The planning, provision and monitoring of medical and support services for patient groups with chronic ailments may require disability assessment and registration. The purpose of this study was to assess disability in three groups of patients with chronic obstructive pulmonary disease (COPD), chronic heart failure (CHF) or stroke.
MethodsConvenience samples of consecutive patients diagnosed with COPD (102), CHF (99), and stroke (99) were taken from 1,053 primary care users in the southern area of the autonomous region of Madrid. The patients were informed of the study and were assessed in their homes by trained field workers using the World Health Organization Disability Assessment Schedule II (WHO-DAS II).
ResultsNone of the groups had patients with extreme disability on their global WHO-DAS II scores. The prevalence of severe disability differed among the groups and was highest for stroke and CHF (33.33% and 29.29%, respectively) and lowest for COPD (14.71%). The three groups shared two similar traits, namely, a higher prevalence of disability among women than men, and a specific pattern by domain, with the highest prevalence of severe/extreme limitations being found in household life activities and mobility. Severe restrictions in Social Participation were more frequent in patients with stroke and CHF. The group with moderate disability according to the global WHODAS II score (n=94) showed a high prevalence of severe limitations in mobility, life activities and self-care.
ConclusionsDisability among non-institutionalized persons with COPD, CHF and stroke is frequent and shows gender- and domain-related patterns similar to those described in a population-based study performed using the WHO-DAS II in elderly persons in Spain. ICF-validated disability categories could be useful in epidemiological surveys, individual assessments and primary care data monitoring systems.
La planificación, prestación y monitorización de servicios sociales y sanitarios a pacientes con trastornos crónicos puede requerir evaluación y registro de su discapacidad. El objetivo de este estudio fue evaluar la discapacidad de tres grupos de pacientes con enfermedad pulmonar obstructiva crónica (EPOC), insuficiencia cardiaca congestiva (ICC) o ictus.
MétodosPacientes con EPOC (102), ICC (99) e ictus (99), vistos consecutivamente, identificados de una lista de 1053 usuarios de atención primaria en el sur de la Comunidad Autónoma de Madrid, España. Tras ser informados, fueron evaluados en sus casas por entrevistadores entrenados utilizando WHODAS-2.
ResultadosNo hubo casos de discapacidad extrema, pero las tres poblaciones mostraron prevalencias de discapacidad grave según WHODAS-2 total, más altas en ictus e ICC (33,33% y 29,29%, respectivamente) y menores en EPOC (14,71%). Los grupos compartían un patrón de discapacidad más alta en mujeres y otro específico por dominios, con prevalencias más altas de discapacidad grave/extrema en actividades domésticas y movilidad. La participación social estaba más restringida en ictus e ICC. El grupo con discapacidad moderada en WHODAS-2 global (94 enfermos) mostraba prevalencias altas de discapacidad grave en movilidad, actividades diarias domésticas y autocuidado.
ConclusionesLa discapacidad en personas no institucionalizadas con EPOC, ICC e ictus es frecuente, con patrones por sexo y dominio similares a los descritos en España con WHODAS-2 en un estudio poblacional de personas de edad avanzada. Las categorías CIF de discapacidad podrían utilizarse en encuestas epidemiológicas y evaluaciones individuales, así como en sistemas de información orientados a la monitorización de la discapacidad en atención primaria.
Chronic diseases are regarded as long-term illnesses that will never be altogether healed. Predominant among the most important chronic conditions are mental illness, musculoskeletal or degenerative neurological disease and cardiovascular disease. In general, affected patients request a wide array of healthcare and social resources, requiring special coordination at the primary care level. Some conditions, such as dementia, may essentially demand social rather than medical or nursing services. Others, such as hypertension or diabetes, mainly call for medical services. Healthcare planning and coordination of the provision of both health and social services is particularly essential when disability-related medical (e.g., rehabilitation) and social services are needed. Chronic heart failure (CHF), stroke and chronic obstructive pulmonary disease (COPD) constitute diagnostic groups requiring both types of resources –social and health– as dictated by individual patient profiles. Whereas the use of primary care services by such groups has frequently been described, little is known about their disability patterns. Recent research results emphasize the actions of interdisciplinary teams and information and communication technologies (ICTs), with special attention paid to fostering patient mobility at home and encouraging caregivers to undertake informal rehabilitation to achieve this goal1,2. Furthermore, there is growing use of ICTs to support chronic home care by means of telemedicine3,4 and ambient assisted living applications5. Coding is basic for exploiting the capabilities of ICT6.
The biopsychosocial model and classification system developed by the World Health Organization (WHO), i.e., the International Classification of Functioning, Disability and Health (ICF) model, suggest that disability is a general construct not confined to disease-specific factors. The ICF incorporates a comprehensive account of personal, social and environmental factors and thus opens new avenues of research for the study of disability and its determinants. Few population-based studies on disability assessment in specific chronic conditions have been conducted using methods linked to the WHO-ICF model. A search of the literature in Medline, using search terms such as “disability”, “survey” and “primary care”, diagnoses such as “stroke”, “COPD” and “CHF” and selection criteria applied to abstracts, yielded six reports7–12. The instruments used for disability assessment varied. The WHO Disability Assessment Schedule II (WHO-DAS II) was used in the Measuring Health and Disability in Europe (MHADIE) project, two stroke studies –one Slovenian and the other German– and an Iranian study in the elderly population7–9. The well-known Katz and Lawton scales were used in a Finnish study on stroke among the population aged 65 to 74 years old10. Distinct questionnaires were used to measure severe COPD-related disability in Spain7. The WHO-DAS II and the ICF Checklist were used to study the prevalence of disability in Spanish populations12,13.
The 2006 Promotion of Personal Autonomy and Care of Dependent Persons Act (Ley 39/2006, de 14 de diciembre, de promoción de la autonomía personal y atención a las personas en situación de dependencia) lent impetus to the use of an ICF-based approach in the 2008 Disabilities, Autonomy and Health Status Survey14,15.
This study sought to assess disability in three groups of Spanish primary care patients with stroke, CHF or COPD by using ICF-based methods to describe differences in disability patterns for the purpose of ICT-based service provision.
MethodsStudy population, healthcare services and entities targeted for studyThe population generating the patients under study was geographically defined as that residing in former Health District XI of the Autonomous Region of Madrid (Spain). This population was entirely urban, with the majority consisting of persons who had migrated from other Spanish regions from 1960 to 197016. In practice, 98% of this population was entitled to receive primary and hospital care free of charge, provided by the Spanish public health services via the Madrid Institute of Health (Servicio Madrileño de Salud). The study population were older and had lower financial and educational levels than the general population in Madrid.
In December 2007, healthcare in Health District XI was provided to 887,134 individual holders of health insurance cards by 42 primary care teams, comprising 521 general practitioners, 111 pediatricians and 490 registered nurses. Acute hospital care was provided by only three general hospitals, namely, the major-sized 12 de Octubre Hospital and two smaller institutions. Individuals are required to be registered with a general practitioner, who then becomes their compulsory supplier of health services. General practitioners act as the gateway to healthcare for the population aged over 14 years and referrals to specialists. The unified primary care electronic medical record is the main source of information on all diagnoses and health resources used by the patient. As with other urban populations in Spain, patients with CHF, stroke, or COPD are generally referred to hospitals or specialists by their general practitioners. This study was conducted in a population of 198,670 individuals over 14 years of age, receiving care in the former Health District XI from 129 family medicine specialists who, by way of inclusion criteria, fulfilled two quality requirements in the electronic medical record registry, namely: (i) notes were kept on >64% of the visits (75th percentile); and (ii) the mean number of care episodes per patient was >417. Stroke, CHF and COPD were selected from among 26 chronic conditions, due to the comparatively higher mean individual use of health resources among patients with these diseases.
PatientsA total of 300 patients with COPD, stroke or CHF were identified from computer files kept on 3,183, 2,658 and 1,377 primary care users, who were diagnosed with COPD, stroke or CHF, respectively, and were being managed by the above-mentioned 129 physicians in 2007. These numbers corresponded to prevalence figures of 21, 18 and 9 per 1,000 inhabitants, respectively. The numerators of these prevalence figures generated convenience samples, yielding approximately 100 participating patients after attrition by death or refusal. All participants had been officially resident in the district during the year preceding the first scheduled visit or longer.A letter was mailed to all patients by the research team, inviting them to participate in this study. The patients’ general practitioners were informed through an internal institutional procedure. A week after the invitation had been sent, an attempt was made to contact individual patients or their relatives by telephone in order to provide further information on the study and, if the patient agreed to participate, to make an appointment. Letters were sequentially mailed, with participants being selected until approximately 100 positive respondents had been enrolled, corresponding to the profile outlined in Table 1. The study included 99 volunteer patients with CHF, 99 with stroke and 102 with COPD, who were finally interviewed at home after informed consent had been obtained. These numbers corresponded to different sampled proportions: 3.20% for COPD, 3.72% for stroke and 7.19% for CHF.
Instrument for disability measurementWe used the 2nd edition of the WHO-DAS II, an instrument tested in over 14 countries and 16 languages, and shown to be a reliable and suitable tool with good metric properties in Spanish clinical and rehabilitation samples of chronic patients18. The 36-item WHO-DAS II is a self-reported or interviewer-administered scale covering the following six disability domains assessed over the 30-day period preceding administration: understanding and communication (UAC), getting around (GAR), self care (SCA), getting along with people (GAP), life activities (LAC), and participation in society (PSO). Items are answered on a 5-point Likert-type scale (1: none; 5: extreme), which grades the difficulty experienced by the participant in performing a given activity. Summary-index and domain scores range from 0 to 100. We used the correct standards released by the WHO through its partner school in Spain, the Psychiatry Research Unit at the Marques de Valdecilla Hospital in Santander19. WHO-DAS II item content is summarily described in this issue of Gaceta Sanitaria20 and in Appendix I (on-line) as a version of the instrument for proxy informants.The WHO-DAS II was chosen in preference to traditional instruments for several reasons. Firstly, the WHO-DAS II is an ICF-based instrument that is not only intended for epidemiological studies but, as stated above, has also proved useful in distinct clinical settings. Secondly, this instrument can be self-administered and used by experts or informal caregivers alike. Thirdly, WHO-DAS II measurements can be completed by ICF assessments of contextual, physical and social environmental factors that have an impact on disability in addition to the effect of health conditions. Fourthly, some authors have commented on more subtle details: while the Extended Katz and Lawton scales take instrumental activities of daily living measures, such as those linked to domestic life, into account, these scales pay no attention to the various facets of disability that are known to be highly predictive of self-rated health and need for services, i.e., the ability to communicate with others and maintain an active social life21.
Field workIn this study, written informed consent was given by all participants in accordance with the Helsinki Declaration. Participants were visited at home from April to September 2009, where their disability was evaluated by professional interviewers purpose-trained in all the assessment procedures used in this study.
A total of 1,053 letters were sent to the homes of patients in the sample, explaining the study in general, and the objective of the visit in particular. Likewise, their physicians were simultaneously informed about the study by surface mail. Trained researchers from the Carlos III Telemedicine and e-Health Institute, working in collaboration with the Madrid Regional Primary Care Authority for District XI, contacted patients or their relatives by telephone to inform them of details of the current study and obtain verbal acceptance prior to written informed consent. Seventy-five of the letters mailed were returned to the sender, stamped “address unknown”. Of the total number of persons telephoned, 260 failed to answer the call, 41 had died, 349 refused to collaborate, and 328 agreed to participate. Finally, 26 patients were not located at the date of the visit and, of the 302 patients who did receive visits from field workers, two refused to sign the consent form and 300 were assessed. Differences between positive and negative respondents were less than 5% by sex and were statistically non-significant by age group and comorbidity, i.e., the number of diagnoses.
Home visits were made approximately one week after dispatch of the letter and were conducted satisfactorily, despite frequent extensions due to patients or relatives needing or requesting support. A team of three interviewers, consisting of two social workers and one university graduate in social sciences, trained by disability assessment experts in using the WHO-DAS II, assessed disability at the patients’ homes using a structured questionnaire adapted to the Spanish version of the 36-item WHO-DAS II and a set of items designed to examine patients’ ability to use interactive telecommunication devices at home. Diagnostic profiles were drawn from general practitioners’ records.
The study sample was an aged, lower-middle or working-class population, with significant inequalities in terms of socioeconomic profiles: 54.3% male, 45.7% female, mean age 74.4 years. The majority belonged to working- or lower-middle class families; those needing help and not living alone were assisted by their relatives, usually daughters. Professional help was scarce: in general, subjects had home help for 1 hour on 2 days a week. Most of the individuals included in the study sample were residents of Health District XI. Most of the households were 3- to 4-room apartments in 4- to 5-storey buildings without an elevator. The patients spent long periods of time without leaving home, engaged in very few outdoor activities, most of which involved visits to the primary care health center, and were almost always assisted by a relative. Persons with severe disabilities used special transport (ambulance). Ten percent of answers were provided by relatives/caregivers and 90% by patients. In several cases (15%), the survey was conducted with support from family members, due to the patients’ difficulties in providing answers or giving consent.
Data-analysisA WHO-DAS II score database was compiled. Items addressing work status were differentially treated, as stipulated by the Promotion of Personal Autonomy and Care of Dependent Persons Act14, since most individuals in our sample were not gainfully employed. The sexuality item was also excluded from the analysis, due to an unusually high proportion of missing values. The life activities domain was assessed in terms of work only among participants who still performed such activities. Missing data for items with less than 30% of missing values were replaced by the mean of the remaining domain values, in line with reported methods13,14. Any individual leaving more than one WHO-DAS II domain blank was excluded from the analysis.
The prevalence of disability was calculated as a percentage. For analytical purposes, disability for specific domains or in different diagnostic groups was assessed and dichotomized as present (if severe or complete), or as absent (if none, mild or moderate) in terms of the ICF categories. Prevalence odds ratios (OR) were reported as crude or as obtained from unconditional logistic regression. The study was approved by the 12 de Octubre Hospital ad hoc Research Ethics Committee, as indicated in report number 09/42.
ResultsSociodemographic features of the study sample as well as ICF disability levels are shown in Table 1. Diagnostic groups displayed varied personal and life characteristics, with the proportions of women, elderly individuls, widows/widowers and receivers of support from relatives or professional caregivers increasing from lowest in patients with COPD to highest in those with CHF. Extreme disability was absent in all three diagnostic groups. Seventy-seven patients, one-fourth of the pooled group, had ICF severe disability.
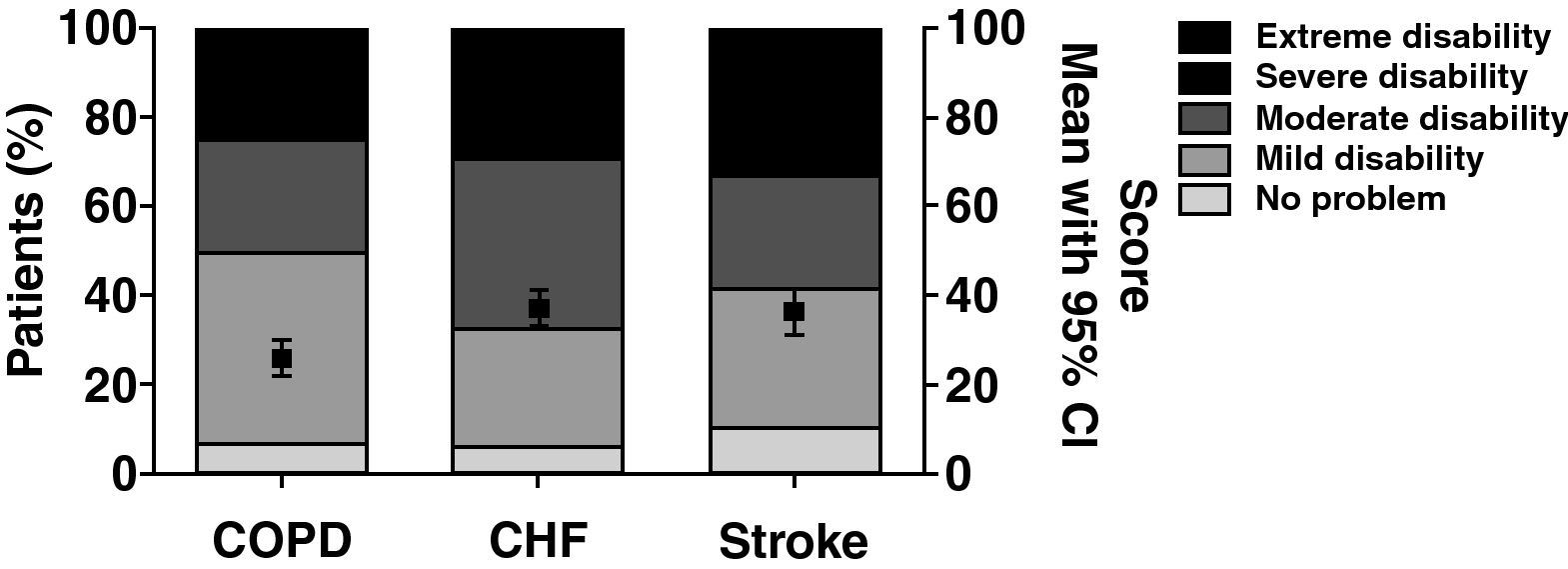
Group disability levels, including mean point estimates and 95%CI, are shown in figure 1. Disability levels were lowest in patients with COPD and highest in those with stroke, with a somewhat larger proportion of ICF moderate disability sufferers than that seen for the CHF group.
Mean and 95%CI values as well as prevalence of different International Classification of Functioning, Disability and Health (ICF) categories by World Health Organization Disability Assessment Schedule II (WHO-DAS) II global score in three diagnostic groups. COPD: chronic obstructive pulmonary disease; CHF: chronic heart failure.
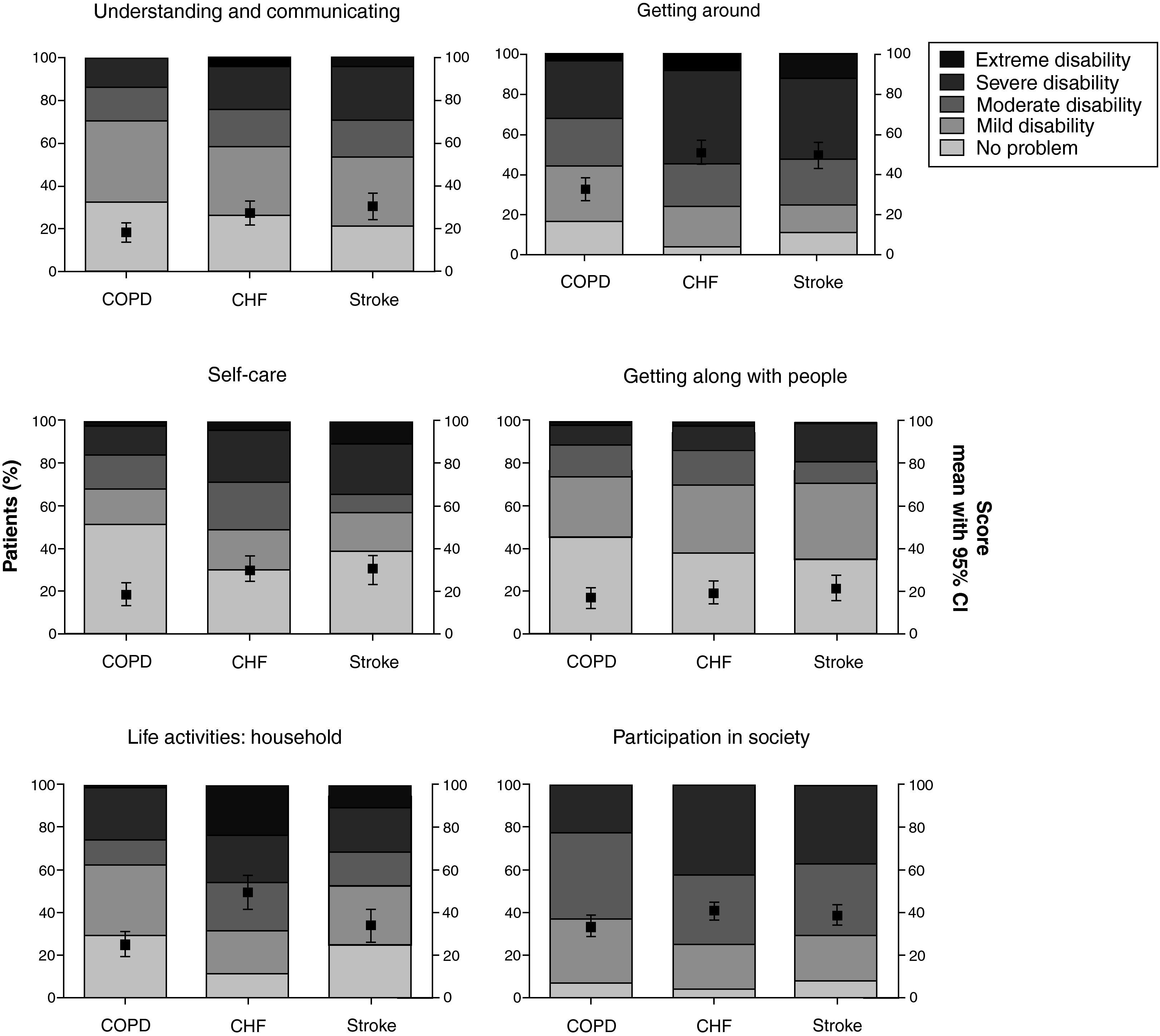
Disability patterns in ICF specific domains are depicted in figure 2. In contrast to total or general disability, ICF extreme disability was present in non-negligible percentages for life activities in CHF (24%), and stroke (11%), as well as for mobility and self-care in stroke and CHF. Participation in society and human relationships were the least affected domains in all three groups, in which the differences were small.
Mean and 95%CI values as well as prevalence of different International Classification of Functioning, Disability and Health (ICF) categories by World Health Organization Disability Assessment Schedule II (WHO-DAS II) score in different domains for each diagnostic group. COPD: chronic obstructive pulmonary disease; CHF: chronic heart failure.
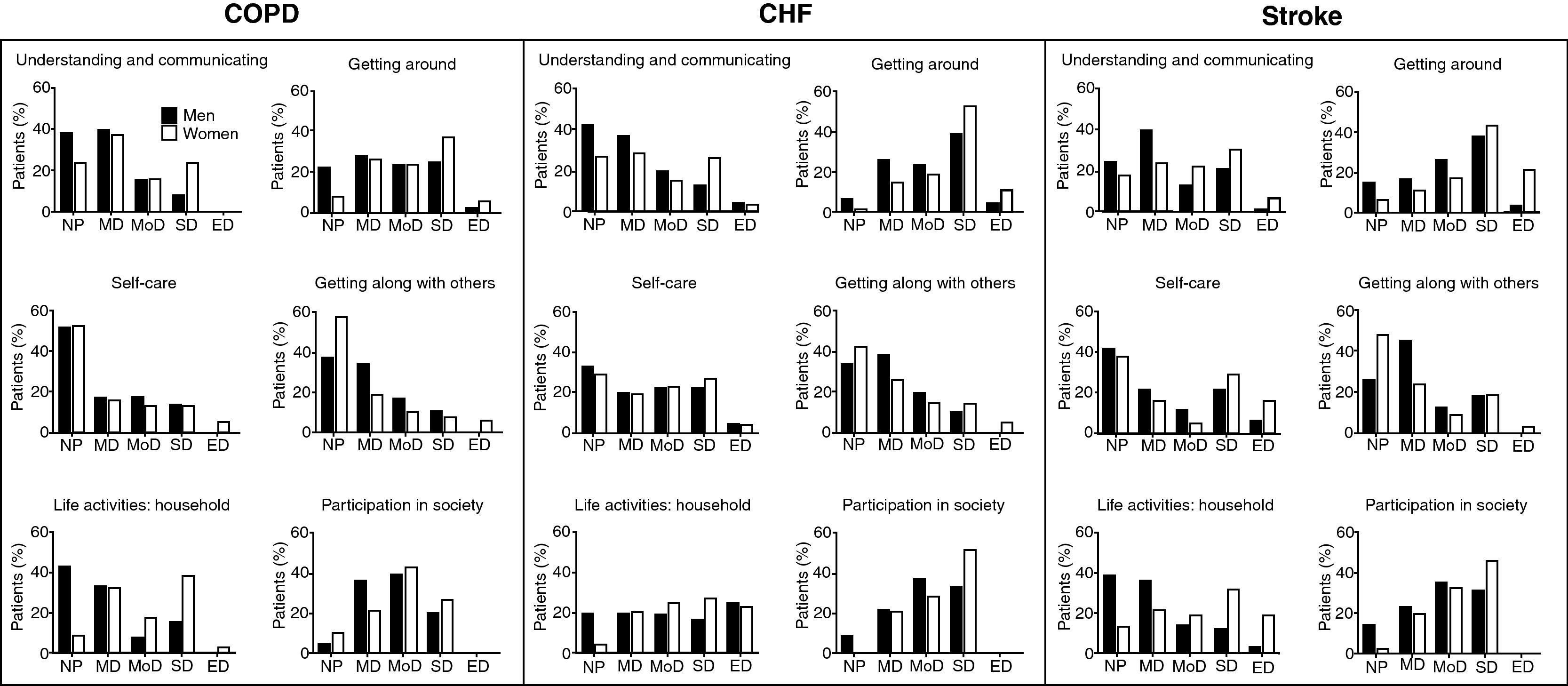
Sex-specific patterns for domains are shown in figure 3 for COPD, CHF and stroke. Higher prevalences of severe/extreme disability were in general observed in women, except in the human relationships and self-care domains, where differences in disability prevalences between genders appeared to be smaller. The highest prevalence of ICF severe/extreme disability was seen for mobility and social participation among persons with CHF and stroke.
Sex-specific prevalence of different International Classification of Functioning, Disability and Health (ICF) categories by World Health Organization Disability Assessment Schedule II (WHO-DAS II) score in different domains for each diagnostic group. COPD: chronic obstructive pulmonary disease; CHF: chronic heart failure.
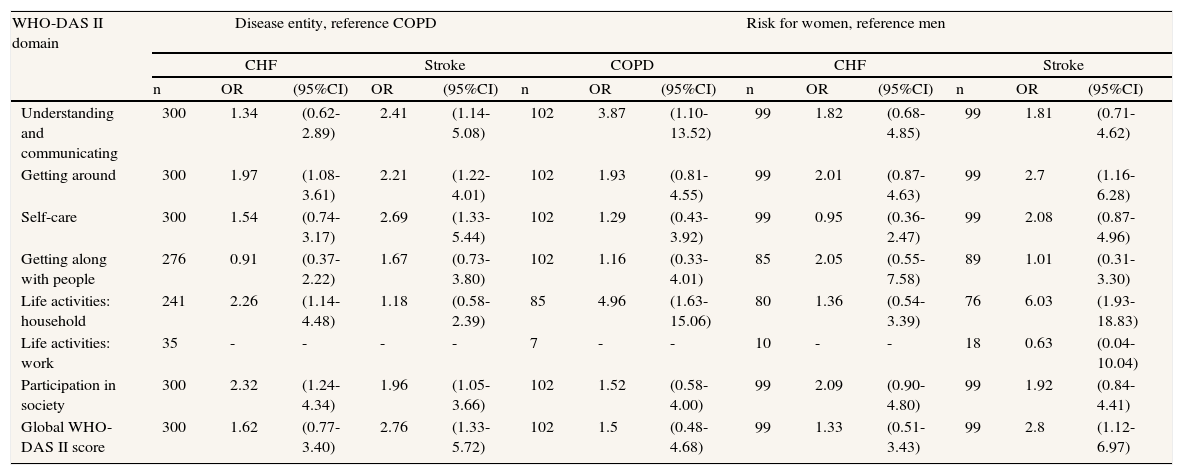
The results of comparing the prevalence of ICF severe/extreme disability for specific domains among groups and between the sexes, by using logistic models, are shown in Table 2. When compared with COPD, significant 2- to 3-fold OR differences were observed in five domains for stroke and a 2-fold variation was found in three domains for CHF, including activities and social participation. When differences by sex within groups were examined, the only significant difference for global scores was observed for stroke (OR=2.8; 95%CI: 1.12-6.97) in women. However, in the six-model groups, women had almost systematically higher disability than men, with the variation for life activities in COPD and stroke, and for communication in COPD, being particularly high, 5- to 6-fold, and statistically significant.
Comparative disability patterns by WHO-DAS II domain, sex and disease. Age- and, when appropriate, age- and sex-adjusted OR and 95%CI for ICF severe or complete disability.
| WHO-DAS II domain | Disease entity, reference COPD | Risk for women, reference men | ||||||||||||
| CHF | Stroke | COPD | CHF | Stroke | ||||||||||
| n | OR | (95%CI) | OR | (95%CI) | n | OR | (95%CI) | n | OR | (95%CI) | n | OR | (95%CI) | |
| Understanding and communicating | 300 | 1.34 | (0.62-2.89) | 2.41 | (1.14-5.08) | 102 | 3.87 | (1.10-13.52) | 99 | 1.82 | (0.68-4.85) | 99 | 1.81 | (0.71-4.62) |
| Getting around | 300 | 1.97 | (1.08-3.61) | 2.21 | (1.22-4.01) | 102 | 1.93 | (0.81-4.55) | 99 | 2.01 | (0.87-4.63) | 99 | 2.7 | (1.16-6.28) |
| Self-care | 300 | 1.54 | (0.74-3.17) | 2.69 | (1.33-5.44) | 102 | 1.29 | (0.43-3.92) | 99 | 0.95 | (0.36-2.47) | 99 | 2.08 | (0.87-4.96) |
| Getting along with people | 276 | 0.91 | (0.37-2.22) | 1.67 | (0.73-3.80) | 102 | 1.16 | (0.33-4.01) | 85 | 2.05 | (0.55-7.58) | 89 | 1.01 | (0.31-3.30) |
| Life activities: household | 241 | 2.26 | (1.14-4.48) | 1.18 | (0.58-2.39) | 85 | 4.96 | (1.63-15.06) | 80 | 1.36 | (0.54-3.39) | 76 | 6.03 | (1.93-18.83) |
| Life activities: work | 35 | - | - | - | - | 7 | - | - | 10 | - | - | 18 | 0.63 | (0.04-10.04) |
| Participation in society | 300 | 2.32 | (1.24-4.34) | 1.96 | (1.05-3.66) | 102 | 1.52 | (0.58-4.00) | 99 | 2.09 | (0.90-4.80) | 99 | 1.92 | (0.84-4.41) |
| Global WHO-DAS II score | 300 | 1.62 | (0.77-3.40) | 2.76 | (1.33-5.72) | 102 | 1.5 | (0.48-4.68) | 99 | 1.33 | (0.51-3.43) | 99 | 2.8 | (1.12-6.97) |
WHO-DAS II: World Health Organization Disability Assessment Schedule II; COPD: chronic obstructive pulmonary disease; CHF: chronic heart failure; ICF:International Classification of Functioning, Disability and Health; OR: odds ratio; 95%CI: 95% confidence interval.
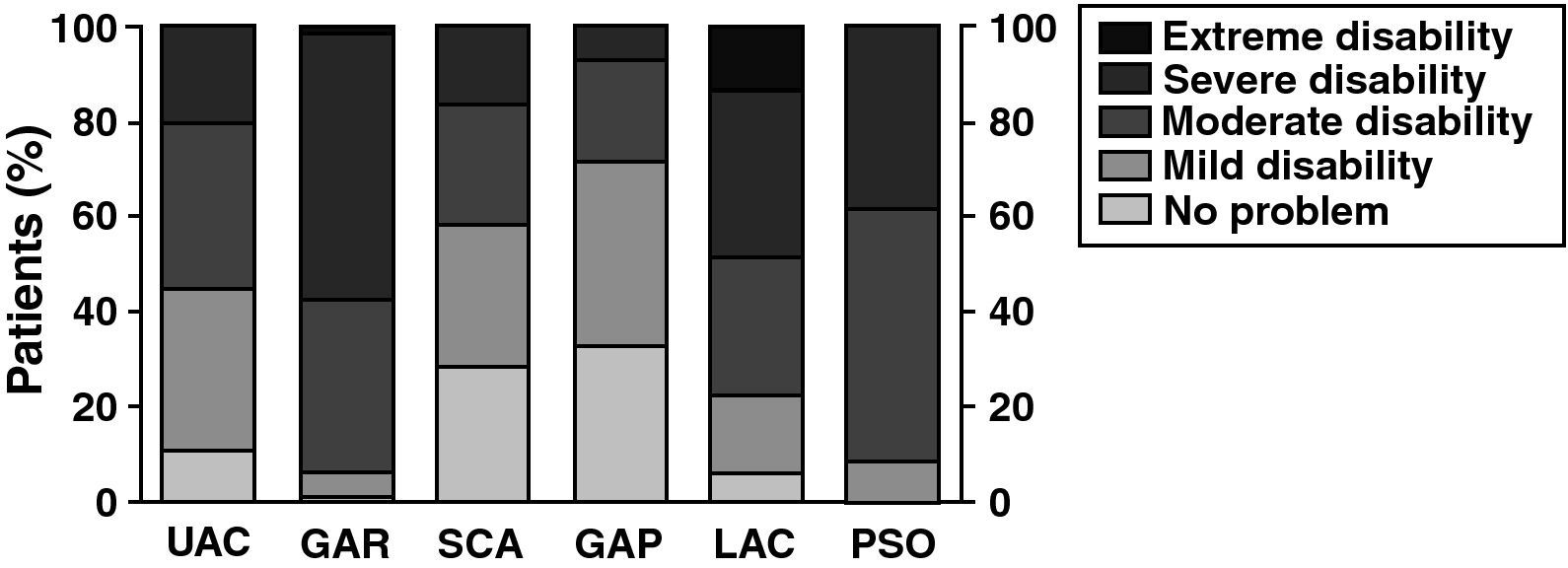
The prevalence of ICF disability categories for each of the six WHO-DAS domains among the moderate-disability group, when calculated for the global WHO-DAS II score in the diagnosis-pooled group, is shown in figure 4. There was a remarkably high prevalence of severe/extreme disability categories, namely, 58% in mobility, 50% in ife activities and 16% in self-care.
Prevalence of different International Classification of Functioning, Disability and Health (ICF) disability categories by World Health Organization Disability Assessment Schedule II (WHO-DAS II) score in different domains among the moderately disabled following global WHO-DAS II scores in the three diagnostic groups.
The results of this study suggest that the disability patterns of the three clinical populations with selected somatic disorders show different prevalences of severe/extreme disability according to the total WHO-DAS II score. Prevalence was highest for stroke and CHF, yet there were also some similar traits, the following two in particular: (i) the higher prevalence among women versus men, particularly for stroke; and (ii) the specific pattern by ICF domain, with the highest severe/extreme limitations being experienced in life activities and mobility. Severe restrictions were also seen in social participation for stroke and CHF and, to a lesser extent, for COPD. In addition, moderate disability according to total WHO-DAS II score concealed substantial proportions of persons with severe/extreme disability in mobility, life activities and self-care.
A potential weakness of this study lies in the selection having been made by non-institutional residence, physician inclusion criteria, participation, and recruitment of the most frequent primary care users, and perhaps the most disabled patients. A surprising result –attributable in part to selection bias– was the high frequency of women with COPD (38%), since COPD is linked to smoking history, which tends to be a characteristic biographical feature of Spanish men. The high level of age-adjusted disability among women with stroke is consistent with stroke being the leading cause of death among Spanish women.
Instrument properties might generate uncertainty due to the field of application. Garin et al. described WHO-DAS-based patterns of disability in seven European diagnostic groups affected by chronic diseases and revealed a latent structure originally designed by the WHO-DAS II developers18. Accordingly, the profiles described in this study for global WHO-DAS II scores may be partly due to clinical severity. Similarly, warnings of ceiling effects described for the WHO-DAS in general populations, and suggested in this study for mobility and life activities in participants classified as moderately disabled by global WHO-DAS scores, might reflect a continuum phenomenon linked to the original underlying structure.
Attention should be drawn to the remarkable disability traits in each of the three diagnostic groups, and in the moderately disabled as per global disability score. The existence of a systematically higher proportion of clinical populations showing severe/extreme disability in specific domains such as mobility and life activities –as observed in this study and in reported observations of a composite population, composed of a very old general Spanish and a comparatively younger elderly Turkish population21,22 studied using the WHO-DAS II– may suggest an instrument- or ICF-related feature. A potential explanation for this pattern is that the WHO-DAS II may specifically capture the nature of disability, i.e., aspects capable of being offset by personal help or performance. The pattern may highlight the potential usefulness of individual domain-specific WHO-DAS II scores for detecting the need for personal help and for planning resource allocation using information systems.
One implication of the concealment properties of the global WHO-DAS measure for planning is that, perhaps due to the broad scope of the ICF measurements, individuals needing personal help to counterbalance disability in mobility and life activities would remain undetected by the global score. This disadvantage points to potential shortcomings of ICF global measurements to detect the need for personal help, a key variable determining the planning and provision of services, whether by the WHO-DAS II, ICF checklist or disease-specific or generic core sets. A validated ICF-based index of need for personal help, such as that proposed on other grounds23, might be useful for screening both undetected and unmet need for help.
Caution should be exercised when interpreting reported WHO-DAS II measurements. For instance, authors use average WHO-DAS global scores of disabled persons, namely, those scoring a minimum of 1 point in each disability field20. The present authors and, occasionally, Donmetz et al22 report the prevalence of severe/extreme disability. A reason for using proportions (i.e., prevalence frequencies) is that this measure is suitable for epidemiological analysis.
Health authorities have proposed the use of medical and social resources to optimize care programs in specific groups24,25. Our results suggest that there are differential areas for improvement determined by diagnosis and that instrumental life activities and mobility generally constitute broad spheres for intervention. Information systems to be used for coordinating or monitoring care and support services should take into account disability patterns in the specific domains described in this study, along with the nature of the services provided, since these are frequently geared to reducing disability by means of distinct mechanisms, e.g., compensating limitations in household or functional improvement through personal help or improving mobility through rehabilitation26. A more in-depth approach encompassing both capacity and performance falls outside the WHO-DAS II framework and would require more sophisticated, individualized ICF measurements, including assessment of the physical and social environment, e.g., by using the ICF Checklist or specific ICF core sets.
In all likelihood, the three groups analyzed in the present study constitute a small proportion of the prevalence-etiological fraction of severe/extreme disability, which among the very old in Spain is reported to be predominantly due to mental (psychiatric and dementia) and neurological disorders, with these accounting for 59.76% (95%CI: 49.26-65.09) and 20.21% (95%CI: 7.78-26.07) of prevalent severe/extreme disability, respectively20. In this population, major diagnoses for disability, such as heart failure or stroke, yielded ORs and 95%CIs of 2.41 (0.90-6.46) and 4.42 (1.67-3.45), respectively, for severe/extreme disability according to the WHO-DAS II global score. However, the specific conditions making the highest contribution to disability status were Alzheimer's disease and depression, with prevalence-etiological fractions of 31.42% (95%CI: 28.47-59.76) and 18.62% (95%CI: 9.85-20.21), respectively. When compared with CHF, the above-mentioned 2-fold prevalence of stroke may indicate that, due to its being more or equally prevalent and more disabling than CHF, stroke generates a higher disability burden in South Madrid than either CHF or COPD.
A non-negligible issue that is not addressed in this study is the difference between disease-generated disability (as opposed to disability due to comorbidity) and disability in persons with a specific diagnosis. As stressed by Peat, attributing disability to a specific health condition of interest potentially limits insights into important interventions, such as managing comorbid interactions and targeting barriers in the physical, social, and attitudinal environment27. The approximately 2-fold prevalence of severe disability among stroke patients as compared to that in the younger COPD group (Table 1) resulted in an OR=1.62, when age was controlled for in the model. Disregarding statistical details, this difference may illustrate conceptual and empirical aspects that can probably be advantageously approached when using the ICF model in general and clinical epidemiology.
An important question when interpreting our results, as well as those yielded by studies on health-related quality of life (HRQoL), refers to differences among findings obtained when disability is assessed using traditional, disease-specific instruments. In an ICF-oriented study on neurological disorders aimed at comparing disease-specific HRQoL instrument structures, we identified limitations of these instruments, which frequently neglect instrumental activities and social participation, since they are mainly modelled on a biomedical rather than the ICF biopsychosocial paradigm28. An approximation to the well-justified use of disease-specific instruments in disability research29,30 is the development by expert consensus of selected check-list items for ICF core sets for stroke and COPD; core set validation and the development of a generic ICF core set for the elderly, among whom there is substantial multimorbidity, are also under way31–33. Caution may be required when proposing inferences from disability results obtained with distinct instruments or different core sets. A short ICF dictionary, with examples illustrating the content of specific items in the Extended Katz, Modified Check-list and WHO-DAS II 36 when assessing stroke patients, is summarized in Appendix II (on-line). In brief, the ICF model may well provide an advantageous multipurpose background for developing information systems in primary care, population surveys, or clinical management for distinct diagnostic groups
To sum up, this descriptive study shows that disability is frequently present in COPD, CHF, and stroke, with sex- and domain-related disability patterns somewhat similar to those reported for unselected elderly of advanced age by population studies. When measured by WHO-DAS II global scores, moderate disability conceals substantial proportions of severe/extreme disability, particularly in life activities and mobility, among clinical and general populations alike. Disability surveys as well as individual assessments and primary care data-monitoring systems could be widely assessed by information systems based on the ICF model. In addition to ICF disability categories, measurement of ICF-validated categories of need for personal aid might be called for.
Electronic records used in primary care should incorporate disability measurements. The International Classification of Functioning advocates the use of a multifactorial and multifaceted model of disability, which is beginning to be used in epidemiological and clinical research. Data on disability patterns assessed by means of the World Health Organization Disability Assessment Schedule II (WHO-DAS II) in somatic disorders are not well known.
What does this study add?Disability among non-institutionalized persons with chronic obstructive pulmonary disease, chronic heart failure and stroke is frequent, exhibiting sex- and domain-related patterns similar to those described in some epidemiological studies. Disability surveys, individual assessments and primary care data monitoring systems may include similar International Classification of Functioning-validated categories of disability.
J. de Pedro, A. Alberquilla and L. García-Olmos contributed to the study design. C.H. Salvador, J.L. Monteagudo and J. de Pedro conceived the study. P. García-Sagredo, A. Alberquilla and C.H. Salvador supervised the field study. M. Carmona, G. Bosca and F. López-Rodríguez assessed disability and built a data base. J. Virués and E. Alcalde analyzed the data. J. de Pedro and G Bosca wrote the first and last drafts of the manuscript. All authors contributed ideas, revised different drafts of the manuscript and approved the final version.
Financial supportThis study was partially supported by a CENIT Program (MICINN-CDTI) [CEN-2007-1010 “Digital personal environment for health and well-being – AmiVital” project], by a grant from the Carlos III Health Institute [AES FIS PI08-0435], by CIBERNED (J. Virués) and by Projects PI06/1098 and PI07/90206 from the Fondo de Investigaciones Sanitarias.
Conflict of interestNone declared.
The authors acknowledge support for implementing patient identification and selection to Dr. Juan José Muñoz (Managing Director) and Dra. Mª Teresa Alonso (Medical Director) from Primary Care Management I, Area 11 Madrid, as well as to Esther Franco, Cristina Martínez, Cristina Ruiz and Olga Burzaco from the Institute for Health Sciences of Aragon for support with training on the application of the WHO-DAS II.