The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoThe purpose of this study will be to review several studies regarding the repair or treatment of perineal tears after vaginal delivery. This is expected to be an update for a midwife in daily caring.
MethodsTwo electronic databases (PubMed and Sciencedirect) were searched to locate relevant literature about perineal tears/wound/laceration/trauma that is published in 2016–2021. 124 Pubmed articles and 452 ScienceDirect articles filtered successfully. The articles that have been obtained will be evaluated based on the inclusion criteria in this study. We summarize place and date, objective, design, samples, the measurement used, and research results.
Results9 articles were found that matched the inclusion criteria. Three articles examined the effect of the type of suture on perineal pain, and another 6 discussed therapy to reduce the adverse effects of perineal tears. The therapies used are far-infrared radiation therapy, capacitive-resistive radiofrequency therapy, pelvic floor muscle training in early postpartum, cold therapy, and treatment with TheresienOl (natural oil).
ConclusionSutures and technique/suturing second-degree perineal tears or a postpartum episiotomy can affect perineal pain. Cold gel pad therapy and treatment with natural oil on perineal wounds can affect perineal pain and wound healing.
Perineal tears often occur in vaginal delivery, either spontaneously or through interventions such as an episiotomy.1,2 Approximately 85% of vaginal deliveries occur in perineal tears, which is more common in primiparas (90.8%) than multiparas (68.8%).1,3 Perineal tears can cause bleeding, infection and postpartum pain associated with the risk of depression, dyspareunia and adversely affects the quality of life and sexual health.4,5 The American College of Obstetricians and Gynecologists (ACOG) classifies perineal tears into four grades: Grade 1st is lacerations to the perineal skin only, Grade 2nd is lacerations to the perineal muscle, but not including the anal sphincter, Grade 3rd is lacerations to the anal sphincter muscle and Grade 4th is lacerations to the anal sphincter muscle anal sphincter and rectal epithelium.5
Grades 1st and 2nd are about 50% of the time at delivery. In grade 1st, because the tear is considered small, repair by suturing may not be carried out depending on the doctor's advice, while in grade 2nd, it is recommended to do suturing. Grades 3rd and fourth require more complex repairs and must be performed in the operating theater.1 Suturing the perineum can increase postpartum pain, impacting daily life, baby care, and the mother's comfort, so health workers must help mothers manage the pain they experience.6
The purpose of this study will be to review several studies regarding the repair or treatment of perineal tears after vaginal delivery.
MethodThis research is a literature review research from various articles in PubMed and ScienceDirect databases. The keywords used in the search were ‘perineal tears,’ ‘perineal wound,’ and ‘perineal laceration’. The search results found 8,246 related articles on Pubmed and 25,902 articles on ScienceDirect. Furthermore, the results will be filtered through the database by taking articles published in 2016–2021, research articles, and free full text from 124 Pubmed articles and 452 ScienceDirect articles filtered successfully. The articles that have been obtained will be evaluated based on the inclusion criteria in this study, namely: 1) not review articles, 2) the English language is available 3) articles containing clinical trials or experiments for repair or treatment of perineal tears, 4) perineal tears discussed are grade 1st and second or episiotomy.
Articles considered appropriate will be reviewed by taking data, journal title, place and date of research, objectives, research samples, research design, the measurement used, and research results.
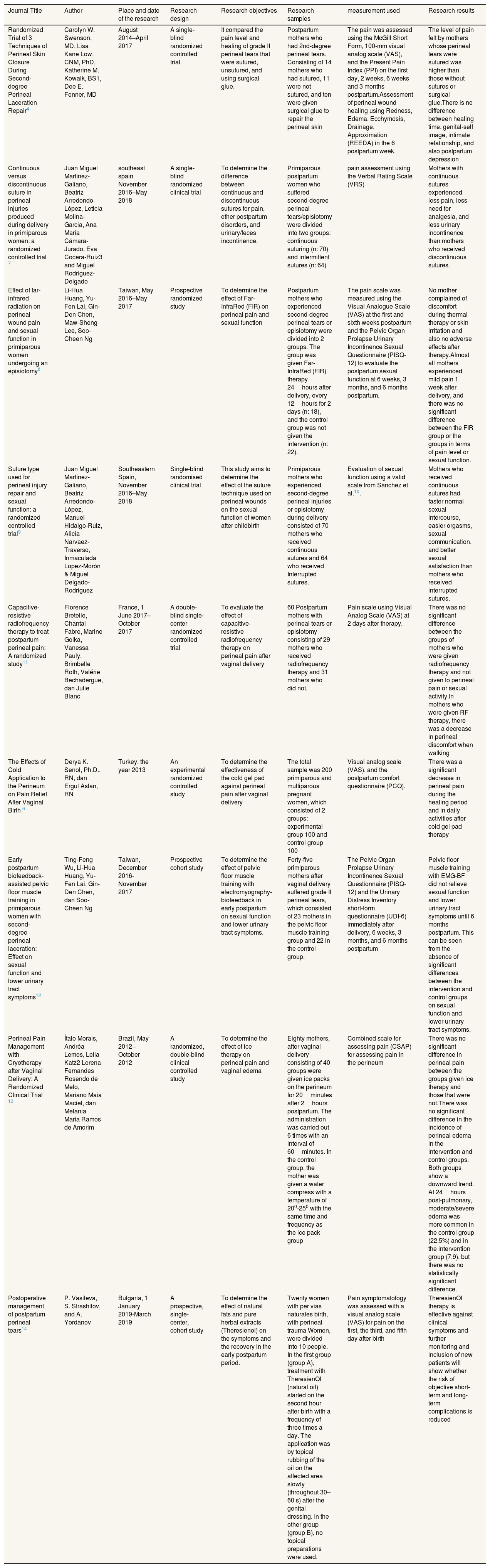
ResultNine articles were found that matched the inclusion criteria. Three articles examined the effect of this type of suture on perineal pain, and another six discussed treatments to reduce the adverse effects of perineal tears—five articles using a visual analog scale in assessing postpartum perineal tears pain (Table 1).
Journal review on Perineal wound repair or care.
| Journal Title | Author | Place and date of the research | Research design | Research objectives | Research samples | measurement used | Research results |
|---|---|---|---|---|---|---|---|
| Randomized Trial of 3 Techniques of Perineal Skin Closure During Second-degree Perineal Laceration Repair4 | Carolyn W. Swenson, MD, Lisa Kane Low, CNM, PhD, Katherine M. Kowalk, BS1, Dee E. Fenner, MD | August 2014–April 2017 | A single-blind randomized controlled trial | It compared the pain level and healing of grade II perineal tears that were sutured, unsutured, and using surgical glue. | Postpartum mothers who had 2nd-degree perineal tears. Consisting of 14 mothers who had sutured, 11 were not sutured, and ten were given surgical glue to repair the perineal skin | The pain was assessed using the McGill Short Form, 100-mm visual analog scale (VAS), and the Present Pain Index (PPI) on the first day, 2 weeks, 6 weeks and 3 months postpartum.Assessment of perineal wound healing using Redness, Edema, Ecchymosis, Drainage, Approximation (REEDA) in the 6 postpartum week. | The level of pain felt by mothers whose perineal tears were sutured was higher than those without sutures or surgical glue.There is no difference between healing time, genital-self image, intimate relationship, and also postpartum depression |
| Continuous versus discontinuous suture in perineal injuries produced during delivery in primiparous women: a randomized controlled trial 7 | Juan Miguel Martínez-Galiano, Beatriz Arredondo-López, Leticia Molina-Garcia, Ana Maria Cámara-Jurado, Eva Cocera-Ruiz3 and Miguel Rodríguez-Delgado | southeast spain November 2016–May 2018 | A single-blind randomized clinical trial | To determine the difference between continuous and discontinuous sutures for pain, other postpartum disorders, and urinary/feces incontinence. | Primiparous postpartum women who suffered second-degree perineal tears/episiotomy were divided into two groups: continuous suturing (n: 70) and intermittent sutures (n: 64) | pain assessment using the Verbal Rating Scale (VRS) | Mothers with continuous sutures experienced less pain, less need for analgesia, and less urinary incontinence than mothers who received discontinuous sutures. |
| Effect of far-infrared radiation on perineal wound pain and sexual function in primiparous women undergoing an episiotomy8 | Li-Hua Huang, Yu-Fen Lai, Gin-Den Chen, Maw-Sheng Lee, Soo-Cheen Ng | Taiwan, May 2016–May 2017 | Prospective randomized study | To determine the effect of Far-InfraRed (FIR) on perineal pain and sexual function | Postpartum mothers who experienced second-degree perineal tears or episiotomy were divided into 2 groups. The group was given Far-InfraRed (FIR) therapy 24hours after delivery, every 12hours for 2 days (n: 18), and the control group was not given the intervention (n: 22). | The pain scale was measured using the Visual Analogue Scale (VAS) at the first and sixth weeks postpartum and the Pelvic Organ Prolapse Urinary Incontinence Sexual Questionnaire (PISQ-12) to evaluate the postpartum sexual function at 6 weeks, 3 months, and 6 months postpartum. | No mother complained of discomfort during thermal therapy or skin irritation and also no adverse effects after therapy.Almost all mothers experienced mild pain 1 week after delivery, and there was no significant difference between the FIR group or the groups in terms of pain level or sexual function. |
| Suture type used for perineal injury repair and sexual function: a randomized controlled trial9 | Juan Miguel Martínez-Galiano, Beatriz Arredondo-López, Manuel Hidalgo-Ruiz, Alicia Narvaez-Traverso, Inmaculada Lopez-Morón & Miguel Delgado-Rodriguez | Southeastern Spain, November 2016–May 2018 | Single-blind randomised clinical trial | This study aims to determine the effect of the suture technique used on perineal wounds on the sexual function of women after childbirth | Primiparous mothers who experienced second-degree perineal injuries or episiotomy during delivery consisted of 70 mothers who received continuous sutures and 64 who received Interrupted sutures. | Evaluation of sexual function using a valid scale from Sánchez et al.10. | Mothers who received continuous sutures had faster normal sexual intercourse, easier orgasms, sexual communication, and better sexual satisfaction than mothers who received interrupted sutures. |
| Capacitive-resistive radiofrequency therapy to treat postpartum perineal pain: A randomized study11 | Florence Bretelle, Chantal Fabre, Marine Golka, Vanessa Pauly, Brimbelle Roth, Valérie Bechadergue, dan Julie Blanc | France, 1 June 2017–October 2017 | A double-blind single-center randomized controlled trial | To evaluate the effect of capacitive-resistive radiofrequency therapy on perineal pain after vaginal delivery | 60 Postpartum mothers with perineal tears or episiotomy consisting of 29 mothers who received radiofrequency therapy and 31 mothers who did not. | Pain scale using Visual Analog Scale (VAS) at 2 days after therapy. | There was no significant difference between the groups of mothers who were given radiofrequency therapy and not given to perineal pain or sexual activity.In mothers who were given RF therapy, there was a decrease in perineal discomfort when walking |
| The Effects of Cold Application to the Perineum on Pain Relief After Vaginal Birth 6 | Derya K. Senol, Ph.D., RN, dan Ergul Aslan, RN | Turkey, the year 2013 | An experimental randomized controlled study | To determine the effectiveness of the cold gel pad against perineal pain after vaginal delivery | The total sample was 200 primiparous and multiparous pregnant women, which consisted of 2 groups: experimental group 100 and control group 100 | Visual analog scale (VAS), and the postpartum comfort questionnaire (PCQ). | There was a significant decrease in perineal pain during the healing period and in daily activities after cold gel pad therapy |
| Early postpartum biofeedback-assisted pelvic floor muscle training in primiparous women with second-degree perineal laceration: Effect on sexual function and lower urinary tract symptoms12 | Ting-Feng Wu, Li-Hua Huang, Yu-Fen Lai, Gin-Den Chen, dan Soo-Cheen Ng | Taiwan, December 2016-November 2017 | Prospective cohort study | To determine the effect of pelvic floor muscle training with electromyography-biofeedback in early postpartum on sexual function and lower urinary tract symptoms. | Forty-five primiparous mothers after vaginal delivery suffered grade II perineal tears, which consisted of 23 mothers in the pelvic floor muscle training group and 22 in the control group. | The Pelvic Organ Prolapse Urinary Incontinence Sexual Questionnaire (PISQ-12) and the Urinary Distress Inventory short-form questionnaire (UDI-6) immediately after delivery, 6 weeks, 3 months, and 6 months postpartum | Pelvic floor muscle training with EMG-BF did not relieve sexual function and lower urinary tract symptoms until 6 months postpartum. This can be seen from the absence of significant differences between the intervention and control groups on sexual function and lower urinary tract symptoms. |
| Perineal Pain Management with Cryotherapy after Vaginal Delivery: A Randomized Clinical Trial 13 | Ítalo Morais, Andréa Lemos, Leila Katz2 Lorena Fernandes Rosendo de Melo, Mariano Maia Maciel, dan Melania Maria Ramos de Amorim | Brazil, May 2012–October 2012 | A randomized, double-blind clinical controlled study | To determine the effect of ice therapy on perineal pain and vaginal edema | Eighty mothers, after vaginal delivery consisting of 40 groups were given ice packs on the perineum for 20minutes after 2hours postpartum. The administration was carried out 6 times with an interval of 60minutes. In the control group, the mother was given a water compress with a temperature of 200-250 with the same time and frequency as the ice pack group | Combined scale for assessing pain (CSAP) for assessing pain in the perineum | There was no significant difference in perineal pain between the groups given ice therapy and those that were not.There was no significant difference in the incidence of perineal edema in the intervention and control groups. Both groups show a downward trend. At 24hours post-pulmonary, moderate/severe edema was more common in the control group (22.5%) and in the intervention group (7.9), but there was no statistically significant difference. |
| Postoperative management of postpartum perineal tears14 | P. Vasileva, S. Strashilov, and A. Yordanov | Bulgaria, 1 January 2019-March 2019 | A prospective, single-center, cohort study | To determine the effect of natural fats and pure herbal extracts (Theresienol) on the symptoms and the recovery in the early postpartum period. | Twenty women with per vias naturales birth, with perineal trauma Women, were divided into 10 people. In the first group (group A), treatment with TheresienOl (natural oil) started on the second hour after birth with a frequency of three times a day. The application was by topical rubbing of the oil on the affected area slowly (throughout 30–60 s) after the genital dressing. In the other group (group B), no topical preparations were used. | Pain symptomatology was assessed with a visual analog scale (VAS) for pain on the first, the third, and fifth day after birth | TheresienOl therapy is effective against clinical symptoms and further monitoring and inclusion of new patients will show whether the risk of objective short-term and long-term complications is reduced |
This review found that the type/technique of sutures used in repairing second-degree perineal tears or episiotomy affects the perineal pain felt by postpartum mothers. The gold standard for repairing perineal wounds is to use absorbable sutures.15 However, suturing the second-degree perineal skin tears can increase postpartum pain compared to unsutured or given surgical glue.4 The technique/type of perineal suture can affect perineal pain, where continuous sutures experience lower perineal pain, better sexual activity, and lower need for analgesia than mothers who are interrupted sutures.7,9 This is due to the use of less material and also fewer knots.9 Post-suturing pain is caused by the inflammatory response of the sutures, which can last until the sutures are removed or absorbed by the body.4 Leaving the perineal skin unsutured, especially in grade 1st and grade 2nd perineal tears may reduce postpartum pain from day 14 to 6 weeks, in addition to reducing the use of analgesia and the incidence of dyspareunia at three months postpartum, but can leave gaping scars and long-term effects of this action is not yet known.5,15,16
Postpartum care, especially for mothers who have perineal tears, needs to be considered to prevent chronic pain after delivery, help mothers control pain, prevent constipation and monitor urinary retention.5,17 It is necessary to use various pharmacological and non-pharmacological methods and safe drugs for the mother to reduce postpartum pain or maternal morbidity due to perineal tears and the side effects of perineal tears.14 The provision of far-infrared radiation therapy, capacitive-resistive radiofrequency therapy, pelvic floor muscle training in early postpartum did not provide additional impact in reducing perineal pain or sexual function. However, radiofrequency therapy helps reduce perineal discomfort when walking.11 Cold therapy on the perineum for 20min can reduce perineal pain and increase the release of endorphins and stimulate the healing process.1,5,6,13 Administration of TheresienOl (a natural oil) can reduce perineal wound pain and reduce swelling and erythema. The described medicine acts by the following mechanism: 1) Hydrates tissues; 2) Reduce bacterial invasion and inflammation; 3) Stimulates migration and proliferation of fibroblastic and endothelial cells; 4) Stimulates epithelialization.14 The medications reviewed in this article do not cause any adverse health effects.
ConclusionSutures and technique/suturing second-degree perineal tears or a postpartum episiotomy can affect perineal pain. Cold gel pad therapy and treatment with natural oil on perineal wounds can affect perineal pain and wound healing.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.