The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoThe study aimed to explore factors associated with prelabor rupture of membrane (PROM) and mode of delivery of PROM at secondary health care.
MethodsIt was a retrospective case-control study within a year observational period. Data were collected from medical records at St. Khadijah I Mother and Child Hospital Makassar.
ResultsThere were 4003 samples with 259 cases with PROM. Parity and body mass index (BMI) were factors associated with PROM with p=0.000 and .032 consecutively; among them, BMI was more prominent than parity with OR=2.392, and 95% CI=1.052–5.442. Cesarean section is not associated with PROM, p=.000.
ConclusionPrimigravidae and obesity were factors associated with PROM, and BMI was more strongly associated with PROM than parity. PROM is not an indication for cesarean section.
Prelabour rupture of membranes (PROM) is a rupture of the amniotic membrane before the labor process. It is a condition frequently found at the end of pregnancy. PROM incidence is about 3% of all pregnancies, with 70% are term pregnancies; it varies about 5–10% of all deliveries. PROM is more frequent in developing countries. The prompt onset of spontaneous labor generally follows 1–4 term PROM, and it complicates 8% of pregnancies.5,6 Since the exact etiology of PROM is multifactorial and, in some cases yet still unclear, effective treatment for preventing PROM is not certain yet. The impact of PROM, especially on neonatal morbidity and mortality, is noteworthy, so it is pertinent to identify factors associated with PROM in order to anticipate PROM when it happens, to reduce the occurrence of adverse effects of PROM toward maternal and neonatal outcomes, and to promote the health of mothers and neonates. Due to PROM, frequent maternal complications are acute chorioamnionitis, subclinical chorioamnionitis, premature placental separation, and postpartum endometritis. Meanwhile, common complications of PROM to neonates are prematurity (the most common complication), sepsis, asphyxia, and respiratory distress syndrome.1,2,4
Extensive efforts were made to find out factors associated with PROM. A hospital-based study by Addisu et al. (2020) revealed that pathological vaginal discharge, urinary tract infection, vaginal hemorrhage during pregnancy, and history of PROM in a previous pregnancy are factors associated with PROM. In comparison, Endale et al. (2016) found that PROM duration and maternal residential sites were associated with PROM outcomes. Another study by Eleje et al. (2020) showed that the Chorioquick test could be used as a modality to detect chorioamnionitis in PROM patients.7–9 PROM's high-risk factors categorized as preventable (include maternal smoking, more than three cups of coffee per day in the first trimester, vaginal colonization by: Chlamydia trachomatis, Neisseria gonorrhoeae, Group B streptococci) and nonpreventable (include the history of PROM, vaginal bleeding in the first and second trimesters, cervical length <2.5cm, positive fibronectin).1,2
PROM remains an important determinant for maternal morbidity and fetal and neonatal morbidity and mortality.4 Timely identification of maternal risk factors helps to reduce the incidence and severity of PROM complications. Therefore, it is necessary to study factors associated with PROM and mode of delivery, as such that proper management could be given to mothers with certain risk factors besides given a choice for the appropriate mode of delivery.
MethodsThis was a retrospective cross-sectional study within a one-year observational period (January 1, 2019, until December 31, 2019). The population of the study was women in labor. Samples were women who gave birth in St. Khadijah I Mother and Child Hospital. This study was approved by the Health Research Ethical Committee, Faculty of Medicine Hasanuddin University. Data were collected from medical records at St. Khadijah I Mother and Child Hospital implementing consecutive sampling and statistically analyzed using the SPSS program. Bivariate analysis was performed using the Chi-square test, and multivariate analysis was using logistic regression.
ResultsWithin the period of the study, there were 4003 samples. Samples were categorized as PROM (n=259 subjects; hence the incidence of PROM in 2019 is 6.47% of all deliveries at St. Khadijah I Mother and Child Hospital Makassar) as case group and not PROM (n=3744 subjects) as a control group. Inclusion criteria were: PROM subjects were diagnosed by the history of per vaginal fluid leakage and nitrazine test, term pregnancy (>37 weeks of gestational age based on last menstrual period), and complete data on the medical record. Exclusion criteria consist of: patients were referred or dead before delivery management was performed and patients admitted to the hospital on December 31, 2018, and the delivery process occurred on January 1, 2019, and also patients admitted to the hospital on December 31, 2019, and the delivery process occurred on January 1, 2020.
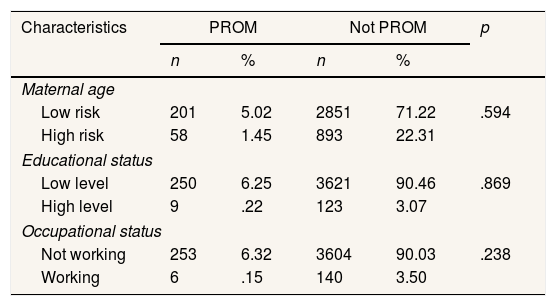
The results of the study were as follows: Table 1 shows the characteristics of study subjects. Statistical analysis revealed that maternal characteristics based on maternal age, educational status, and occupational status were homogenous.
Characteristics of subjects.
| Characteristics | PROM | Not PROM | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Maternal age | |||||
| Low risk | 201 | 5.02 | 2851 | 71.22 | .594 |
| High risk | 58 | 1.45 | 893 | 22.31 | |
| Educational status | |||||
| Low level | 250 | 6.25 | 3621 | 90.46 | .869 |
| High level | 9 | .22 | 123 | 3.07 | |
| Occupational status | |||||
| Not working | 253 | 6.32 | 3604 | 90.03 | .238 |
| Working | 6 | .15 | 140 | 3.50 | |
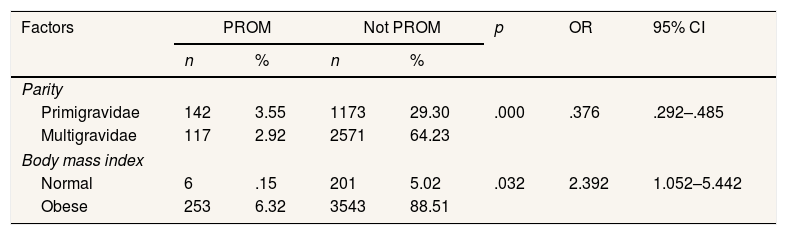
Table 2 described that parity and Body Mass Index (BMI) were factors associated with PROM, with BMI was the stronger factors related to PROM. The probability of obese pregnant women having PROM was two folds compared to normal pregnant women.
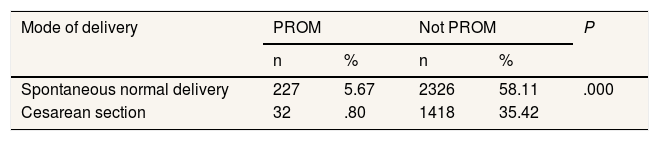
Table 3 revealed that PROM was not an indication for performing a cesarean section.
DiscussionBased on gestational age, PROM was categorized as: term PROM (PROM that occurred at >37 weeks of gestation), preterm PROM (PROM that happened <37 weeks of gestation), and Previable PROM (PROM before the fetus is viable).10 As a secondary health care, St. Khadijah I mother and child hospital does not have NICU facilities. Thus preterm cases were referred to health care with more advanced facilities. In this study, all PROM cases were term PROM.
Infection in pregnancy brings about a reduction in membrane tensile strength which eventually caused PROM. Membrane tensile strength reduction was rendered by the collagenolytic effect of metalloproteinases, the effect of bacterial proteases, or repeated stretching by uterine contractions.12
In this study, PROM is more frequent in primigravidae than multiparous. This result is in accordance with the study by Ibishi et al. (2015).4
In our study, obese mothers were inclined to encounter PROM two folds compared to non-obese mothers. At present, the most common BMI measurement used is the Quetelet index which is calculated:
According to World Health Organization (WHO), the classification of obesity was as follows11:
- -
Underweight: <18.5kg/m2
- -
Normal: 18.5–24.9kg/m2
- -
Overweight: 25–29.9kg/m2
- -
Obese:
- ∘
Class 1: 30–34.9kg/m2
- ∘
Class 2: 35–39.9kg/m2
- ∘
Class 3: ≥40kg/m2
- ∘
A study by Fallatah et al. (2019) found that obesity in pregnancy is related to a great amount of maternal and neonatal risk and eventually adverse maternal and neonatal outcomes. The study involved 1037 samples which were classified into 4 classes of obesity. Among several antepartum variables, PROM is one of them.12 A study by Wendremaire et al. (2011) showed that leptin increase in obese pregnant women has a role in myometrial apoptosis due to leptin-induced inhibition.13 The association between prelabour rupture of the membrane with obesity was also found in a study by Hautakangas et al. (2018). Their study that consisted of 598 samples revealed that obesity was an independent risk factor of labor dystocia when BMI was ≥30kg/m2 but did not affect neonatal outcome. PROM occurred in 41.9% of cases of severely obese parturients (BMI>35kg/m2).14
We also found that PROM is not an indication for cesarean section. Middleton et al. (2017), in a Cochrane Systematic Review and Metanalysis, proved that there was no clear difference between planned and expectant management for the risk of cesarean section in term pregnancy.6 But our result is not in accordance with the study conducted by Ibishi et al. (2015), which revealed an increase in cesarean section delivery due to PROM.4 Several factors must be taken into consideration before performing a cesarean section, such as maternal and neonatal morbidity and mortality and subsequent pregnancy and delivery. Clinical possibilities to avoid dystocia in obese pregnant women are limited, so it is worth trying vaginal delivery. For obese parturients, recognizing risk factors is pertinent before deciding to perform a cesarean section.14
Our study has a strength that is the fairly large study samples from a single center. Thus the homogeneity of the study is good. The data on maternal background and deliveries is reliable, collected from the patients’ medical records. The limitation of our study is that some important variables are not included due to incomplete documentation and inappropriate chart keeping. Another limitation is we did not stratified obesity according to WHO classification.
ConclusionIn this study, maternal parity and obesity were factors associated with PROM, with the latter being more strongly related to PROM. PROM is not an indication for cesarean section.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.