Edited by: Carme Borell
Last update: March 2023
More infoCommunity health can reduce inequalities in health and improve the health of the most disadvantaged populations. In 2007, Barcelona Salut als Barris (Barcelona Health in the Neighbourhoods) was launched, a community health programme to reduce social inequalities in health. In 2018, this programme reached the 25 most disadvantaged neighbourhoods of the city. This article shares the lessons learned after 12 years of work. The programme was initially funded by a research grant and the funds were maintained during the economic crisis and were tripled when the programme became a political priority in the last municipal government. During the 12-year period, partnerships with stakeholders were generally stable and productive. Maximum community participation was obtained in the detection of health assets and needs and in action plans. During 2018, Barcelona Salut als Barris worked with more than 460 agents that co-produced 183 interventions involving more than 13,600 people. Most of the interventions assessed showed improvements in the health of participants, which could help to reduce health inequalities. The greatest difficulties were: a) citizen participation, b) the sustainability of working groups over the years, c) conflicts of interest, d) the sustainability of interventions, e) reaching certain minority groups and f) evaluation. The increase in resources in the last period contributed to the maturity and expansion of the programme. Key factors in its scope and results were political will, strong technical capacity and methodology, strong intersectoral partnerships and continued community work.
La salud comunitaria puede reducir las inequidades en salud y mejorar la salud de las poblaciones más desfavorecidas. En 2007 se inició Barcelona Salut als Barris (Barcelona Salud en los Barrios), un programa de salud comunitaria para reducir las desigualdades sociales en salud. En 2018, el programa alcanzó los 25 barrios más desfavorecidos de la ciudad. Este artículo comparte las lecciones aprendidas tras 12 años de trabajo. Los primeros fondos del programa procedieron de una beca de investigación, se mantuvieron durante la crisis económica y se triplicaron cuando pasó a ser una prioridad política en el último gobierno municipal. Durante estos 12 años, las alianzas con las partes interesadas se mantuvieron, en general, estables y productivas. La máxima participación comunitaria se obtuvo en la detección de activos y necesidades en salud y en los planes de acción. Durante 2018, Barcelona Salut als Barris trabajó con más de 460 agentes que coprodujeron 183 intervenciones en las que participaron más de 13.600 personas. Gran parte de las intervenciones evaluadas mostraron mejoras en la salud de las personas participantes, pudiendo contribuir a la reducción de desigualdades. Las mayores dificultades fueron: a) la participación ciudadana, b) la sostenibilidad de los grupos de trabajo a lo largo de los años, c) los conflictos de intereses, d) la sostenibilidad de las intervenciones, e) acceder a algunos grupos minoritarios y e) la evaluación. El aumento de los recursos del último periodo contribuyó a la madurez y la extensión del programa. La voluntad política, una sólida capacidad técnica y metodológica, consolidadas alianzas intersectoriales y el trabajo comunitario continuado han sido factores clave de su alcance y resultados.
In the last few decades, social inequalities in health have become a priority in public health at the supranational, national and local levels.1 In cities, citizen's health is influenced by the natural and built environments, as well as by socioeconomic determinants. These social determinants affect citizens’ health by worsening the health of those living in the most underprivileged neighbourhoods.2 Community health has been defined as a multi-sector and multidisciplinary approach to engage and work with communities to improve people's health and quality of life.3 Despite the difficulties of evaluating community health, current data support the idea that such evaluation can be effective in addressing social inequalities in health4 and can help to improve health and social support in disadvantaged populations.5–7 Several community health programmes in urban areas (such as in Glasgow, Rotterdam, and Amsterdam) have been shown to improve health and socioeconomic factors and reduce social inequalities.8–11 In Spain, programmes with this aim have been steadily implemented in cities and territories, such as Gente Saludable,12RIU Project,13COMSALUT Programme14 and Barcelona Salut als Barris (Barcelona Health in the Neighbourhoods).15 Other strategies also promote health through community participation, such as the mapping of health assets, aimed at strengthening social networks and facilitating the creation of intersectoral spaces.16,17 In Barcelona, strategies such as the Social Services Community Plan,18 Community Development Plans19 and Barcelona Neighbourhoods Plan,20 have created highly important synergies that have reinforced community health interventions.4,21
Barcelona Health in the Neighbourhoods programme: history and contextBarcelona, with a population of 1,620,343 inhabitants,22 is organised into 73 neighbourhoods. In 2004, the Catalonia Neighbourhoods Law (Law 2/2004) was designed to improve living conditions in the most disadvantaged neighbourhoods of Catalonia, mainly through town planning interventions.23 A year later, the Health in the Neighbourhoods programme was developed by the Catalonian Department of Health to improve the health of residents of those neighbourhoods benefitted by the Neighbourhoods Law and to reduce social inequalities in health between neighbourhoods through community health interventions.24 In Barcelona, this programme was reinforced and called Barcelona Health in the Neighbourhoods (BHiN). BHiN is a community health programme carried out in the most disadvantaged neighbourhoods of Barcelona to reduce health inequalities between them and the rest of the city. The programme was launched in 2007 with the co-leadership of: a) the Public Health Agency of Barcelona; b) the institution responsible for health care in the city (Consorci Sanitari de Barcelona); and c) the city Council. Nowadays, BHiN is one of the oldest community health strategies in Spain.25 The programme, based on public health, health promotion and community health models;26,27 encompasses five phases: 1) alliances with stakeholders; 2) health needs assessment; 3) an action plan; 4) monitoring and evaluation; and 5) sustainability (see Table I in online Appendix). From 2007-2008, BHiN was partially funded by a research grant from the Spanish Ministry of Health. As a research project, BHiN was carried out in two neighbourhoods of Barcelona, and after 3 years, the feasibility and achievements of the community model were assessed with good results.15 Subsequently, the rest of the neighbourhoods benefitted by the Catalonia Neighbourhoods Law were progressively included in the BHiN strategy, until encompassing all of them in 2015. Since then, other neighbourhoods have been incorporated using the Urban Heart instrument in Barcelona, a tool that includes 15 health and social determinants-related indicators that allowed identification of the neighbourhoods in the city with the worse indicators.28 In 2018, BHiN reached the 25 most disadvantaged neighbourhoods in the city.29
This article aimed to describe some lessons learned about the history of the BHiN strategy after 12 years of collaborative work. The article describes the structural aspects of the programme, its implementation process and its most relevant health outcomes through documentary analysis30 and consensus among all authors.
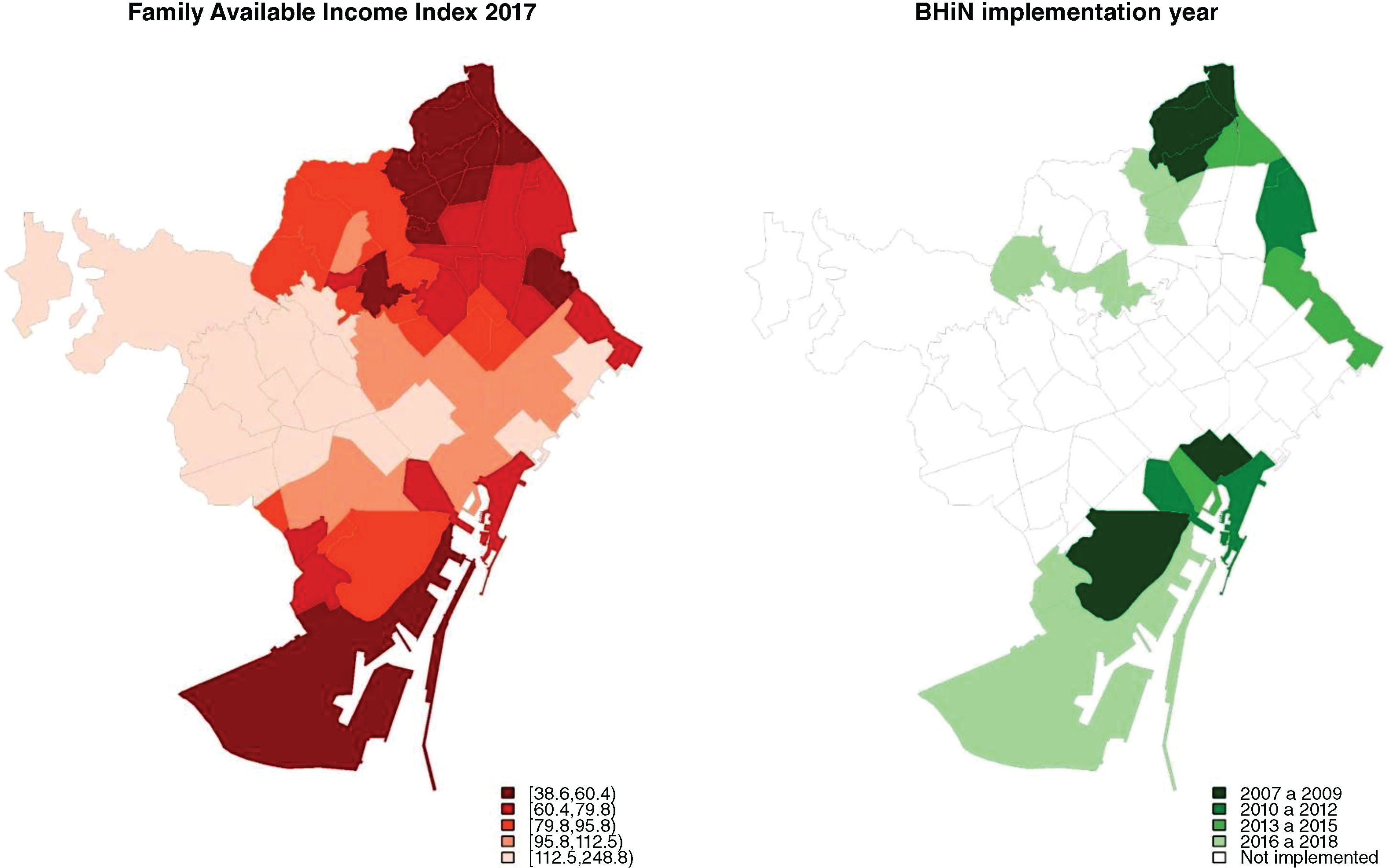
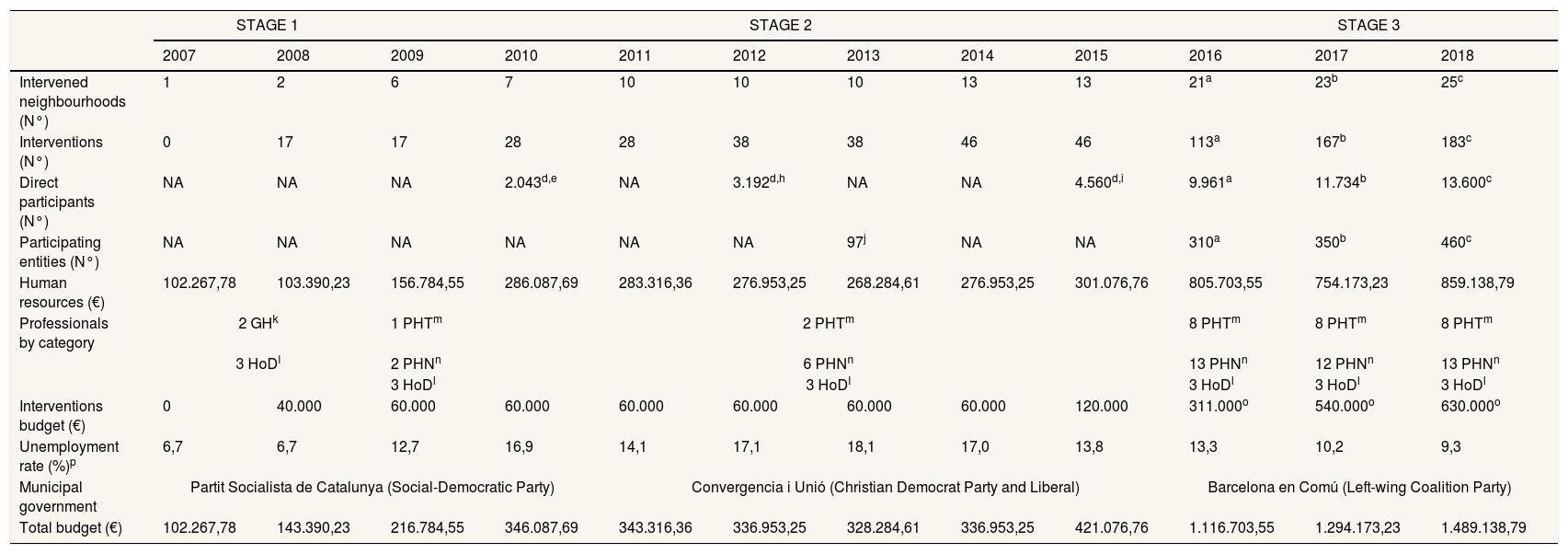
Structural aspects of the programmeThe running costs and other implementation related variables from 2007 to 2018 are shown in Table 1. BHiN has been implemented in the neighbourhoods with the worst Family Available Income Index (Fig. 1). This index includes five indicators and reflects the distribution of the neighbourhood mean family income compared with the city mean.28 During the 12 years of BHiN, three different stages can be distinguished, defined by the municipal government, the economic context and the resources allocated to the programme: stage 1 (from 2007 to 2008), stage 2 (from 2009 to 2015), and stage 3 (from 2016 to 2018). In stage 1, the programme was funded by a research grant; in stage 2, limited resources were allocated by the Public Health Agency of Barcelona; and in stage 3, the resources were tripled by the new left-wing government (Barcelona en Comú) since social inequalities in health became a priority in their political agenda.19,31 This political will transformed the programme, generating the following substantial positive changes: a) an increase in the number of neighbourhoods served; b) an increase in the number and variety of interventions; and c) the hiring of 13 new public health professionals (Table 1). These changes improved the coordination between the programme and the stakeholders and the generation of a new annual report of process indicators.29 From 2007 to 2018, the programme grew progressively, even though the city faced a major economic crisis. The increase of served neighbourhoods, interventions, direct participants and entities was directly proportional to the economic resources allocated to the programme each year (Table 1).
Barcelona Health in the Neighbourhoods running costs and other implementation-related variables per year. From 2007 to 2018.
| STAGE 1 | STAGE 2 | STAGE 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
| Intervened neighbourhoods (N°) | 1 | 2 | 6 | 7 | 10 | 10 | 10 | 13 | 13 | 21a | 23b | 25c |
| Interventions (N°) | 0 | 17 | 17 | 28 | 28 | 38 | 38 | 46 | 46 | 113a | 167b | 183c |
| Direct participants (N°) | NA | NA | NA | 2.043d,e | NA | 3.192d,h | NA | NA | 4.560d,i | 9.961a | 11.734b | 13.600c |
| Participating entities (N°) | NA | NA | NA | NA | NA | NA | 97j | NA | NA | 310a | 350b | 460c |
| Human resources (€) | 102.267,78 | 103.390,23 | 156.784,55 | 286.087,69 | 283.316,36 | 276.953,25 | 268.284,61 | 276.953,25 | 301.076,76 | 805.703,55 | 754.173,23 | 859.138,79 |
| Professionals by category | 2 GHk | 1 PHTm | 2 PHTm | 8 PHTm | 8 PHTm | 8 PHTm | ||||||
| 3 HoDl | 2 PHNn | 6 PHNn | 13 PHNn | 12 PHNn | 13 PHNn | |||||||
| 3 HoDl | 3 HoDl | 3 HoDl | 3 HoDl | 3 HoDl | ||||||||
| Interventions budget (€) | 0 | 40.000 | 60.000 | 60.000 | 60.000 | 60.000 | 60.000 | 60.000 | 120.000 | 311.000o | 540.000o | 630.000o |
| Unemployment rate (%)p | 6,7 | 6,7 | 12,7 | 16,9 | 14,1 | 17,1 | 18,1 | 17,0 | 13,8 | 13,3 | 10,2 | 9,3 |
| Municipal government | Partit Socialista de Catalunya (Social-Democratic Party) | Convergencia i Unió (Christian Democrat Party and Liberal) | Barcelona en Comú (Left-wing Coalition Party) | |||||||||
| Total budget (€) | 102.267,78 | 143.390,23 | 216.784,55 | 346.087,69 | 343.316,36 | 336.953,25 | 328.284,61 | 336.953,25 | 421.076,76 | 1.116.703,55 | 1.294.173,23 | 1.489.138,79 |
Evaluation reports of all BHIN: a Report 2016; bReport 2017; cReport 2018
N° direct participants according to neighborhoods: dPoble Sec; eRoquetes: fSant Pere-Sta Caterina-La Ribera; gZona Nord; h Barceloneta; iBon Pastor I Baró de Viver (Neighbourhoods evaluation report)
j Ferran Daban, Núria Calzada, Maribel Pasarín, Elia Díez, Lucia Artazcoz, Carme Borrell. Summary of activity of Health in the Neighbourhoods, 2013. Barcelona: Agència de Salut Pública de Barcelona, 2013
Professionals by category and % of time dedicated: kResearch grant holder (100%); lHead of Department (33%); mPublic health technician (100%); nPublic health nurse (50%)
o Government Measure19
p Unemployment rate in all of Barcelona (Labour Force Survey, 2° trimester) http://www.bcn.cat/estadistica/catala/dades/ttreball/epa/epa/patu/evtated.htm
NA: Not available
Family Available Income Index in 2017 and first year of BHiN implementation in the neighbourhoods from 2007 to 2018.
Compound index that includes five indicators (people aged 25 years or more with university education (%), registered unemployment among people aged 16 to 64 years (%), number of cars per inhabitant, new cars (less than 2 years) with more than 16 Hp (%) and second-hand housing prices).28.
As already stated, BHiN encompasses five phases. The main strengths and lessons learned in each phase are summarised in Table I in online Appendix. In the first phase, alliances with stakeholders remained fairly stable and productive during the 12 years. The alliances were established at the political, technical and community level in each neighbourhood. These characteristics contributed to the sustainability and maturity of the programme and generated effective community-based interventions that were replicated in other neighbourhoods. All five phases were directed by multidisciplinary and multisectoral working groups. Professionals working on the community development plans usually played an important role, leading community networks and contributing to building trust within the working group. The second phase, health needs assessment, was successfully carried out in all neighbourhoods. Quantitative and qualitative methods were combined for data collection, analysis and interpretation. This was the phase with the highest neighbourhood participation. Community organisations and neighbourhood residents participated in the design of the qualitative process for the detection of needs and assets, and subsequently in 1-day meeting group to determine a list of priorities.32 Later, in the third phase, action plan, community programmes were implemented to address the selected health priorities. Action plans from 2007 to 2015 were characterised by the design, implementation and evaluation of new interventions. Whenever possible, the design of the interventions was based on the available evidence and combined with the proposals of the working groups. In the last years (2016-2018), the action plan was characterised by scaling up and adapting the interventions to new neighbourhoods, although in neighbourhoods with active working groups, new interventions were launched that addressed health priorities. This was the phase in which the working group was most active and motivated, generating more than six interventions in some neighbourhoods.30 In contrast, only one or two interventions were carried out in other neighbourhoods for different reasons (see Table I in online Appendix). During 2018, in the 25 neighbourhoods involved in BHiN, a total of 183 interventions were co-produced with more than 460 different agents and more than 13,600 participants.29 Not all interventions were different: most were effective interventions carried out in stages 1 and 2 that were scaled up to new neighbourhoods from stage three. In the fourth phase, monitoring and evaluation processes represented a major challenge. The main reasons were: a) professional overload; b) lack of time for formal evaluation; c) the difficulty of collecting data from vulnerable groups about sensitive or upsetting topics; d) cultural alignment with different migrant populations with distinct languages, values and cultural traditions; and e) lack of awareness of the importance of evaluation. Despite these difficulties, most interventions were evaluated or are currently in the process of evaluation (see Table II in online Appendix). Finally in the fifth phase, the sustainability, was reached after an average of 3 to 5 years of collaborative work in each neighbourhood. The increase in human and economic resources was crucial to sustain the programme and interventions. In this phase, a health needs assessment was carried out again to identify new needs and generate new interventions, with the process thus being iterative and circular (see Table I in online Appendix).
Effectiveness of interventions and health outcomesAs mentioned above, most interventions were evaluated and showed positive results and some are currently under assessment (see Table II in online Appendix): a) a parenting skills programme improved child-rearing skills and social support among parents, and reduced children's negative behaviours and parental stress;33 b) a community counselling intervention increased the consistent use of contraception in participants and reduced adolescent fertility rates in the neighbourhoods included in the programme;34 c) an intervention providing weekly outings for elderly people isolated at home due to architectural barriers improved self-rated health and mental health, and reduced participants’ anxiety;35 and d) an occupational training programme for young people increased young women's self-esteem.36 Other interventions showed favourable preliminary results.37,38 Finally, an as example of the evaluation process, we are currently evaluating the effectiveness and cost-effectiveness of a programme of health schools for older people, which provide 22 weekly planned group sessions.39
Lessons learned: strengths, limitations and barriersBHiN is a community health programme that grew progressively over a 12-year period. We identified four main strengths:
- •
A consistent methodology maintained over time:26,27 the interventions were designed through multisectoral working groups, based on prior assessment of health needs and assets and on the scientific evidence.
- •
Community work:29 the interventions were implemented through community work and were evaluated. This circular process progressively improved over the years due to a continued intersectoral and community strategy.
- •
Political will that led to the growth of economic and human resources:19,31 political commitment in the last 4 years contributed very positively to the sustainability and maturity of BHiN. This support came when the programme already had 8 years of experience, an important factor that helped to increase its efficiency.
The stability of available funds: as the funds allocated to the program increased, the served neighbourhoods, interventions, direct participants, entities and human resources increased. Community health programmes need resources to be successfully implemented and to become an effective strategy to improve health and social support in disadvantaged populations.
We also identified some limitations and barriers for the implementation of the programme, such as limited citizen participation in the working groups. Citizens have usually participated through entities or neighbourhood associations. The main reasons for the low participation were the schedule of meetings, limited availability of time, cultural diversity with highly diverse views, and lack of motivation (see Table I in online Appendix). Overcoming these barriers is crucial as citizen participation can provide knowledge and ideas that can be useful to improve population health.40 More inclusive, flexible and motivating community spaces should be promoted to broaden participation.
In some neighbourhoods, the working group was less active in some phases of the programme, such as health assessment or evaluation, mainly due to lack of time or experience in methodological aspects (see Table I in online Appendix). To address these barriers and promote community health action, the Public Health Agency of Barcelona provided training to community agents. In addition, the Catalonian Department of Health developed the COMSALUT programme, to facilitate methodology tools and coaching to primary health care teams and public health technicians to boost local community health.14 It would be beneficial if other sectors that could play a key role in the development of BHiN were to participate in these resources to achieve the full potential of community-based programmes. Another limitation identified in working groups was the difficulty of maintaining motivation over time, especially in groups where interventions were delayed or scarce. In addition, in some neighbourhoods, the action plan failed because of a lack of communication, lack of time, and conflicts of interest among the members of the working group. In contrast, groups with good communication, a tradition of community action, and focused on the common good, generated several interventions and remained motivated.30 One of the most satisfactory elements of the working group members was seeing the interventions and the results of their work. Likewise, scheduled renewal of members after some years could help to promote new ideas and sustain motivation.
An important objective was to reach and work together with persons most in need (e.g. socially isolated older people, some migrant populations, and long term unemployed people), but this was not always possible. This failure can be explained by several factors: a) lack of motivation; b) lack of information about the interventions; c) lack of time; and d) interventions perceived as not useful to cover the needs of these individuals. Some strategies are being implemented to reach people who are most in need: a) designing the intervention together with these persons; b) translating the information into different languages; and c) increasing the resources devoted to dissemination.
Regarding evaluation, an important limitation was the small sample size of participants per intervention, making it necessary to analyse different years and neighbourhoods together, with all the limitations that this might entail. On some occasions, it proved difficult to properly explain the importance of evaluation to the other sectors involved, causing resistance to the evaluation process.
ChallengesOne of the main challenges of the programme was the sustainability of the interventions (see Table I in online Appendix). Interventions that were most likely to be sustained were those that had the full involvement of several sectors and those needing fewer resources. Strategies to consolidate the sustainability of the interventions with higher economic costs implied transfer the intervention to other sectors or the direct involvement of other administrations. It is essential that community programmes influence the agendas, objectives and plans of different stakeholders in the neighbourhood. Another challenge is to guarantee that the interventions designed and implemented have an intersectional perspective, that is, that they are culture and gender sensitive.41
Some of the evaluated interventions showed positive health effects in their participants.33–38 It is also known that community processes and intersectorial work can improve people's health and reduce social inequalities in health.7 These effective interventions have been scaled up to other neighbourhoods in order to expand their effects, and community processes were increased in most of the neighbourhoods intervened.29 However, we have not evaluated the potential effect on health inequalities at the population level. Since there is evidence of the effectiveness of this type of intervention and their community processes in reducing health inequalities,4,7 in the near future we will evaluate these effects at the population level in Barcelona city.
A series of relevant factors to reduce social inequalities in health came together in the last few years in Barcelona;31 even so, sustained and better collaborative work between agents and sectors, enhanced technical capacity, higher citizen participation and the continuous support of the political sector must be attained to more effectively address social health inequalities through community health action. New and sustained relationships must be forged to promote this collaboration.40
ConclusionBHiN is a good example of a community health programme aiming to tackle health inequalities. The experience of these 12 years may serve future programmes in other territories with similar objectives. Key factors in its scope and results are political will, strong technical capacity and methodology, economic resources, strong partnerships and continued intersectoral and community work.
Editor in chargeC. Álvarez-Dardet.
Authorship contributionsF. Daban, C. Borrell, M.I. Pasarín, L. Artazcoz and E. Díez conceived and designed the study and interpreted the data. F. Daban and V. Porthé wrote the first draft and analysed and interpreted the data. A. Pérez and A. Fernández critically reviewed previous drafts of the manuscript and made substantial intellectual contributions. The BHiN group contributed substantially to the drafting and critically revising the manuscript. All authors approved the final version for publication, take responsibility for its contents, and guarantee that all aspects composing the manuscript have been reviewed and discussed among them to ensure maximum accuracy and integrity.
AcknowledgementsTo all the people who have enabled the implementation and development of Barcelona Health in the Neighbourhoods. We thank the Human Resources Department of the Barcelona Public Health Agency for its collaboration in making available the necessary information presented in this manuscript. We would also like to thank the four reviewers of this manuscript who have contributed to the marked improvement of our work. We thank Gail Craigie for her help in correcting the English version of this article.
This article forms part of the doctoral dissertation of F. Daban Aguilar at the Universitat Pompeu Fabra of Barcelona.
FundingNone.
Conflicts of interestThe signatories of this article work at the Public Health Agency of Barcelona, some of them in management positions, and therefore they have been involved in most of the interventions described in this manuscript.