent form clearly stated the confidentiality of the study. The 18 Harm reduction centers included needle exchange programs, outreach programs, and three supervised injecting facilities. Most harm reduction centers included in the study (11 out of 18) were located in Barcelona or in its metropolitan area. A convenience stratified sample of injecting opioid users was selected (n=729).19 Assignment to strata was proportional to the volume of visits in each center and to the percentage of individuals in each center by country of birth. In centers with less than 5% foreign-born clients, only native participants were recruited. Participants were randomly selected within harm reduction centers.
Data CollectionFace to face interviews were conducted in each center by trained interviewers using an anonymous structured questionnaire, adapted from the Itinere3 and World Health Organization20 questionnaires. Information was collected on socio-demographic variables, patterns of drug use, use of social and health services, and non-fatal opioid overdoses. The questionnaire was provided in 4 languages (Spanish, Romanian, English, and French), and piloted with a group of 15 IDUs from several countries before its administration. Interviewers were weekly monitored to control the quality of data collection.
Overdose was defined as an episode occurring due to heroin, methadone or other opioids use, in which after drug use, extreme difficulty in breathing, loss of consciousness and problems waking up or recovering consciousness, and sometimes bluish skin or lips would appear.21 Participants were asked, in two open ended questions, to list the three main reasons for an overdose to occur, as well as the three main actions to undertake in case of witnessing an overdose. Respondents received 24€ to encourage participation. The study protocol of the REDAN study was approved by an Ethics Committee Review Board (Hospital Universitari Germans Trias i Pujol, Badalona, Spain).
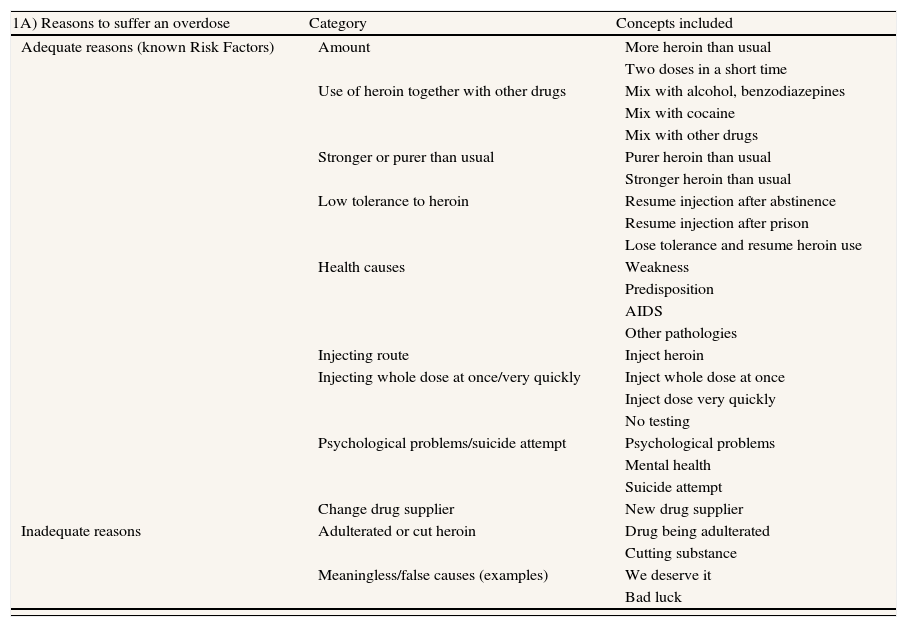
VariablesDependent variableReasons and actions cited in each open ended question were collected as transcribed verbatim and, based on similar underlying concepts, were classified in 11 recoded reasons (of which 9 were risk factors and 2 were inadequate reasons) and 15 recoded actions (9 recommended actions and 6 inadequate actions). Adequacy was based on the literature;7,8,10,12 see all categories and example verbatim in Table 1. This classification was reviewed and agreed upon separately by three experienced researchers (co-authors MTB -M.D. PhD-, ASR –MPH PhD, C.V -M.D. PhD-). A regional working document was used to resolve inconsistencies.22 Two variables were created, “Reasons to suffer an overdose”, and “Actions to undergo if witnessing another person suffering an overdose”.
Concepts included in each category of recoded answers to open-ended questions (OEQs). 1A) Answers to the OEQ: “List the three main reasons for overdose you can think of”. 1B) Answers to the OEQ: “List the three main actions to undertake in case of witnessing an overdose in a peer”.
| 1A) Reasons to suffer an overdose | Category | Concepts included |
| Adequate reasons (known Risk Factors) | Amount | More heroin than usual |
| Two doses in a short time | ||
| Use of heroin together with other drugs | Mix with alcohol, benzodiazepines | |
| Mix with cocaine | ||
| Mix with other drugs | ||
| Stronger or purer than usual | Purer heroin than usual | |
| Stronger heroin than usual | ||
| Low tolerance to heroin | Resume injection after abstinence | |
| Resume injection after prison | ||
| Lose tolerance and resume heroin use | ||
| Health causes | Weakness | |
| Predisposition | ||
| AIDS | ||
| Other pathologies | ||
| Injecting route | Inject heroin | |
| Injecting whole dose at once/very quickly | Inject whole dose at once | |
| Inject dose very quickly | ||
| No testing | ||
| Psychological problems/suicide attempt | Psychological problems | |
| Mental health | ||
| Suicide attempt | ||
| Change drug supplier | New drug supplier | |
| Inadequate reasons | Adulterated or cut heroin | Drug being adulterated |
| Cutting substance | ||
| Meaningless/false causes (examples) | We deserve it | |
| Bad luck |
| 1B) Actions if witnessing an overdose | Category | Concepts included |
| Adequate actions (Recommendations) | Call emergency services | Call an ambulance |
| Call health emergency | ||
| First aid | Mouth-to-mouth resuscitation | |
| Cardiopulmonary resuscitation (CPR) | ||
| Recovery position | ||
| Wake up/Keep awake | Wake him/her up | |
| Do not allow falling asleep | ||
| Assessment | Check if person is conscious | |
| Check pulse | ||
| Check pupils | ||
| Call police/call for help | Call police | |
| Call friends or relatives asking for help | ||
| Search for help | ||
| Naloxone | Inject naloxone | |
| Inject antidote | ||
| Observation | Observe him/her | |
| Stay next to him/her | ||
| Facilitate breathing | Make sure airway is clear | |
| Loosen tight clothes | ||
| Remove syringe | Remove syringe | |
| Inadequate actions | Shower | Shower person |
| Put him/her in the bathtub | ||
| Hit | Hit him/her violently | |
| Shake him/her violently | ||
| Make the person move/stand up | Make him/her run or walk | |
| Help him/her stand up | ||
| Inject substance other than naloxone | Inject saline | |
| Inject citric | ||
| Inject cocaine | ||
| Abandon him/her | I leave the place of the event | |
| I leave him/her alone | ||
| Meaningless actions (Examples) | I laugh at him/her | |
| I panic |
The dependent variable “Limited knowledge about overdose prevention” was created by grouping categories of recoded reasons and actions. When a participant mentioned a maximum of 2 items (including evidence-based risk factors and adequate actions), he/she was considered to present “limited knowledge about overdose prevention”.
Independent variablesTo assess the effect of treatment and training episodes in their level of knowledge about overdose prevention, participants were asked whether they were receiving treatment for their drug dependency at the time of the interview, and whether they had ever undergone treatment. Drug dependency treatment included drug-free residential treatment or admission in therapeutic communities, in-hospital detoxification, out-patient drug-free treatment, methadone maintenance, and other medication/other treatments. Participants were also asked if they had ever attended overdose prevention training courses.
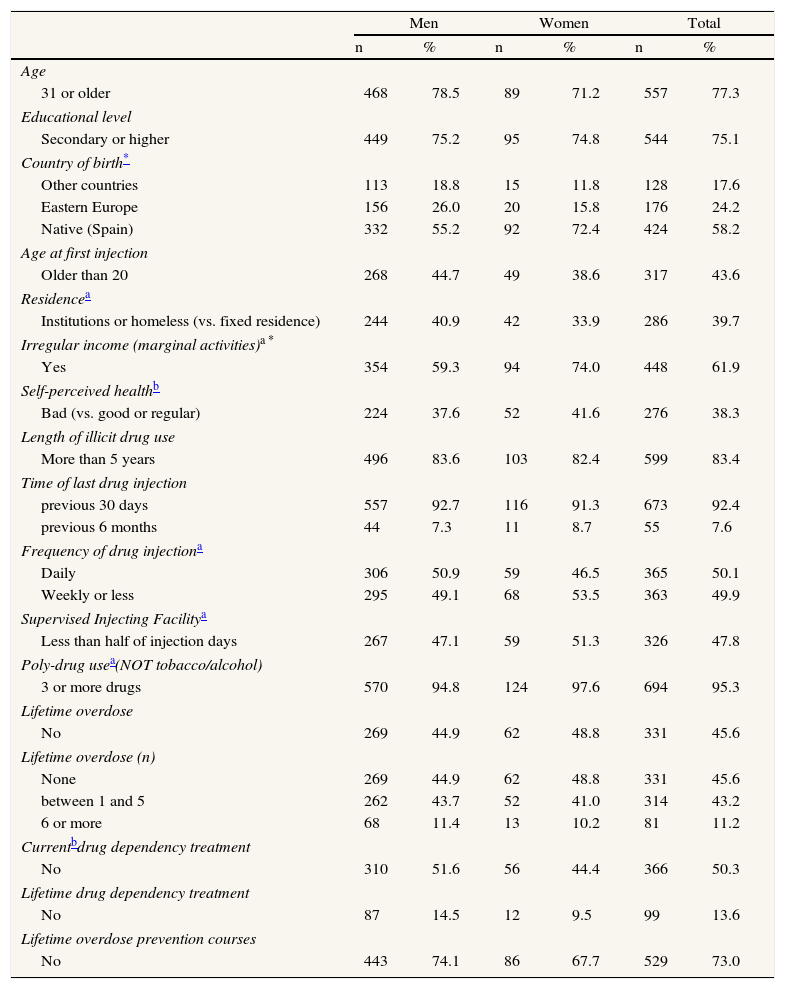
Socio-demographic information was collected. Cultural and language background was accounted for by regrouping countries of birth in three categories: native (Spanish), Eastern European (or former Soviet Republic countries; Georgia, Romania, Russia, Bulgaria, the former Yugoslavian countries, Albania, Armenia, Belarus, Lithuania, Poland, Czech Republic, and Ukraine), and other countries (a heterogeneous category including EU-15 and other Western European, African, Asian, and American countries). See Table 2 for a complete listing of explicative variables included in this study.
General characteristics of opioid injectors recruited in Catalonian harm reduction centres, 2008-2009.
| Men | Women | Total | ||||
| n | % | n | % | n | % | |
| Age | ||||||
| 31 or older | 468 | 78.5 | 89 | 71.2 | 557 | 77.3 |
| Educational level | ||||||
| Secondary or higher | 449 | 75.2 | 95 | 74.8 | 544 | 75.1 |
| Country of birth* | ||||||
| Other countries | 113 | 18.8 | 15 | 11.8 | 128 | 17.6 |
| Eastern Europe | 156 | 26.0 | 20 | 15.8 | 176 | 24.2 |
| Native (Spain) | 332 | 55.2 | 92 | 72.4 | 424 | 58.2 |
| Age at first injection | ||||||
| Older than 20 | 268 | 44.7 | 49 | 38.6 | 317 | 43.6 |
| Residencea | ||||||
| Institutions or homeless (vs. fixed residence) | 244 | 40.9 | 42 | 33.9 | 286 | 39.7 |
| Irregular income (marginal activities)a * | ||||||
| Yes | 354 | 59.3 | 94 | 74.0 | 448 | 61.9 |
| Self-perceived healthb | ||||||
| Bad (vs. good or regular) | 224 | 37.6 | 52 | 41.6 | 276 | 38.3 |
| Length of illicit drug use | ||||||
| More than 5 years | 496 | 83.6 | 103 | 82.4 | 599 | 83.4 |
| Time of last drug injection | ||||||
| previous 30 days | 557 | 92.7 | 116 | 91.3 | 673 | 92.4 |
| previous 6 months | 44 | 7.3 | 11 | 8.7 | 55 | 7.6 |
| Frequency of drug injectiona | ||||||
| Daily | 306 | 50.9 | 59 | 46.5 | 365 | 50.1 |
| Weekly or less | 295 | 49.1 | 68 | 53.5 | 363 | 49.9 |
| Supervised Injecting Facilitya | ||||||
| Less than half of injection days | 267 | 47.1 | 59 | 51.3 | 326 | 47.8 |
| Poly-drug usea(NOT tobacco/alcohol) | ||||||
| 3 or more drugs | 570 | 94.8 | 124 | 97.6 | 694 | 95.3 |
| Lifetime overdose | ||||||
| No | 269 | 44.9 | 62 | 48.8 | 331 | 45.6 |
| Lifetime overdose (n) | ||||||
| None | 269 | 44.9 | 62 | 48.8 | 331 | 45.6 |
| between 1 and 5 | 262 | 43.7 | 52 | 41.0 | 314 | 43.2 |
| 6 or more | 68 | 11.4 | 13 | 10.2 | 81 | 11.2 |
| Currentbdrug dependency treatment | ||||||
| No | 310 | 51.6 | 56 | 44.4 | 366 | 50.3 |
| Lifetime drug dependency treatment | ||||||
| No | 87 | 14.5 | 12 | 9.5 | 99 | 13.6 |
| Lifetime overdose prevention courses | ||||||
| No | 443 | 74.1 | 86 | 67.7 | 529 | 73.0 |
Proportions were calculated in relation to those who answered each question for the total sample and separated by sex. The proportion of cases citing each reason and action category was calculated per country of birth.
The association between limited knowledge about overdose prevention and a set of explanatory variables was examined using bivariate and multivariate methods. In bivariate methods statistical significance of differences in the prevalence of limited knowledge was tested using the Chi-square test, rejecting the null hypothesis when p<0.05. In multivariate analysis different Poisson regression models with robust error variance were fitted,23 obtaining Prevalence Ratios (PRs) and 95% confidence intervals. Finally, a multivariate Poisson regression model with robust variance (backward model) was fitted, obtaining adjusted PRs. All variables were included in the first model and rejected in a stepwise way, according to statistical significance. Sex and age were retained in the model despite not reaching statistical significance. Statistical analyses were performed using Stata 11.0.
ResultsGeneral characteristics of the sampleThe study included 729 participants, of which 379 were recruited within the city of Barcelona. The sample was 82.6% male, median 36 years of age (20-59 years). Most participants had completed secondary education (Table 2). There were no statistically significant differences in most characteristics by sex, with the exceptions of having received most of their income in the previous 6 months from irregular or marginal activities and being immigrant. The vast majority of participants had injected drugs during the previous month, but only half of them injected drugs on a daily basis. In the previous 6 months, almost all participants were using at least 3 different drugs (95.3%) and had used syringe exchange programs (95.6%; data not shown). Most participants had at some point in their lives received drug dependency treatment (86.4%), and half underwent treatment at the time of the interview (49.7%), but only 27% had ever attended overdose prevention courses.
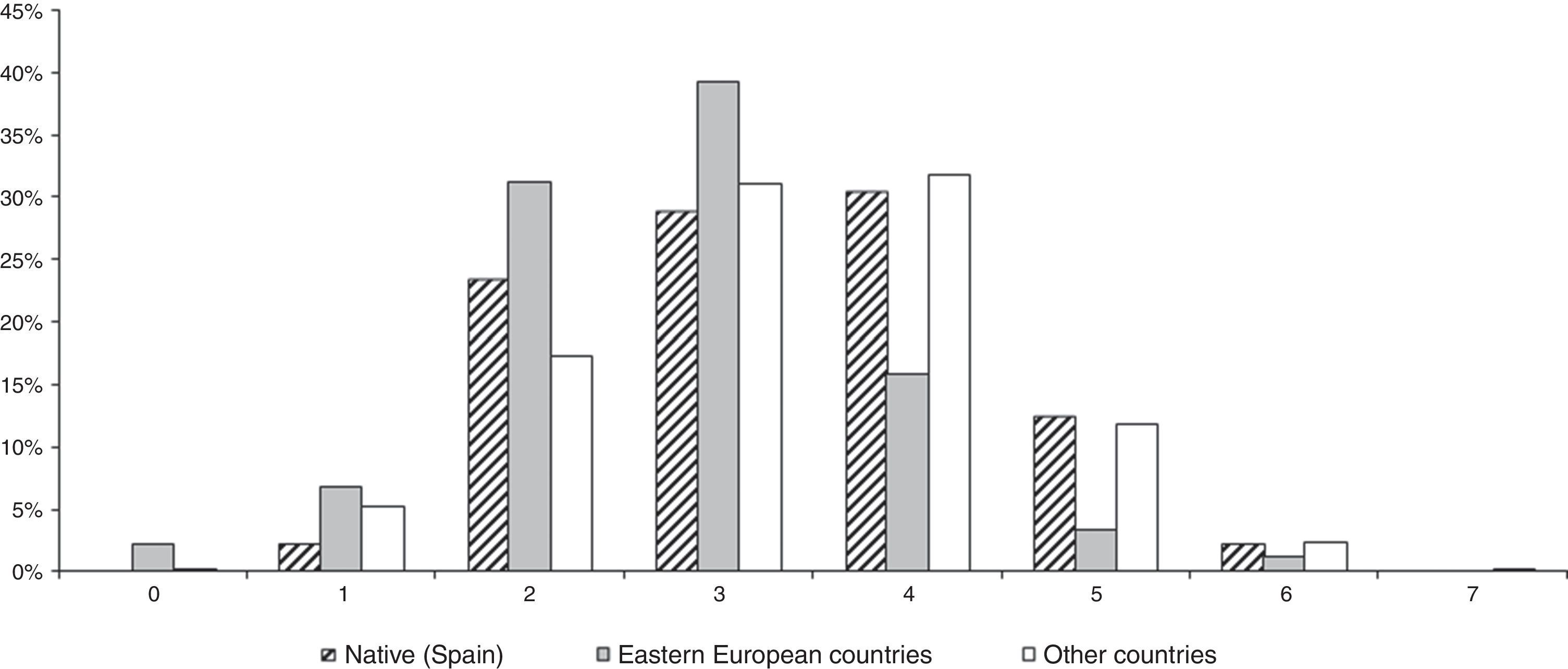
Prevalence of Limited Knowledge about Overdose Prevention and associated factorsOverall, 28.7% of participants had limited knowledge about overdose prevention, since they could not cite more than two risk factors and/or adequate actions to undertake if witnessing an overdose. When separated by origin, 25.7% of native respondents presented limited knowledge, versus 40.4% of participants from Eastern Europe and 22.6% among participants from other countries (Figure 1). Differences in prevalence of limited knowledge were significant when comparing native and Eastern Europeans (p<0.001) as well as when comparing Eastern Europeans with immigrants from other countries (p<0.01).
Crude prevalence of limited knowledge about overdose prevention was significantly higher in people who came from Eastern European countries, were not receiving or had never received drug dependency treatment, never had suffered an overdose, never had attended overdose prevention courses, injected drugs on a daily basis, or had better or similar self-perceived health than their age peers (Table 3). Use of supervised injecting facilities was not significantly associated with knowledge about overdose prevention.
Predictors of limited knowledge about overdose prevention among opioid injectors recruited in Catalonian harm reduction centres, 2008-2009.
| Crude | Adjusted | ||
| Prevalence (%) | cPR (CI95%) | aPR (CI95%) | |
| Sex | |||
| Men | 27.3 | 0.96 (0.71-1.31) | 0.87 (0.64-1.17) |
| Women | 28.3 | 1 | 1 |
| Age | |||
| 30 or younger | 28.7 | 1 | 1 |
| 31 or older | 27.3 | 0.95 (0.71-1.31) | 1.16 (0.88-1.52) |
| Educational level | |||
| Primary or lower | 32.2 | 1.25 (0.97-1.62) | 1.50 (1.16-1.94)* |
| Secondary or higher | 25.7 | 1 | 1 |
| Country of birth | |||
| Other countries | 25.8 | 1.14 (0.81-1.60) | 0.87 (0.64-1.17) |
| Eastern Europe | 40.3 | 1.78 (1.39-2.29)* | 1.71 (1.29-2.26)* |
| Native (Spain) | 22.6 | 1 | 1 |
| Age at first injection | |||
| 20 or younger | 25.4 | 1 | |
| Older than 20 | 30.0 | 1.18 (0.93-1.50) | |
| Residencea | |||
| Fixed residence | 29.0 | 1 | |
| Institutions or homeless | 24.8 | 0.86 (0.67-1.10) | |
| Irregular income (marginal activities)a | |||
| No | 29.7 | 1 | |
| Yes | 26.1 | 0.88 (0.69-1.12) | |
| Self-perceived healthb | |||
| Good/regular | 30.6 | 1.36 (1.05-1.76)* | |
| Bad | 22.5 | 1 | |
| Length of illicit drug use | |||
| 5 years or less | 29.4 | 1 | |
| More than 5 years | 27.2 | 0.93 (0.68-1.26) | |
| Last drug injection | |||
| previous 30 days | 28.2 | 1.55 (0.87-2.76) | |
| previous 6 months | 18.2 | 1 | |
| Frequency of drug injectiona | |||
| Daily | 31.0 | 1.29 (1.02-1.64)* | |
| Weekly or less | 24.0 | 1 | |
| Supervised Injection Facilitya | |||
| Half or more of injection days | 26.4 | 1 | |
| Less than half of injection days | 29.4 | 1.12 (0.88-1.42) | |
| Poly-drug usea(NOT tobacco/alcohol) | |||
| 2 or less drugs | 41.2 | 1.54 (1.01-2.34)* | |
| 3 or more drugs | 26.8 | 1 | |
| Lifetime overdose | |||
| Yes | 22.5 | 1 | 1 |
| No | 33.5 | 1.49 (1.18-1.89)* | 1.37 (1.07-1.75)* |
| Lifetime overdose (n) | |||
| None | 33.5 | 1.60 (1.02-2.50)* | |
| between 1 and 5 | 22.9 | 1.09 (0.68-1.75) | |
| 6 or more | 21.0 | 1 | |
| Currentbdrug dependency treatment | |||
| Yes | 22.2 | 1 | |
| No | 32.8 | 1.48 (1.16-1.89)* | |
| Lifetime drug dependency treatment | |||
| Yes | 24.5 | 1 | 1 |
| No | 46.5 | 1.89 (1.47-2.44)* | 1.52 (1.17-1.99)* |
| Lifetime overdose prevention courses | |||
| Yes | 18.9 | 1 | |
| No | 30.6 | 1.62 (1.18-2.23)* | |
After adjusting for other factors, those participants with primary or lower educational level (PR=1.50, 95% CI:1.16-1.94), coming from Eastern European countries (PR=1.71, 95%CI: 1.29-2.26), never having undergone drug dependency treatment (PR=1.52, 95% CI:1.17-1.99) and never having suffered an overdose (PR=1.37, 95% CI:1.07-1.75) had higher probability of presenting limited knowledge about overdose prevention (Table 3).
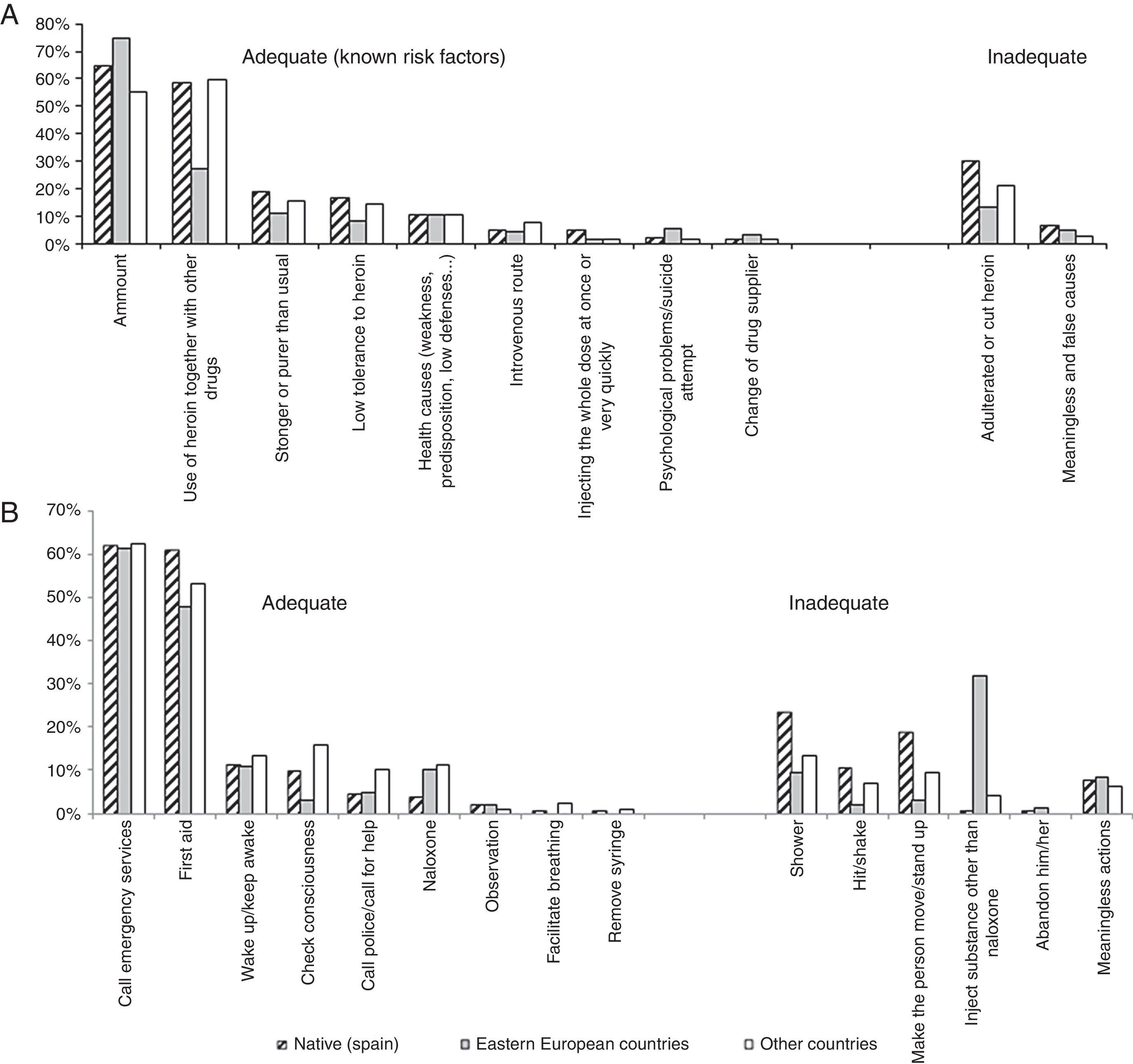
Self-Perceived General Reasons for Overdose and Actions in Case of Witnessing an OverdoseIn this sample, 30.6% of injecting opioid users did not identify any risk factor for overdose, 51.3% identified one and 18.1% identified more than one. Native participants cited more frequently inadequate reasons for overdose, and especially the use of adulterated or cut heroin (Figure 2a). Notably, 5.2% cited the use of the injected route of administration as a risk factor for an opioid overdose.
Percentages of participants mentioning each reason and action related to opioid overdose by country of birth among opioid injectors recruited in Catalonian harm reduction centres, 2008-2009.
A) Reasons to suffer an opioid overdose
B) Actions to undertake in case of witnessing an opioid overdose.
In addition, 35.9% IDUs in the sample did not identify any adequate action in case of witnessing an overdose, 61.1% identified one, and only 3% identified two. Calling an emergency service (61.9%) and giving first aid (56.5%) were the most frequently cited adequate actions in case of witnessing an overdose. Naloxone administration was the sixth most frequent cited adequate action, and native participants seemed less familiar with this action (3.8%) than their foreign peers (10.1% Eastern Europeans, 11.1% other countries). In contrast, Eastern European participants cited very frequently the injected administration of substances different from naloxone (typically saline or water with lemon), whereas native participants very rarely mentioned this inadequate practice (Figure 2b).
DiscussionThe main findings in the present study were: 1) Factors associated with limited knowledge about overdose prevention were never having attended drug dependency treatment, having a low educational level, never having suffered an overdose, and coming from an Eastern European country; 2) Contact with other preventive resources (supervised injecting facilities, overdose prevention courses) did not predict increased knowledge about overdose prevention; 3) Almost 40% of respondents reported inadequate actions in case of witnessing an overdose, and only 5.2% recognized the injected route of administration as a risk factor for suffering an overdose; 4) Almost three quarters of the sample had never received training in overdose prevention.
Study limitations and strengthsThis study poses the strength of exploring in detail a relevant topic which has been poorly studied, namely knowledge about opioid overdose prevention in an IDU population. Although we cannot assure that the sample is representative of opioid injectors as a whole in Catalonia, this study reaches a large sample out of a hidden population, generally very difficult to access and which bears enormous social barriers. The sample is representative of those injecting opioid users who attended Catalonian harm reduction centers, since assignment to strata was proportional to the volume of visits in each center and to the percentage of individuals in each center by country of birth, and since sample selection was random within the centers.
The dependent variable, limited knowledge about overdose prevention, is not straightforward, but it is informative about those participants presenting reduced knowledge about overdose prevention. This variable includes information about risk factors and adequate peer assistance. There is an underreporting of well-known risk factors for overdose among this sample, such as using the injected route of administration. It is possible that participants do not identify such risk factors spontaneously, but would recognize them if they would appear as a list of pre-coded questions, as was indeed the case in another study.21 It is also possible that participants have taken for granted those risk factors.
Limited knowledge about overdose preventionA large proportion of participants cited consuming adulterated or cut heroin as a risk factor for overdose, even though this is considered an erroneous belief by the scientific community, as cited elsewhere.21 It is possible that this myth is encouraged by the fact that prevention messages associated with concerns about purity or amount coincide with those regarding adulterated heroin. Using a large amount of drug as a risk factor for suffering an opioid overdose was the most frequently cited reason, as in other studies.12,21
Other authors21 reported a prevalence of 57.2% regarding limited knowledge of overdose risk factors (less than two risk factors), against our 81.9% prevalence for the same variable. This difference could lie in the fact that our study population is older and less educated than that making up the Itinere cohort.3,21
The role of treatment and preventive trainingTo be effective and to have a positive impact in knowledge, overdose prevention programs must achieve high coverage, reaching most of the IDUs population.24 In Spain, harm reduction programs were implemented during the 1990s, especially methadone maintenance treatment and syringe exchange programs. These were set up later than in other EU countries, and introduction was heterogeneous throughout the country.25–28 Although overdose prevention interventions had been working in Barcelona for over 8 years at the time of the interviews,25–27 these interventions have only recently been implemented in a systematic way.
In this study, only 27% of the participants reported ever having attended overdose prevention courses. Even though they presented lower prevalence of limited knowledge than their peers, this difference was not statistically significant, and neither was the association measure (adjusted prevalence ratio). Other studies21,29,30 have reported better scores regarding overdose prevention knowledge in those IDUs attending courses or IDU-oriented resources. We would expect finding an association between knowledge about overdose prevention and access to health care services, but in our sample, use of harm reduction resources (supervised injecting facilities and overdose prevention courses) does not seem to protect against limited knowledge. However, Harm Reduction strategies have played an important role in other aspects of community health. Hence, injected drug use has overall decreased in Spain while syringe exchange programs have been expanded.25
Interestingly, participants who had never been exposed to treatment for their drug use did present significantly higher prevalence of limited knowledge about overdose prevention. Other studies had reported that exposure to opioid maintenance treatment reduced long-term risk of overdose death.31,32 In our study, participants who had undergone previous treatment were less prone to presenting limited knowledge. If knowledge levels translate into adequate preventive behaviors, it is possible that, until the study period, treatment centers were more efficient at delivering correct information, and therefore at preventing overdose episodes, than were overdose prevention courses. Further studies are needed to evaluate the performance of more recently implemented, systematic overdose prevention programs. Additionally, efforts should continue to make the most of those opportunities presented in each treatment episode, further spreading preventive messages in the community.
Other Risk factors for Limited Knowledge about overdose preventionOther individual factors associated with limited knowledge about overdose prevention in this study were the country of origin (Eastern European countries), having a low educational level, and never having experienced an overdose before. IDUs who have already suffered non-fatal overdose episodes are more likely to be experienced drug users, with a history of exposure to different IDU-oriented resources including treatment and harm reduction, and probably having received a broad array of preventive messages.
Country of origin and low educational level likely have contributed a negative effect on understanding complex messages, such as those supplied in overdose prevention courses, since initially the content of such courses was neither provided in other languages nor tailored to low literacy populations. In this sense, special efforts should be made to provide specific responses to IDUs with limited Spanish/Catalan knowledge and low literacy. In the Catalonian case, where there are higher proportions both of IDUs and of immigrant drug users than in other Spanish regions, ad hoc programs should be developed accounting for users’ specificities, such as idiomatic barriers and/or functional illiteracy stemming from a low educational level. Moreover, as the proportion of foreign-born users in IDU-oriented resources increases, and since immigrants in Spain tend to make less use of health services than natives,33,34 specifically targeted interventions should be developed to assure an increased access to such resources.
In conclusion, our findings suggest that harm reduction and overdose prevention programs, though implemented for almost a decade,25–28 and though successful in many other aspects, might not have had a significant impact in reducing limited knowledge about overdose prevention among injecting opioid users in Catalonia at the time of the interviews. It is of vital importance to continue developing extensive, methodologically systematic overdose prevention programs, especially designed to address idiomatic, educational and cultural differences, in order to improve knowledge about overdose prevention and to reduce potentially harmful beliefs persisting in the community. All IDU-oriented resources should be included in such programs, particularly treatment centers and harm reduction resources, in order to maximize their effect. Qualitative research should be undertaken to better understand the barriers to acquiring knowledge and how this translates into actions at overdose events among the injecting population. This research should then inform the development of future overdose training programs and their evaluation.
Opioid overdose events are preventable and reversible, but still account for over 6500 deaths per year in Europe. Self-perceived general reasons for overdose and actions to undertake if witnessing an overdose have been explored, and can inform about the general “state of the art” regarding preventive knowledge in injecting drug users (IDUs).
What this study adds to what is known?A restrictive variable is used which addresses limited knowledge about opioid overdose prevention, hence concentrating on the most vulnerable IDUs population.
Within the EU, Schengen Treaty allows free migration across borders. The present study acknowledges the country of origin of participating IDUs. Achieving larger impact of preventive measures may imply addressing this immigration status.
Ma Felicitas Domínguez-Berjón.
Contributions of authorshipAuthors Maria Teresa Brugal, Jordi Casabona, Cinta Folch, Xavier Majó and Carmen Vecino designed the study and wrote the protocol. Authors Albert Espelt and Ana Sarasa-Renedo conducted literature searches. Authors Albert Espelt, Ana Sarasa-Renedo and Yolanda Castellano conducted the statistical analysis. Author Ana Sarasa-Renedo wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
FundingThis study was supported by the following entities: Direcció General de Salut Pública, Departament de Salut, Generalitat de Catalunya; Subdirecció General de Drogodependències, Departament de Salut, Generalitat de Catalunya; Agència de Gestió d’Ajuts Universitaris I de Recerca – AGAUR (2005/SGR/00505), Departament d’Universitats, Recerca i Societat de la Informació, Generalitat de Catalunya; and Red de Trastornos Adictivos [RD06/0001/1018].
Conflict of interestThe authors declare that there are no conflicts of interest.
The authors thank all interviewers, participants and collaborating centers: Ambit Prevenció; SAPS; Baluard, CAS Vall d’Hebrón; “El Local” Sant Adrià; AEC-Gris;Asaupa’m Santa Coloma; CAS Reus, AIDE Terrassa, Alba Terrassa, Arrels Lleida; Mercè Fontanilles Lleida; Creu Roja Constantí, IAS Girona.