The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosThe quality of health services has long received global attention. Consequently, safe and quality health services in hospitals have become the main hopes and goals of the community, health workers, managers, owners, and regulators. A common external strategy used globally involves recognizing the applied quality management system, specifically certification and accreditation.
ObjectiveTherefore, the purpose of this study is to determine the relationship between levels of quality perception and accreditation in hospitals based on several variables.
MethodsA total of 13 hospitals were examined in this cross-sectional study, while a questionnaire consisting of 24 validated items was used for data collection. Subsequently, the analysis was performed by utilizing descriptive statistics and chi-square techniques.
ResultsFrom the results obtained, the patient assessment, drug use management, patient and family education, infection prevention and control, alongside facility management and safety variables, had a relationship with the level of hospital accreditation, while patient service did not.
ConclusionsTherefore, each hospital is expected to improve its service quality and accreditation.
One of the external strategies commonly used in the world is the recognition of the applied quality management system, particularly certification and accreditation. Accreditation is a management concept and method, which helps hospitals gain a competitive advantage and subsequently develop by considering sustainable environmental changes. According to the World Health Organization (WHO), this concept can be the single most important way to improve the quality of health care institutions.1 Furthermore, hospital accreditation systems are used in many countries, as they are believed by the provider to be persuasive, improve quality, and help employees organize and strengthen patient safety.2
Accreditation is an external review process designed to evaluate employee performance based on established standards. Specially trained external teams also conduct announced surveys to assess compliance with these standards.2 Currently, international accreditation organizations require an assessment of patient safety culture to identify the inherent strengths and weaknesses, alongside evaluate staff teamwork. They also observe management and leadership capabilities, the frequency of incident reporting, and existing patient safety culture issues.3
The Ministry of Health appreciates hospitals’ achievement of providing an accreditation certificate through the independent agency, Hospital Accreditation Committee (KARS). Meanwhile, the process involved in determining this final decision is based on the hospital's ability to meet the 2017 National Hospital Accreditation Standards (SNARS).4 Hospital managers and leaders attach great importance to the need for accreditation to ensure customers are satisfied with the service quality provided. Various studies have shown a clear result, which is that the major advantage of implementing accreditation is based on criteria that can standardize certain characteristic.5
Hence, this study aims to determine the relationship between the quality perception and accreditation level of hospitals based on several variables. These accreditation variables include patient assessment and care, drug use management, patient and family education, infection prevention and control, as well as facilities management and safety.
MethodologyStudy designThis quantitative study used a cross-sectional approach and was performed in hospitals with the 2012 KARS Basic, Intermediate, Main, and Plenary 2012 accreditation status in Makassar City in 2018 for one year. The locations involved thirteen public hospitals in this city, including Dr. Wahidin Sudirohusodo, Makassar Hasanuddin University, Awal Bros Makassar, Stella Maris, Pelamonia Lv II, Makassar City, and Haji Regional General Hospitals. The others were RSUD in South Sulawesi Province, Jaury Academic, Faisal Islamic, Bhayangkara, University of East Indonesia Wisata, South Sulawesi Labuang Baji, and Mitra Husada Hospitals. Meanwhile, the sample determination was adjusted to accommodate the total employees in the concerned hospitals, and this population encompassed medical personnel, paramedics, and support staff, including doctors, nurses, and pharmacists. This sample was taken by researchers through a proportional random sampling method of about 1873 samples.
InstrumentThe questionnaire involved 24 items in six dimensions, which included patient assessment document, patient care, drug use management, comprising four items each. Meanwhile, the other dimensions were patient and family education, with two, alongside infection prevention and control, as well as facilities management and safety, involving five items each. The respondents were asked to answer each item using a two-point Likert scale ranging from ‘bad’ to ‘good.’ Then, the categorization scores were computed based on the mean value, where outcomes equal to or greater than this value was included in the ‘good’ category, while lower results were placed in the ‘bad’ group.
Data analysisThis study used descriptive statistics and chi-square to determine the independent variable's effect on the dependent parameter.
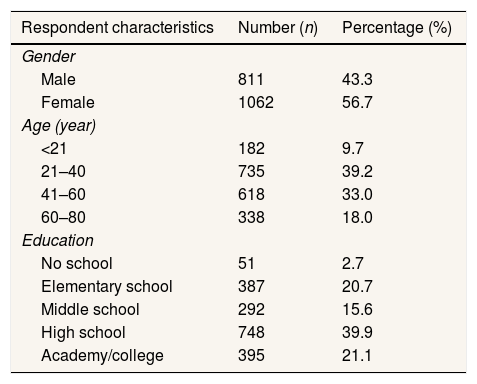
Finding and discussionCharacteristics of the sampleAs shown in Table 1, there were 1062 female respondents and 811 males based on gender, which accounted for 56.7% and 43.3%, respectively. Additionally, 735 persons were aged between 21 to 40 years, while the group with the lowest number was <21 years, comprising 182 respondents, at 39.2% and 9.7%, consecutively. Based on education, the majority, at 748 persons or 39.9%, were Senior High School students or at equivalent levels, while 51 respondents had no education and made up the least proportion at 2.7%.
Respondent characteristics.
| Respondent characteristics | Number (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 811 | 43.3 |
| Female | 1062 | 56.7 |
| Age (year) | ||
| <21 | 182 | 9.7 |
| 21–40 | 735 | 39.2 |
| 41–60 | 618 | 33.0 |
| 60–80 | 338 | 18.0 |
| Education | ||
| No school | 51 | 2.7 |
| Elementary school | 387 | 20.7 |
| Middle school | 292 | 15.6 |
| High school | 748 | 39.9 |
| Academy/college | 395 | 21.1 |
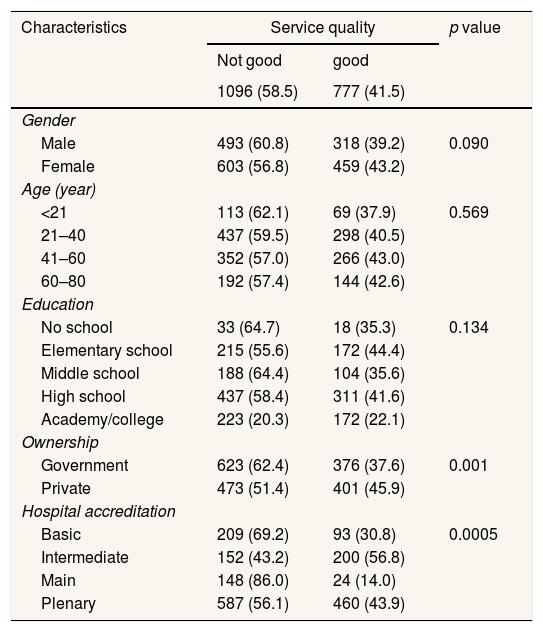
The analysis of the relationship between the respondent characteristics and the perceptions of service quality presented in Table 2 showed that 318 males and 459 females, which accounted for 39.2% and 43.2% of the participants, stated that the service quality was good. Based on age, this group was dominated by 266 respondents between 41 and 60 years old, while the least was 69 persons aged <21, and both categories constituted 43.0% and 37.9%, respectively. The education of those with this response was majorly at the elementary level, while the academy/college group had the lowest proportion, at 172 respondents each, or 44.4% and 22.1%, respectively. Consequently, the chi-square test results for the gender, age, and education level variables gave p-values of 0.090, 0.569, and 0.134, respectively, and hence, had no relationship with the perception of service quality.
The relationship between respondent characteristics and service quality perceptions.
| Characteristics | Service quality | p value | |
|---|---|---|---|
| Not good | good | ||
| 1096 (58.5) | 777 (41.5) | ||
| Gender | |||
| Male | 493 (60.8) | 318 (39.2) | 0.090 |
| Female | 603 (56.8) | 459 (43.2) | |
| Age (year) | |||
| <21 | 113 (62.1) | 69 (37.9) | 0.569 |
| 21–40 | 437 (59.5) | 298 (40.5) | |
| 41–60 | 352 (57.0) | 266 (43.0) | |
| 60–80 | 192 (57.4) | 144 (42.6) | |
| Education | |||
| No school | 33 (64.7) | 18 (35.3) | 0.134 |
| Elementary school | 215 (55.6) | 172 (44.4) | |
| Middle school | 188 (64.4) | 104 (35.6) | |
| High school | 437 (58.4) | 311 (41.6) | |
| Academy/college | 223 (20.3) | 172 (22.1) | |
| Ownership | |||
| Government | 623 (62.4) | 376 (37.6) | 0.001 |
| Private | 473 (51.4) | 401 (45.9) | |
| Hospital accreditation | |||
| Basic | 209 (69.2) | 93 (30.8) | 0.0005 |
| Intermediate | 152 (43.2) | 200 (56.8) | |
| Main | 148 (86.0) | 24 (14.0) | |
| Plenary | 587 (56.1) | 460 (43.9) | |
Based on hospital ownership, 376 respondents in government settings and 401 persons from private hospitals, both of which made up 37.6% and 45.9%, respectively, stated that the quality was good. Meanwhile, the majority of these persons, specifically 200 respondents, which constituted 56.8%, confirmed that the perception at the intermediate accreditation level was good, while only 24 persons, or 14.0%, agreed at the main level. The chi-square test results for the respondents’ characteristics on the variables of hospital ownership (p=0.001) and accreditation (p=0.0005) proved that a relationship with service quality perceptions exists (Table 2).
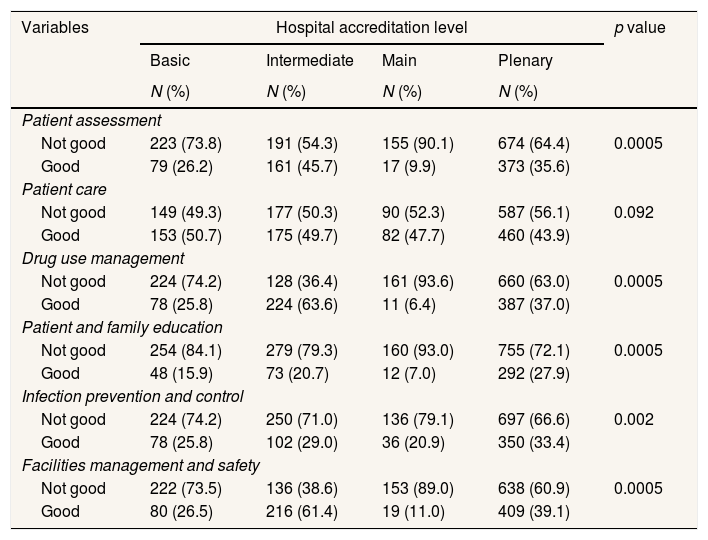
The relationship between perceptions of quality and the level of hospital accreditation based on the SNARS variable.
Table 3 shows the relationship between perceived quality and the accreditation level of hospitals based on the SNARS variable. For patient assessment, 161 respondents stated that the service quality perception was good at the intermediate accreditation level, while 17 persons constituted the lowest proportion and supported the main level, with each making up 45.7% and 9.9%, respectively. Regarding patient service, 153 respondents at the basic level and 460 persons from the plenary level made up the majority and minority of the supporters, respectively, with each group comprising 50.7% and 43.9%. Meanwhile, concerning the drug use management variable, the highest supporting number was from the intermediate accreditation level, totaling 224 persons, while the least was 11 from the main level, at 63.6% and 6.4%, respectively.
Correlation of the perceptions of quality based on several variables with the accreditation level.
| Variables | Hospital accreditation level | p value | |||
|---|---|---|---|---|---|
| Basic | Intermediate | Main | Plenary | ||
| N (%) | N (%) | N (%) | N (%) | ||
| Patient assessment | |||||
| Not good | 223 (73.8) | 191 (54.3) | 155 (90.1) | 674 (64.4) | 0.0005 |
| Good | 79 (26.2) | 161 (45.7) | 17 (9.9) | 373 (35.6) | |
| Patient care | |||||
| Not good | 149 (49.3) | 177 (50.3) | 90 (52.3) | 587 (56.1) | 0.092 |
| Good | 153 (50.7) | 175 (49.7) | 82 (47.7) | 460 (43.9) | |
| Drug use management | |||||
| Not good | 224 (74.2) | 128 (36.4) | 161 (93.6) | 660 (63.0) | 0.0005 |
| Good | 78 (25.8) | 224 (63.6) | 11 (6.4) | 387 (37.0) | |
| Patient and family education | |||||
| Not good | 254 (84.1) | 279 (79.3) | 160 (93.0) | 755 (72.1) | 0.0005 |
| Good | 48 (15.9) | 73 (20.7) | 12 (7.0) | 292 (27.9) | |
| Infection prevention and control | |||||
| Not good | 224 (74.2) | 250 (71.0) | 136 (79.1) | 697 (66.6) | 0.002 |
| Good | 78 (25.8) | 102 (29.0) | 36 (20.9) | 350 (33.4) | |
| Facilities management and safety | |||||
| Not good | 222 (73.5) | 136 (38.6) | 153 (89.0) | 638 (60.9) | 0.0005 |
| Good | 80 (26.5) | 216 (61.4) | 19 (11.0) | 409 (39.1) | |
Based on the patient and family education variables, the plenary accreditation level had the most respondents, at 292 persons, agreeing that the perception of service quality was good, while the least was 12 at the main level, comprising 27.9% and 7.0%, respectively. In the infection prevention and control variable, the majority and least of supporting respondents were 350 and 36 persons from the plenary and main accreditation levels, respectively, with each comprising 33.4% and 20.9%. Finally, the facility management and safety variables had the highest and lowest number of respondents from the intermediate and main accreditation levels at 216 and 19 persons, which accounted for 61.4% and 11.0%, respectively. The chi-square test results showed that five of the variables had a relationship with the hospital accreditation level. These were patient assessment (p=0.0005), drug use management (p=0.0005), patient and family education (p=0.0005), infection prevention and control (p=0.002), alongside facility management and safety (p=0.0005). However, as shown in Table 3, the patient care variable (p=0.092) had no relationship with the parameter.
DiscussionHospital accreditation is a standard compliance assessment process performed by independent institutions at home and abroad. Accredited hospitals receive recognition from the government because they fulfill service and management standards.6 Therefore, the assessment employed in this research uses the national hospital accreditation standards made by the Hospital Accreditation Committee (KARS). Several study variables were adopted from the KARS instrument and compared to hospital accreditation levels.7 These variables were patient assessment, patient care, drug use management, patient and family education, infection prevention and control, alongside facility management and safety.
The quality of health services provided is necessary to fulfill customer expectations and patient needs, as well as improve the services offered by health care professionals.8 According to Donabedian,9 this quality refers to the application of medical science and technology in a way that maximizes health benefits and decreases risks.
Subsequently, this study discovered that hospital accreditation has a significant relationship with the perception of service quality at a p-value=0.0005, <0.05. This result corresponds with the study by Avia and Hariyati,6 which found that hospital accreditation has a positive impact on enhancing the quality of provided services by improving management, employee participation, and results. A study in Romania also discovered that hospital accreditation plays a positive role in improving health service quality, patient satisfaction, and institutional reputation.10
Meanwhile, Hapsari and Sjaaf3 stated that accredited hospitals have a much higher perception of facility management, patient safety, and incident reporting frequency than their non-accredited counterparts. Respondents from these hospitals are more likely to report incidents, have an increased perception of patient safety, and feel that their service quality improved with accreditation.3
Furthermore, this research found that the perception of good service quality was higher in private hospitals at a percentage of 45.9% than government hospitals at 37.6%. This result corresponds with a study in Saudi Arabia comparing the service quality of private and government hospitals. According to the findings (t=3.390, p<0.01), private hospital patients experienced a higher level of health service quality 11. In contrast, literature review studies in Europe showed that government hospitals are more efficient than their private counterparts, and only patients with higher socioeconomic backgrounds have access to better private hospital services.12
Almost all the six quality variables, except patient care, demonstrated a relationship with the hospital's accreditation level. This study obtained a p-value of 0.092, >0.05 for this variable, demonstrating the absence of a significant relationship with the level of hospital accreditation. However, this result was different from the outcomes obtained by Algahtani,13 which stated that accreditation allows increased patient care. It also revealed that it positively impacts the process and implementation of changes in hospitals that result in improvements in patient care and other health services.13 Furthermore, Trisno et al.14 stated that hospital accreditation increases nurses’ perceptions of service quality, which is one of its impacts. Consequently, nurses in accredited hospitals experience a higher quality of health care.14
The drug use management variable also exhibited a relationship with the hospital accreditation level. Meanwhile, the 2012 Indonesian KARS version of hospital accreditation calls for the application of drug use management (MPO) standards, which aim at patient safety. A part of these standards is the implementation of proper drug administration as an important component in the palliative, symptomatic, preventive, and curative treatment of various diseases and conditions. MPO components include the systems and processes used by the hospital in providing pharmacotherapy to patients. This is a multidisciplinary and coordinated effort of hospital staff in applying the principles of effective process design and implementation. It also entails the enhancement of selection, procurement, storage, ordering or prescription, recording of transcripts, drug distribution, preparation, dispensing, administration, documentation, and monitoring of drug therapy. Although the role of health care providers in the implementation of correct drug administration varies widely from one country to another, good management processes for patient safety are universal.7 Hence, accreditation status is an acknowledgment that the hospital has fulfilled the standards, including the MPO, at a fully or plenary accredited hospital. The high incidence of patient safety in several reports in Indonesia indicates a weak relationship with accreditation status.
Additionally, Putro et al.15 stated that the implementation level of correct drug administration in hospitals with prime accreditation status is slightly higher than those with complete status, according to both nurses and patients, and only a few nurses occasionally performed wrongly. Hospitals with prime accreditation show that better implementation of correct drug administration is associated with a lower perception of patient safety incidents. However, there was no relationship with complete accreditation status and no difference in the level of accuracy when administering drugs.15
Other research results also suggest a relationship between the accreditation level and perception of quality based on patient and family education variables. This deduction was supported by a study concerning the form of education at Pelamonia Lv. II Hospital, Makassar. It was employed to directly enlighten patients and their families and encourage them to play active roles during the treatment process. Necessary instructional materials were also supplied by distributing brochures and leaflets and providing communication media, such as TVs displayed in front of the patient's waiting room and each treatment room.16
Patients and family members have the right to receive appropriate education to make sure that the acquired knowledge can be used to participate in their care process and make informed decisions. This includes identifying the patient or family's educational needs, formulating a personalized plan, providing appropriate education, evaluating the effectiveness of the learning process, and safeguarding patient rights. Also, hospitals are required to have sufficient resources, including but not limited to personnel, premises, and educational materials, to ensure proper education for the patients and their families. As healthcare growth in many countries continues to outpace inflation, policymakers are increasingly focused on controlling costs. Consequently, cost control studies have shown that patient education can save a lot of money and assist them in maintaining better health with fewer complications. Hence, they would require fewer hospitalizations, emergency visits, clinics, and doctor visits.1
The perception of quality is also based on the infection prevention and control variable, which has a relationship with the hospital accreditation level. This finding corresponds with a study at a private hospital in Yogyakarta, which showed that the Infection Prevention and Control (IPC) program has not yet reached the target based on SNARS Edition I. The facilities provided by the hospital were inadequate, as seen from the unavailability of infrastructure in several units, especially those handling numerous infections, where there was incomplete equipment to support the work of the IPC Team. Apparently, the 2018 IPC Team's work program had not been agreed upon and submitted to the Director. The recording and reporting of infection surveillance, alongside the integrated Quality Improvement and Patient Safety (PMKP), was also yet to be executed. Consequently, the trend of Surgical Site Infection (SSI) cases increased quite significantly, in line with the definition of an extraordinary event (KLB), thus requiring further investigation. This hospital is currently undergoing the accreditation process, which is to be received in 2018 for the first time.17 Therefore, the level of accreditation certainly influences infection prevention and control programs.
The results also show that the perceptions of quality based on facility management and safety variables have a relationship with the level of hospital accreditation. This finding is supported by a study at the X Mother and Child Hospital in Semarang City, which found that although internal regulations related to facility management and safety were still lacking, it had made risk management efforts. Hence, risk management was implemented incidentally by this hospital, considering that there were also plans to apply for accreditation shortly.4 Therefore, the level of accreditation clearly has a relationship with the facility management and safety variables.
ConclusionsThe study show that respondent characteristics, such as gender, age, and education level have no relationship with the perceptions of service quality, while ownership and hospital accreditation variables exhibited positive results.
According to the results also, patient assessment, drug use management, patient and family education, infection prevention and control, facility management, and safety variables are related to the hospital accreditation level, while patient care is not.
RecommendationsEach hospital is expected to improve its service quality and accreditation.
Conflicts of interestsThe authors declare that they have no conflict of interest.
Funding sourcesNone.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.