Edited by: Carme Borell
Last update: March 2023
More infoThe COVID-19 pandemic currently affects populations worldwide. Although everyone is susceptible to the virus, there are numerous accounts of the pandemic having a greater impact on lower socioeconomic groups and minorities, which is a ubiquitous phenomenon. It is essential for public health administrations and governments to uncover and understanding these inequities to develop proper intersectoral policies to tackle this crisis. Therefore, developing a conceptual framework on this topic, describing the social mechanisms that explain the unjust distribution of the incidence and mortality of COVID-19, is a key task. The aim of this paper is to adapt the framework on social determinants of health from the World Health Organization to the specifics of COVID-19 pandemic. Thus, it identifies and explains the structural and intermediate determinants involved in this pandemic, and adds some new elements (such as the role of the oppression systems and communication) which may help to understand, and ultimately tackle, social inequities in COVID-19 distribution.
La pandemia de COVID-19 afecta actualmente a poblaciones de todo el mundo. Aunque todas las personas son susceptibles de contraer la enfermedad, hay numerosos argumentos de que la pandemia tiene un mayor impacto en los grupos socioeconómicos más desfavorecidos y en las minorías, lo que es un fenómeno omnipresente. Es esencial que las Administraciones de salud pública y los gobiernos comprendan las desigualdades para desarrollar políticas intersectoriales adecuadas para hacer frente a esta crisis. Por lo tanto, es clave desarrollar un marco conceptual sobre este tema, que describa los mecanismos sociales que explican la injusta distribución de la incidencia y la mortalidad de la COVID-19. El objetivo de este trabajo es adaptar el marco sobre determinantes sociales de la salud de la Organización Mundial de la Salud a las particularidades de la pandemia de COVID-19, identificar y explicar los determinantes estructurales e intermedios implicados en esta pandemia, así como añadir algunos elementos nuevos (como el papel de los sistemas de opresión y la comunicación) que pueden ayudar a comprender, y en última instancia a abordar, las desigualdades sociales en la distribución de la COVID-19.
SARS-CoV-2, the new coronavirus, is a necessary but not sufficient cause of the COVID-19 pandemic. Starting as a health crisis, the pandemic was transformed into a social, economic and political phenomenon by the high risk of person-to-person infection, the collapse of health systems and the need for measures such as lockdowns.1 These factors occurred in a world where socioeconomic inequalities have risen sharply and have encouraged viral transmission due to precarious employment and living conditions.2,3 However, these factors are not equally distributed and consequently a pandemic in an increasingly unequal world has unequal and unjust consequences for health and its determinants.
Although everyone is susceptible to the virus, there are numerous accounts of the pandemic having a greater impact on lower socioeconomic groups and minorities, which is a ubiquitous phenomenon. A higher incidence and mortality of COVID-19 in disadvantaged and minority social groups has been reported in several countries.3
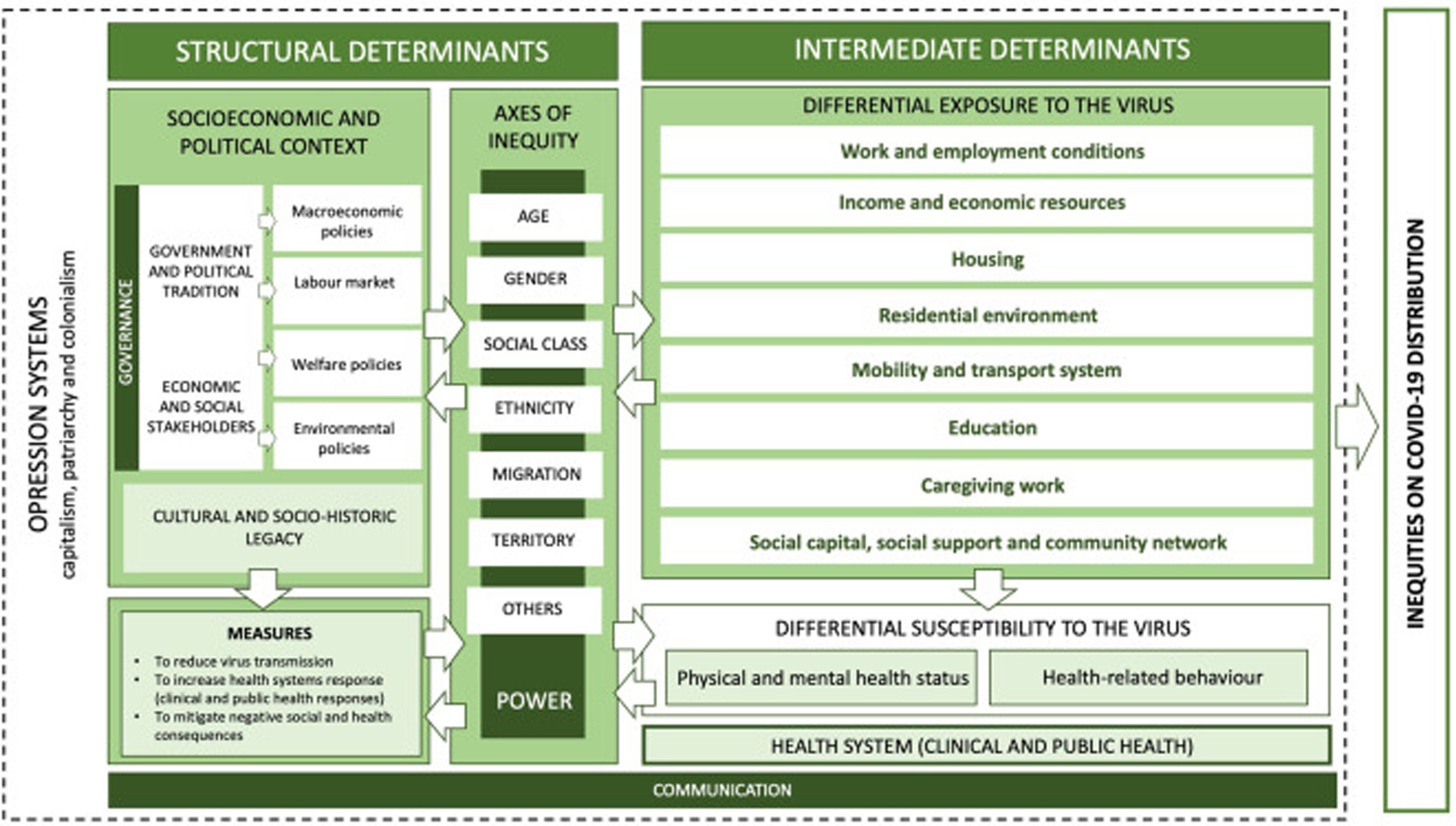
To tackle this crisis, it is essential for public health administrations and governments to uncover and understanding this social phenomenon. Therefore, developing epidemiologic theory on the unequal distribution of this pandemic is a key task. The aim of this article is to adapt the framework on social determinants of health from the World Health Organization to the specifics of COVID-19 pandemic, describing the social mechanisms that explain the unjust distribution of the incidence and mortality of COVID-19 (Fig. 1). In our knowledge, there are not frameworks that directly address this issue.
MethodWe reviewed the evidence published to date on inequities in the incidence and mortality of COVID-19 and their social determinants until December 2020. Then, we carried out an iterative process to organise and relate the available data into a conceptual framework, based on the general framework on social determinants of health of the World Health Organization and also that of the Spanish Commission to Reduce Socioeconomic Inequalities in Health.4,5 Thus, we have adapted these frameworks in order to include the specifics pathways to health inequities in this pandemic, adding new elements such as the role of the oppression systems and communication. The complete process and methods are detailed in the online Appendix 1.
A conceptual framework on unequal COVID-19 distributionGiven the available evidence, this proposed framework focuses mainly on middle- and high-income countries. Below we describe the main determinants included in this framework.
Oppression systemsPeople's health and wellbeing are shaped by the multiple aspects of social life, government and governance, economics and politics, and space and place, which enable or inhibit the implementation of policy and people's capacity to follow it.6 All of those aspects are influenced by hegemonic structures, which rely on a set of values and ideologies that are reinforced by power structures (as political, corporations, etc.) and become perceived as natural and inevitable.7 Historically, this hegemony has been reflected in systems of oppression and exploitation, such as capitalism, colonialism/racism and patriarchy, which lead to social exclusion and interact to influence all levels of the social determination of health, including the COVID-19 crisis.8
Despite these oppression systems are not explicitly named in known previous conceptual frameworks on health inequities, such as those which we are based on, it is important to emphasize their relevance to understand phenomena such as this pandemic, and the inequities related to it. For instance, some authors report that the underlying reason for this pandemic (and its inequities) must be found in global capitalism and how it fosters the global alteration of ecosystems, along with social class inequalities, which lead to insecure and unsafe living conditions for most of the global population.9 Regarding patriarchy, COVID-19 has demonstrated the functioning of existing gender systems, which reproduce gender inequalities and reverberate in all aspects of society. Colonialism has been expressed in many areas of the pandemic (from the incidence of the disease to access to vaccines, for example), so that the political economy of COVID-19 has been the political economy of extraction, following longstanding patterns of exploitation dating from colonial times.10
Structural determinantsThe aforementioned systems of oppression deeply influence the structural determinants of COVID-19 distribution, which include the socioeconomic and political context. This level is related to both the type of government and political tradition and the economic and social powers/lobbies which, in turn, determine the governance processes and, consequently, the public policies (such as macroeconomic, labour market, welfare and environmental policies) that encompass the rights contained in the legislation and in the practices through which these rights are exercised. This dimension, which also includes cultural and socio-historical legacy (i.e. values such as democratic culture, individualism/collectivism, trust in institutions, inclusion of minorities and respect for diversity, rules and ways of life), clearly influence the kind of response and measures to reduce transmission of the virus, to increase the response of the health systems and to mitigate the negative health and social consequences of COVID-19 through social protection policies.1,3 For instance, political orientation might be reflected in an emphasis on intervention on individual-level behaviour versus population-level measures. Similarly, governments with a market-driven orientation may prioritise interventions that preserve the economy.9 Therefore, policy responses to this crisis may protect people from the entire social spectrum or, conversely, increase social and health inequities.
In addition, the socioeconomic and political context creates a social hierarchy due to unequal distribution of power and resources among social groups, according to several axes of inequity such as age, gender, social class, ethnicity/migration, territory, sexual and affective diversities, ability, and other factors. Indeed, these axes of inequities lead people to occupy social positions that imply different power relations and access to resources and exposure to discrimination.4 Moreover, intersectionality theory is also necessary to understand these experiences (e.g., what is happening with the effects and consequences of COVID-19 on low-income racialised women). This leads to a differential exposure risk and a differential susceptibility to the virus due to distinct work and living conditions.2,4,5 This has been clearly reflected in the tremendous impact of COVID-19 on older people, mainly in nursing homes, not just due to biological ageing-related factors, but also to their lesser access to resources and opportunities compared with people from labour force ages.
Intermediate determinantsIntermediate social determinants, between structural determinants and COVID-19 inequities, are related to the working and living conditions that lead to a differential exposure to the virus. Also, they influence health-related behaviours and health status (i.e.. comorbidities, biological embodiment of social reality, stress response, etc.), which lead to a differential susceptibility to the virus. Finally, they are related to the ability of the health system (clinical and public health), which may addresses differences in exposure and vulnerability by improving equitable access to health care and public health services.2–4
1) Differential exposure to COVID-19According to the social determinants and health inequities theory, social stratification engenders differences in exposure to health-damaging or health-protective social determinants, leading to an unequal distribution of health outcomes, such as COVID-19 incidence and mortality.4,5 These determinants include several dimensions, although they probably have a different weight in the production of COVID-19 inequities and have slightly changed during the course of the pandemic and between the different waves. For example, occupation played a strong role in the first few weeks of the pandemic, whilst housing probably became more important in subsequent phases.2,3 However, in general, the more underprivileged population seems to be more exposed to COVID-19. The social determinants related to the differential exposure to COVID-19 are described in Table 1 (all identified references by topic are included in online Appendix 2).
Intermediary determinants related with differential exposure and their relationship with COVID-19a.
| Work and employment conditions: Face-to-face jobs, without teleworking, pose a greater risk of exposure to infection. These include essential workers, such as those from the food and transportation sectors and cleaning staff, whose jobs usually entail physical proximity to other people, and healthcare workers who experience close contact with persons with potential COVID-19 infection. In addition, precariousness (e.g. temporary workers) and informal employment, such as seasonal migrant agricultural workers, may increase exposure to infection due to the lack of adequate personal protective equipment at the workplace; even more importantly these workers have limited access to sick leave and health services and may also be hesitant to quarantine when they are infected. |
| Income and economic resources: Low income and lack of economic resources is another dimension that could increase COVID-19 exposure and reduce adherence to quarantine. This social determinant is closely linked to adverse employment and housing conditions, two of the most important pathways to unequal distribution of the pandemic. However, beyond these clear pathways, low income fosters a lack of basic amenities as adequate personal protective equipment, such as masks and alcohol-based gel, increasing the risk of COVID-19 infection. In addition, low income is related to other types of insecurity, such as food insecurity, which may lead to seeking help in crowded places where there is a higher likelihood of infection. |
| Housing: Poor housing conditions, energy poverty, housing insecurity and homelessness increase the risk of infection and mainly affect the most disadvantaged social groups. Crowded living conditions and mutigenerational households may increase the risk of infection with SARS-CoV-2. In addition, eviction and homelessness are likely to increase COVID-19 infection rates because of the aforementioned reasons and because they also result in doubling up, transiency, limited access to healthcare, and a decreased ability to comply with pandemic mitigation strategies. Indeed, physical distance and social isolation are important public health measures to tackle the spread of the pandemic, which strongly depends on people having access to safe and secure housing. Finally, collective housing, such as shelters and long-term care facilities (e.g. nursing homes for the elderly), without adequate public health measures, may increase infection risk in residents and workers, as demonstrated during the current pandemic. |
| Residential environment: Exposure to COVID-19 differs depending on the area of residence, urban or rural, as well as within urban areas, fact that could be explained by constitutional factors (i.e. the characteristics of the residents in those areas) and contextual factors (i.e. the characteristics of the place such as its population density), although these two types of factors are closely intertwined. Areas with a higher proportion of people with lower socioeconomic status or ethnic minorities have higher rates of COVID-19, as do those with a lack of resources in key sectors such as transportation, employment, health care capacity, public health infrastructure, food security and green spaces. |
| Mobility and transport system: The global spread of the virus has been increased by hypermobility of the transport network. Locally, public transport is used daily by millions of people, often carrying passengers above its capacity in peak hours, which might increase exposure to COVID-19 among public transport users. However, this imply the need to improve public transport in terms of user safety and to promote active mobility such as walking and cycling which, in turn, are more compatible with physical distancing. |
| Education: The pandemic has revealed that the digital divide involves significant inequities, conferring a higher risk of infection in the most vulnerable populations. The lack of access to information relevant to protection, the impossibility of managing certain procedures (including those related to health services), the impossibility of teleworking, and a greater potential for social isolation. Likewise, it is worth noting the situation of children and adolescents who were unable to access education through digital tools during lockdowns. Indeed, school education is a powerful strategy to combat poverty and to promote social interaction and safety, important social determinants of health. This is important because school closures have been implemented internationally to control the pandemic, although there is no clear evidence of the effectiveness of this measure. |
| Caregiving work: Caregiving work, both formal and informal (e.g. domestic work and family caregivers, paid caregivers for dependent people, nursing home workers, etc.) may expose caregivers to infected people, leading them, in turn, to become potential spreaders of COVID-1. Furthermore, caregiving work is significantly gendered, with women generally undertaking most care-related responsibilities, introducing an additional gender-bias exposure to the risk of infection. |
| Social capital, social support, and community network: Social capital and community support networks may reduce the risk of exposure to COVID-19. Outbreaks such as COVID-19 are better managed in places where social capital is high. For instance, greater trust and relationships within a community could endow individuals with a greater concern for others, thereby leading to more hygienic practices and physical distancing, and support with material and psychosocial resources to the most disadvantaged people. In addition, there is well-known the positive effects of bonding social capital among close relations or tight-knit communities in reducing health inequities such as those being reported in the COVID-19 pandemic. Finally, social and community participation has been described as one of the factors that can influence the future of the pandemic, both because of its contribution to knowledge, essential for planning and intervention, and because of the co-production of responses to the pandemic. |
In addition to all the determinants of exposure to COVID-19, differences in the distribution of the pandemic are also related to differential individual susceptibility to the virus. Growing evidence reports that the risk of COVID-19 infection and severe illness is increased by underlying chronic diseases and behaviours that may negatively affect health,11 which, in turn, are unequally distributed across the social hierarchy.4 Thus, disadvantaged groups become more susceptible to the virus, widening health inequalities.
3) Health systems (clinical and public health)Health systems themselves (including both clinical health care and public health) should be viewed as an intermediary determinant because they can directly address differences in exposure and susceptibility to COVID-19, but also in epidemiological surveillance and, accordingly, the promotion of intersectoral action to implement preventive public health measures to tackle the pandemic and improve the population's health.12
CommunicationEffective communication of risk and community engagement are vital to reduce uncertainty and to properly deploy public health measures.13 However, the communication and dissemination of messages on disease prevention and containment measures may not reach the entire population uniformly, and may be understood and interpreted differently. This is associated with social inequalities, which also exist in access and barriers to health knowledge among groups according to educational level, social class, origin and ethnicity, and age.14 Moreover, because of health knowledge inequity, COVID-19-related misinformation and rumours are relatively prevalent among people with low health literacy, although they also depend on political ideology and perceptions.8 Moreover, across and within countries, members of certain groups —such as older people, less educated people, and those with a lower income— have limited access to digital technologies and poor internet skills. Digital inequalities result in some people being more socially excluded than others when required to maintain physical distancing because of their limited access to the digital society.15
ConclusionsThis conceptual framework offers a model to understand the relationship between social determinants of health and the unequal distribution of the incidence of COVID-19 and its associated mortality. Although the elements that compose the framework are shown as a group of closed boxes, it is important to note that they are parts of a complex system and, in turn, can themselves also be understood as systems, incorporating other elements from a lower hierarchical level. Thus, dimensions such as housing, employment, residential environment, and income are closely interrelated (and embedded in certain structural determinants and systems of oppression) in explaining the mechanisms that generate inequalities in COVID-19 distribution. Finally, it is important to note that this phenomenon also interplays with another diseases (mainly chronic diseases), and their determinants, that increases the complexity that we are discussing about. This convergence is known as a syndemic, or synergistic epidemic. It has been defined as “a set of closely intertwined and mutual enhancing health problems that significantly affect the overall health status of a population within the context of a perpetuating configuration of noxious social conditions‿.3 Thus, considering COVID-19 only as an isolated phenomenon excludes such a broader but necessary perspective.
Although this conceptual framework is proposed for this specific crisis, its utility may be extrapolated to other similar epidemics. Identifying these mechanisms and representing them in a framework could be useful to design, deploy and assess public policies to address inequities in COVID-19. Developing public policies and specific interventions that address intermediary determinants such as work and employment conditions, income, caregiving, housing, the transport system, social capital and community networks could have a strong impact in reducing the incidence and mortality of COVID-19 and their inequities, and could prevent further effects of health and social inequities. Indeed, based on this framework, a review, of the intersectoral public policies that have been implemented to address the pandemic would be desirable.
Finally, further efforts to develop conceptual frameworks for the socioeconomic and health consequences of the COVID-19 pandemic are needed. That topic is beyond the scope of this article, although there is some evidence that already shows that those consequences are having a differential impact by axes of inequality and therefore on health inequities. Future studies will need to monitor these aspects and policies should address them.
Availability of databases and material for replicatingThis article is based on a review of the existing literature. The search strategy used for the review is available in online Appendix 1.
Editor in chargeMiguel ÿngel Negrín Hernández.
Authorship contributionsAll authors have designed the protocol to adapt the framework. B. Biaani León-Gómez have proposed the first scheme of contents. H. Vásquez-Vera and C. Borrell have made the literature review. Specific topics were distributed and reviewed by all authors: H. Vásquez-Vera, housing, differential exposure, and health related behaviours; B. Biaani León-Gómez, inequalities in COVID-19 and consequences; C. Borrell, governance, public health measures to reduce negative consequences and to increase capacity of the public health system; C. Jacques-Aviñó, power systems and inequality axes; M.J. López, education; L. Medina-Perucha, care work; M. Pasarin, social and community networks; E. Sánchez-Ledesma, education and employment and work; and K. Pérez, environment and transport systems. H. Vásquez-Vera wrote the first draft of the manuscript with inputs of other authors (related with several parts of the framework). All authors have made critical comments on the different drafts of the article and have approved the final version. All parts of the article have been critically reviewed and discussed by all authors.
FundingNone.
Conflicts of interestNone.
The authors thank the comments received to a previous draft of Lucía Artazcoz, Laia Palència, Glòria Pérez, and Maica Rodríguez-Sanz.