In Spain, responsibility for care of old people and those in situations of dependency is assumed by families, and has an unequal social distribution according to gender and socioeconomic level. This responsibility has negative health effects on the carer. In 2006, the Dependency Law recognised the obligation of the State to provide support. This study analyses time trends in health inequalities attributable to caregiving under this new law.
MethodsStudy of trends using two cross-sectional samples from the 2006 and 2012 editions of the Spanish National Health Survey (27,922 and 19,995 people, respectively). We compared fair/poor self-rated health, poor mental health (GHQ-12 >2), back pain, and the use of psychotropic drugs between non-carers, carers sharing care with other persons, and those providing care alone. We obtain prevalence ratios by fitting robust Poisson regression models.
ResultsWe observed no change in the social profile of carers according to gender or social class. Among women, the difference in all health indicators between carers and non-carers tended to decrease among those sharing care but not among lone carers. Inequalities tend to decrease slightly in both groups of men carers.
ConclusionsBetween 2006 and 2012, trends in health inequalities attributable to informal care show different trends according to gender and share of responsibility. It is necessary to redesign and implement policies to reduce inequalities that take into account the most affected groups, such as women lone carers. Policies that strengthen the fair social distribution of care should also be adopted.
En España, el cuidado de las personas mayores o en situación de dependencia es desempeñado por las familias, con desigual distribución social según género y nivel socioeconómico. Esta responsabilidad afecta negativamente a la salud de quienes cuidan. En 2006, la Ley de Dependencia reconoció la obligación del Estado de atender esta situación. Este estudio analiza la evolución de las desigualdades en salud atribuibles al cuidado en el contexto de la ley.
MétodoEstudio de tendencias basado en las ediciones de 2006 y 2012 de la Encuesta Nacional de Salud de España (27.922 y 19.995 personas, respectivamente). Se obtuvieron razones de prevalencia robusta mediante modelos de Poisson para comparar mala salud autopercibida, mala salud mental (GHQ-12 >2), lumbalgia crónica y uso de psicotrópicos entre quienes no cuidaban, quienes compartían con alguien el cuidado y quienes cuidaban en solitario.
ResultadosEl perfil de las personas cuidadoras permaneció invariable según género y nivel socioeconómico. Entre las mujeres, las desigualdades en salud, respecto a las que no cuidaban, se redujeron para aquellas que compartían el cuidado, manteniéndose para las que cuidaban en solitario. En los hombres, las desigualdades disminuyeron para ambos grupos de cuidadores respecto a no cuidadores.
ConclusionesEntre 2006 y 2012, la evolución de las desigualdades en salud atribuibles al cuidado informal muestra diferentes tendencias según género y reparto de responsabilidad. Son necesarias políticas dirigidas a reducir estas desigualdades valorando los grupos más afectados, como las mujeres que cuidan solas. Además, deben adoptarse políticas que fortalezcan una distribución social más equitativa del cuidado.
The organisation of care for elderly people or individuals with functional diversity is one of the main challenges faced by western societies at the beginning of the 21st century. The “crisis of care” has intensified as women have progressively moved into the paid labour force and as fertility rates decrease and life expectancy increases in many countries. These ageing societies have resulted in heavy pressures on families and also on welfare state regimes.1
The provision of care varies across Europe according to labour markets and welfare state regimes. Mediterranean countries form a distinctive cluster where the management of care is delegated almost entirely to the family, mostly to women in the private sphere.2 Care is predominantly provided by women, based in traditional gender stereotype and the gendered division of work.
There is evidence that family care negatively affects the caregiver's quality of life, with an impact on both physical and psychological health.3 The stress produced by caregiving can lead to physical and emotional problems, and even death.4 The responsibility of care is also linked to a deterioration in self-perceived health, pain, depression.5 Caring for others also affects other aspects of life, undermining personal development and opportunities to enjoy leisure time and a social life.6 These health effects are due to the conditions under which care is given, rather the care itself, and are likely modulated by the amount of time devoted to caregiving,7,8 the type of activities carried out,9 social support,10 and formal and informal networks to complement care activities.7,11 In addition, cultural norms and motivation to provide care could also influence the burden.12 Family care is assumed according to a social hierarchy that is related to gender and socioeconomic level. Informal care is distributed in families according to gender, age, relationship, and cohabitation status. Thus, caregivers are usually women aged ≥50 years who are the mother, daughter or wife of the care-receiver, who live in the same home as the care-receiver, and who are not in paid employment.13,14 Due to its unequal social distribution, caregiving is a determinant of health inequalities.8
Spain has one of the highest proportions of elderly people of all OECD countries, with 17.6% of the population aged >65 years. In 2008, there were 3,850,000 people with functional diversity (8.5% of the population), of which more than half were in a situation of dependence, i.e. needing personal assistance to carry out activities of daily living.15 The Dependency Law passed in 2006 (Ley 39/2006 2006; LAPAD, from its acronym in Spanish) was an important turning point because it introduced the notion that all citizens have a right to be cared, and that the State is obliged to provide care for people in situations of dependence. LAPAD contemplates social benefits in the form of services and economic compensation when a person is cared by family members. Reports and studies of LAPAD have highlighted budget difficulties since its implementation,16 with the most important reductions in July 2012 due to budget cuts in the context of government austerity policies.17 Some authors have argued that LAPAD does not sufficiently integrate all the perspectives of the various actors involved, and that this could reinforce care-related social inequalities.1,12,18 To date, studies analysing the impact of LAPAD have mainly focused on the economic aspects, and on satisfaction among people in situations of dependence.16 To our knowledge, no population-level studies have examined the influence of LAPAD on caregivers’ health and health inequalities with respect to non-caregivers.
The aim of this paper is to analyse time trends in health inequities due to caregiving for elderly people or those in situations of dependence in the context of LAPAD, taking gender and caregiver status into account.
MethodsDesign, information source and study populationWe performed a study of time trends using two cross-sectional samples based on data from the 2006 and 2012 editions of the Spanish National Health Survey (acronym in Spanish: ENS), which were conducted before and after introduction of LAPAD, respectively. The study population consisted of all non-institutionalised persons aged ≥16 years who were living in Spain in the year of the survey.
Study sampleA stratified multistage sampling was applied for both surveys, the first, second and third-stage units being census tracts, main family dwellings, and individuals, respectively. Individuals who declared severe chronic limitation to their activity due to a health problem in the previous 6 months (5.3% of samples in 2006 and 4.3% in 2012) were excluded from the analyses to avoid reverse causality due to their inability to be caregiver. The final sample obtained consisted of 27,922 persons in 2006 and 19,995 in 2012.19
Variables- 1)
Health outcomes
The following health indicators were used as the main dependent variables:
- –
Self-rated general health status: using the question “Within the last 12 months, would you say your health was very good, good, fair, bad or very bad?”, we created a dichotomous outcome variable expressed as good (“very good” or “good”) or poor (“fair”, “bad” or “very bad”) health.20
- –
Mental health: assessed using the 12-item version of the General Health Questionnaire (GHQ-12) with questions referring to the previous weeks and categorizing three or more points as indicating poor mental health.21
- –
Lower back pain: assessed using the question “During the last 12 months, have you suffered from lower back pain?” (yes/no).
- –
Use of psychotropic drugs: assessed using the question “during the past two weeks, have you used tranquilizers, anxiolytics, sleeping pills, antidepressants and/or stimulants?” (yes/no).
- –
- 2)
Main independent variable
To identify caregivers, ENS 2006 used the following questions: “Is there anyone in your home older than 74 who needs care? If yes, who mainly takes care of this person?”; and “Is there anyone in your home who is disabled or has limitations, and who needs care? If yes, who mainly takes care of this person?”. ENS 2012 used one question: “Is there anyone in your home that, due to any limitation or disability, is unable take care of themselves and needs someone to take care of them? If yes, who generally spends more time caring for this person?”. We assume that the question used in 2012 was broad enough to identify the same caregivers as the two questions used in 2006. Consequently, we considered caregivers to be those who identified themselves as someone cohabiting with one person in need of care, and who mainly undertook this responsibility according to any of the previous questions. Samples were categorized in three groups according to caregiver status: those who were not cohabiting with someone needing care or were not responsible for their care (non-caregivers), those who provided care and shared this responsibility with other persons (sharing care), and finally those who provided care alone (lone carers).
- 3)
Other independent variables
Other covariables used in the analysis were: age (15-44, 45-64, ≥65 years); highest level of education completed (no education, primary, secondary, university); social class, based on the current or last occupation of the person, or the head of the household in the case of never-employed respondents, categorized according to the Spanish Society of Epidemiology's proposal (social class I-II: professionals, managers, directors; social class III: administrative workers, clerks, safety/security workers and self-employed individuals; social class IV: skilled and semi-skilled manual occupations; social class V: unskilled manual occupations),22 employment status (working, unemployed, homemaker, retired, other), marital status (single, married, other), urban or rural setting (urban: living in a municipality with >20,000 inhabitants), social support (assessed using the Duke-UNC functional Social Support Questionnaire, considering scores below the 15% percentile as indicating poor social support)23 and household size (2 or >2 persons).
All analyses were conducted separately for men and women, and were adjusted for sampling weights. Analyses were performed using the STATA statistical package, version 13.
We first described socio-demographic characteristics and age-standardized proportions of health indicators stratified by caregiver status, sex and survey year. For standardization, we used the direct method, taking the lone carers group in ENS-2006 as the reference group. We fit robust Poisson regression models to obtain prevalence ratios (PR) with 95% confidence interval for health outcomes of caregivers who shared care and lone carers with respect to non-caregivers, adjusting for age and then sequentially adding educational level, household size, employment status and social support as explanatory factors. Finally, household size, employment status and social support did not substantially modify the association between caregiving status and health outcomes, either individually or through multiplicative interaction, so we report only the results for models adjusted for age and educational level.
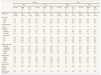
ResultsThe proportion of caregivers decreased slightly between 2006 and 2012; however, there were only minor changes in their socio-demographic characteristics. In both surveys, the largest group of caregivers was that of women who provided care alone (Table 1).
Socioeconomic description of the study population by distribution of care, sex and year of the survey. Residents in Spain aged 16 or more.
| Women | Men | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2012 | 2006 | 2012 | |||||||||
| No care | Share care | Care alone | No care | Share care | Care alone | No care | Share care | Care alone | No care | Share care | Care alone | |
| % | % | % | % | % | % | % | % | % | % | % | % | |
| Total (n, %)a | 13385 (94.3%) | 229 (1.6%) | 585 (4.1%) | 9739 (95.9%) | 144 (1.4%) | 275 (2.7%) | 13381 (97.5%) | 196 (1.4%) | 146 (1.1%) | 9615 (97.7%) | 148 (1.5%) | 74 (0.8%) |
| Age (years) | ||||||||||||
| 16-44 | 53.1 | 23.7 | 19.8 | 49.1 | 37.7 | 21.3 | 56.5 | 21.4 | 15.1 | 52.3 | 40.7 | 18.4 |
| 45-64 | 27.5 | 42.9 | 42.0 | 30.2 | 34.8 | 49.9 | 28.2 | 42.4 | 29.3 | 30.9 | 35.6 | 33.2 |
| ≥65 | 19.4 | 33.4 | 38.2 | 20.7 | 27.5 | 28.9 | 15.3 | 36.2 | 55.6 | 16.9 | 23.6 | 48.4 |
| Educational level | ||||||||||||
| No education | 11.6 | 24.2 | 24.3 | 11.8 | 22.3 | 18.3 | 8.1 | 16.7 | 24.2 | 9.1 | 15.2 | 22.7 |
| Primary | 49.6 | 49.8 | 57.9 | 51.2 | 56.0 | 61.8 | 49.0 | 57.3 | 51.2 | 55.2 | 57.5 | 45.7 |
| Secondary | 21.7 | 15.7 | 11.9 | 19.7 | 9.9 | 12.1 | 24.4 | 12.1 | 16.8 | 20.2 | 9.5 | 15.4 |
| University | 17.2 | 10.3 | 5.9 | 17.4 | 11.8 | 7.8 | 18.6 | 13.8 | 7.8 | 15.5 | 17.8 | 16.3 |
| Social class | ||||||||||||
| I-II | 19.4 | 16.7 | 13.0 | 18.4 | 11.0 | 14.8 | 21.1 | 14.4 | 14.8 | 19.1 | 14.8 | 9.8 |
| III | 22.9 | 20.9 | 28.9 | 19.5 | 18.8 | 18.7 | 23.7 | 25.5 | 21.4 | 17.1 | 20.8 | 21.6 |
| IV | 41.3 | 44.9 | 35.3 | 45.3 | 57.8 | 52.0 | 40.9 | 43.6 | 42.3 | 50.5 | 49.3 | 46.3 |
| V | 13.7 | 14.7 | 18.1 | 16.8 | 12.4 | 14.6 | 12.6 | 16.1 | 18.7 | 13.3 | 15.2 | 22.4 |
| Employment status | ||||||||||||
| Working | 43.2 | 36.3 | 20.3 | 41.4 | 27.7 | 29.6 | 64.7 | 42.2 | 18.9 | 51.9 | 38.7 | 17.6 |
| Unemployed | 8.0 | 5.7 | 8.6 | 12.3 | 15.7 | 12.8 | 6.3 | 10.2 | 5.6 | 16.9 | 20.0 | 13.4 |
| Homemaker | 24.9 | 29.9 | 41.9 | 19.0 | 30.8 | 30.9 | 0.1 | 1.0 | 1.6 | 0.7 | 0.8 | 1.1 |
| Retired | 15.8 | 26.0 | 27.0 | 18.8 | 24.4 | 25.0 | 20.5 | 46.2 | 71.0 | 22.0 | 30.3 | 60.5 |
| Other | 8.2 | 2.2 | 2.2 | 8.5 | 1.4 | 1.8 | 8.5 | 0.4 | 2.9 | 8.5 | 10.1 | 7.4 |
| Marital status | ||||||||||||
| Single | 28.0 | 18.5 | 16.8 | 29.3 | 26.4 | 18.5 | 37.7 | 27.5 | 25.8 | 35.2 | 31.8 | 31.8 |
| Married | 57.2 | 71.3 | 65.8 | 54.0 | 61.1 | 65.8 | 56.3 | 68.1 | 56.6 | 58.4 | 58.5 | 59.5 |
| Other | 14.8 | 10.2 | 17.4 | 16.6 | 12.5 | 15.6 | 6.0 | 4.4 | 17.6 | 6.4 | 9.8 | 8.7 |
| Low social support (P15) | 13.6 | 18.8 | 24.3 | 12.2 | 13.2 | 25.9 | 14.4 | 18.8 | 32.5 | 13.0 | 14.4 | 29.4 |
| Area of residence (urban) | 67.8 | 62,3 | 59,7 | 68,7 | 58,5 | 70,3 | 68,3 | 63,1 | 68,0 | 68,0 | 70,6 | 64,3 |
| Household size (>2 persons) | 68.0 | 85.2 | 64.1 | 59.5 | 87.8 | 61.4 | 70.8 | 84.0 | 29.0 | 64.6 | 89.7 | 26.6 |
Caregivers who give care alone were generally older than non-caregivers and the differences were greater among men. In both surveys and for both sexes, caregivers were less generally well educated and more likely to belong to more disadvantaged social classes (IV and V) than non-caregivers.
We observed a change in employment status between the surveys, with a generalized increase in unemployment in 2012. Those who provided care alone were more likely to be homemakers or retired (women and men, respectively) than non-caregivers, with differences decreasing in 2012. The percentage of women lone caregivers who were in paid employment increased in 2012, and was also greater (29.6%) than for women who shared caregiving (27.7%), but was still lower than that among non-caregivers (41.4%). In both editions of the survey, caregivers were more likely to be married and to live in urban areas. Caregivers were more likely to have poor social support, especially among men who provided care alone, with all proportions decreased in 2012 with respect to 2006, except for women who provided care alone.
In both surveys, men tended to present better health indicators than women. Between 2006 and 2012, women showed a decrease in the age-standardized proportion of illness for all four health indicators (Fig. 1). Only the proportion of lower back pain increased slightly among those who provided care alone (39.1% to 42.0%). The decrease in poor health was more pronounced among women who shared caregiving, in whom self-rated poor health decreased from 61.0% in 2006 to 42.3% in 2012, poor mental health decreased from 44.2% to 29.5%, and the use of psychotropic drugs decreased from 32.2% to 21.2%. The decrease in poor health indicators were less remarkable among men, except for self-rated poor health in lone carers, which decreased from 59.1% to 42.3%. Notably, we observed an increase in the proportion of poor mental health among men who were non-caregivers (14.2% in 2006, 16.7% in 2012) and those who shared caregiving (21.7% to 27.1%), but a decrease among men who were lone caregivers (from 29.4% to 27.3%).
In 2006, the likelihood of poor self-rated health was higher among caregiving than non-caregiving women (PR=1.29 and 1.19 for those giving shared and lone care, respectively) (Fig. 2). In 2012, this gap disappeared among those giving shared care (PR=0.89) but increased among lone caregivers (PR=1.26). The greatest difference between caregiving and non-caregiving women in 2006 was in the proportion of poor mental health (PR=1.69 and 1.51 for those giving shared and lone care, respectively). These differences decreased considerably in 2012 among individuals providing shared care (PR=1.04), but not among lone carers (PR=1.54). According to the adjusted models, the other health indicators, lower back pain and use of psychotropic drugs, followed the same pattern. In both surveys, men lone carers showed a higher probability of poor health than other groups, except in terms of the use of psychotropic drugs. The only significant differences in the 2006 survey were between lone carers and non-caregivers for poor self-rated health (PR=1.43) and poor mental health (PR=2.00). All inequalities tended to decrease for both groups of caregivers in the 2012 survey, and none of were statistically significant.
Multivariate-adjusted Prevalence Ratio (PR) and 95% confidence interval for health outcomes for persons who share the care and persons who care alone with respect to persons who don’t care by sex and survey of year. Residents in Spain aged 16 or more. PR are adjusted by age and educational level. PR=1 No caregiving. WOMEN 3.0.
This study shows that the social profile of caregivers in Spain has remained largely unchanged in recent years, and caregiving continues to be linked to gender and social class. Between 2006 and 2012, there was a decrease in health inequalities between individuals providing shared care and non-caregivers, and an increase in inequalities among the largest group of caregivers, women who provide care alone.
Our results show that caregiving is mostly undertaking by women, with similar percentages to those from previous studies in our context.8,9,13 Also consistent with these studies, caregiving women and men generally tend to have a low educational level. These data indicate the persistence of social inequalities in the system of informal care.
Stratifying our analysis by gender allow us to interpret the poorer health indicators among caregiving women than caregiving men in a gender based framework. Differences between caregiving men and women could be explained in terms not only of the higher proportion of women, but also of the types of tasks and time devoted to caregiving, which disrupt women's daily life much more than that of men, thus affecting their health.14 Women more often care for psychological and physical needs, such as assistance with personal hygiene, in contrast to men who have a greater tendency to perform activities in the public sphere.9 Previous research also shows that men faced with a highly demanding caregiving situation are more likely to seek external support, thus experiencing lower stress levels than women.24
In contrast with previous studies,10 we found that social support does not appear to be a main modulator of the burden of care and health problems. One explanation for this could be the fact that we stratified our analysis according to whether care was shared or undertaken alone, where shared care partly accounts for this support.
The difference in time trends in heath inequalities between the two groups of caregiving women may be due to differences in how they use the economic compensation offered for providing care at home. This economic benefit becomes the rule, 54% of the total benefits in 2012, and 93% of the caregivers who received it were women.25 As some authors have suggested,18 the economic benefit for women who provide care alone may condemn them to take a role that excludes them socially. Literature shows that economic benefits in Mediterranean countries may allow families to hire non-professional caregivers,26 many of whom are immigrant women.27,28 This situation may reduce the burden of care on those who share caregiving, as they feel accompanied and relieved.12,29 Receiving help from someone outside the family is associated not only with a reduced burden, but also with a less negative reaction to care,30 which may also explain the health improvement, but maybe moving health inequalities to inmigrant caregivers. Notably, the decrease in mental health inequalities in men is also due to the increased prevalence of poor mental health in non-caregiving men. This is consistent with previous analyses of the same surveys, which showed that the prevalence of poor mental health has increased among men during the economic crisis, especially among middle-aged male main-earners due to their change in employment status.31 The economic crisis in Spain has affected mental health more than other health indicators, such as self-rated health or all-cause mortality.32,33
Limitations and strengthsThis study has some limitations. First, we were not able to determine whether people in situations of dependence receive benefit from LAPAD, nor the severity of their situation. However, LAPAD has been implemented gradually, with an initial focus on situations of greater dependence. Thus, caregivers with a greater burden and a greater health impact should have been the first to receive some kind of benefit.
We only accounted for caregivers who live with the care-receiver, and therefore a part of the caregiver population is lost. However, this group represents the majority of caregivers, and is the one that bears most of the burden and health consequences of caring.12
The two ENS editions surveys used different questions to identify caregivers. Changes in the surveys could explain the decrease in the number of caregivers in 2012, so we do not interpret this as an effect of LAPAD.
Finally, implementation of the Law has faced significant budget difficulties. Nonetheless, the most drastic budget cuts probably did not affect the 2012 edition of the survey because the data were collected before they took place.
This is the first study to analyse time trends in health inequalities associated with caring for people in situations of dependence in the context of the Spanish Law of Dependency. One strength of this study is that it provides quantitative information at the population level, with quite consistent findings across a range of reliable health indicators, including self-rated health, which reflects a global evaluation of disease, symptoms, functional abilities and overall well-being,34 chronic back pain, a very frequent affliction among caregivers,35 and mental health evaluated using both a standardised questionnaire, and in terms of current use of psychotropic drugs.
Another strength is that we have been able to distinguish between caregivers according to whether they share the responsibility of care, which reveals the most affected groups and a difference in time trends. This helps to discover the mechanisms through which the LAPAD and other contextual factors may influence health inequalities according to how care is provided.
ConclusionsAccording to our results, the general structure of the care model, characterised by gender and class division, remains largely unaltered. We observed different trends according to gender and care-sharing, with the health of women who provide care alone remaining the most markedly affected by caregiving.
Based on the findings of the current study, we believe that it is necessary to redesign and implement policies to reduce inequalities related to caregiving that take into account the most affected groups, such as female lone caregivers. It is important to improve the implementation of LAPAD, and in parallel to invest in new solutions that promote a fairer social distribution of care.
Care for people in situation of dependence is a determinant of health inequalities. In 2006, in Spain, the Dependency Law introduced the universal right to public benefits in a in a context of scarce development of welfare policies for caregiving.
What does this study add to the literature?In the Law's context, health inequalities due to care diminished especially for those who shared the care. However, health inequalities remained for lone caring women, the largest caregivers’ group. Dependency Law needs to be improved to reduce health inequalities in groups that could be more affected. Besides this enhancement, it is required to promote a fairer social distribution of care.
M.a Felicitas Domínguez Berjón.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsM. Salvador-Piedrafita, D. Malmusi and C. Borrell were involved in the conception and design of the work, carried out the analysis and interpretation of data. The first version of the manuscript was written by M. Salvador-Piedrafita and was subsequently improved by all authors, with important intellectual contributions. All authors have approved the final version and are jointly responsible for adequate revision and discussion of all aspects included in the manuscript.
FundingThis research was partially supported by the European Community's Seventh Framework Programme (FP7/2007-2013, grant agreement number 278173): Evaluating the impact of structural policies on health inequalities and their social determinants and fostering change (Sophie) project.
Conflicts of interestC. Borrell belongs to the Gaceta Sanitaria editorial committee, but was not involved in the editorial process of the manuscript.
The authors thank Mercè Gotsens for collaborating in the analysis and Sophie participants for their contributions at project meetings.