The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosThe research aimed to determine the effect of breastfeeding on body temperature, body weight, and jaundice of 0–72h-old infants in Sitti Khadijah I Mother and Child Hospital of Makassar.
MethodThe research was an observational longitudinal design. The samples were breastfeeding mothers and 0–72h-old newborn infants consisting of 70 people selected using the purposive sampling method. The data were analyzed using the Chi-square test.
ResultThe result of the research indicated that there are 29 respondents (41.4%) giving exclusive breastfeeding with infants normal body temperature 29 people (100%), decreasing body weight 28 people (96.6%), and no jaundice 29 people (100%), while the respondents who do not give breastfeeding consist of 41 people (58.6%) with body temperature undergoing hyperthermia one respondent (2.4%), increasing body weight three people (7.3%) and jaundice four people (9.8%).
ConclusionThere is an effect of giving breastfeeding on body temperature (p=0.016), but there is no effect on body weight (p=0.168) and jaundice (p=0.083) of 0–72h-old infants.
Breastfeeding in the early days is highly recommended because it provides health benefits for both mother and baby. The benefits of breastfeeding immediately are for the baby's survival, immunity, preventing hypothermia, the sucking reflex of the mother's nipple, and releasing the hormone Oxytocin will stimulate milk production. The World Health Organization (WHO) states that breast milk (ASI) is the first food for infants. It is reported that 2/3 of under-five deaths occur in infancy, most of which are related to poor feeding practices. It is widely recognized that the role of immediate breastfeeding can reduce 22% of all neonatal deaths so that breastfeeding becomes a top priority for infants.1
Unicef and WHO is recommend exclusive breastfeeding for several months of life until the age of 6 months, after which the child should be given solid and semi-solid foods as other food in addition to breast milk. The WHO statement has not been fully implemented, it is proven that there are still babies aged 0 months getting food and drinks other than breast milk, as reported by the Basic Health Research (RIKESDAS) about the percentage of breastfeeding patterns in infants based on the 0 month age group, there are 39.8% who get exclusive breastfeeding. 55.1% were given water and honey, and 20% were given formula milk. The causes of failure in breastfeeding include working mothers, lack of knowledge of mothers, culture in society, and the proliferation of promoting formula milk.
RIKESDAS (2013), several causes of infant mortality are respiratory disorders 37%, prematurity 34%, sepsis 12%, hypothermia 7%, these events should be reduced by maximizing breastfeeding starting with Early Initiation Breastfeeding (IMD), especially premature infants, and hypothermia. This statement is proven by research,2 which shows an increase in body temperature in hypothermic infants after 1h of early breastfeeding initiation even though the baby has not been fully breastfed with an increase in temperature of 0.1–0.3°C.3
In addition to preventing hypothermia, breastfeeding is also associated with increased birth weight. Neonatal weight loss in the first days is often a concern for mothers. This is a process of physiological adjustment of the intrauterine environment's transition from the intrauterine environment. Usually, term neonates will experience a weight loss of about 5–10% of birth weight during the first week of life. Weight loss of more than 10% of birth weight indicates a problem with breastfeeding. Inadequate breastfeeding causes a lack of caloric intake, dehydration, decreased gastrointestinal motility. It is highly recommended that the baby be breastfed ten times in 24h during the first week of birth to compensate for this weight loss. Most babies gain the weight back to their birth weight in the first 10–14 days of life.
Based on the results of the study that immediate and exclusive breastfeeding for infants is highly recommended, if there is a delay in breastfeeding, it will have a harmful impact on the baby, which occurs where there are (62.2%) infants who are not breastfed with (32.4%) jaundice in the newborn baby at the Siti Fatimah Mother and Child Hospital in Makassar. Meanwhile, the incidence of jaundice in Indonesia in term infants in several teaching hospitals, including RSCM, Sardjito Hospital, Dr. Hospital. Soetomo, Dr. Hospital. Kariadi Semarang from 13.7% to 85%. Incidence of non-physiological jaundice at RSU Dr. Soetomo Surabaya 9.8% in 2002 and 15.66%.
The problem of low breastfeeding is reported that breastfeeding patterns in Indonesia at the provincial level show that breastfeeding is less than 1 hour after the baby is born, the highest in West Nusa Tenggara (52.9%) and the lowest in West Papua (21.7%) and breastfeeding >48 the highest hour was in the province of Central Sulawesi (26.4%). The lowest was in the province of West Nusa Tenggara (4.6%), while in South Sulawesi, breastfeeding was less than 1h (44.9%), but there were still breastfeeding >48h (15.1%). Most of the breastfeeding process is carried out in the range of 1–6h after the baby is born, but there are still 11.1% carried out after 48h.3
The number of infants who were exclusively breastfed in South Sulawesi in 2011 was (36.8%) in 2012 (63.7%) and increased in 2013 (67.8%). Based on the explanation above that RSIA Sitti Khadijah I Makassar the birth rate is relatively high (2243) with an average of 200 deliveries per month, so a study was conducted on the Effect of Breastfeeding on Body Temperature, Body Weight and Jaundice in Newborns aged 0–72h in RSIA Sitti Khadijah I Makassar City.
Materials and methodsThis research was conducted at the Mother and Child Hospital (RSIA) Sitti Khadijah I Makassar City. The type of research used is observational using the Longitudinal Observation design. The population was all normal newborns at RSIA Siti Hadijah I Makassar. A sample of 70 people was selected by purposive sampling who met the inclusion criteria, namely: Babies born with regular delivery, healthy babies, mothers being able to breastfeed, and willing to take part in this study by signing the informed consent issued by the Ethics Committee of the Faculty of Medicine Hasanuddin University. Data collection was done by direct observation and systematic recording of the object to be studied. Researchers carried out observations by observing and recording: Breastfeeding, which includes; The first time breastfeeding was given, measurement of the baby's body temperature, weighing the baby's weight, and assessing jaundice in the baby. The researcher then directly observed breastfeeding after the mother gave birth from 0 to 72h of delivery by using a checklist sheet (observation) and taking body temperature measurements, Bodyweight, and assessment jaundice at 0–24h, 24–48, and 48–72h. The analysis in the form of univariate and bivariate analysis is the analysis of the independent variables that are thought to have a relationship with the related variables. Analysis of the data used is the Chi-Square test. Through the Chi-Square test, a conclusion is then drawn; if the p-value <0.05, then Ha is accepted, indicating an influence between the dependent variable and the independent variable. Meanwhile, if the p value >0.05, then Ho is rejected, which indicates there is no effect between the dependent variable and the independent variable.
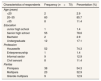
ResultThe results of this study are presented in the following tableBased on Table 1, the characteristics of the frequency of respondents in the age group of 70 respondents who gave breastfeeding were aged 20–35 years, namely 60 people (85.7%) and a small portion aged >35 years, namely 8 (11.4%). Most of them have a high school education. Namely, 55 people (78.6%) and a small part have bachelor education, namely two people (2.9%). Most of them work as housewives with 52 people (74.3%) and a small part as Civil Servants with eight people (11.4%). Most parity is Primipara. Namely, 38 people (53.3%) and a small proportion are Grandemultipara, nine people (12.9%) (Table 2).
Frequency distribution of respondents characteristics.
| Characteristics of respondents | Frequency (n=70) | Percentation (%) |
|---|---|---|
| Age (years) | ||
| <20 | 2 | 2.9 |
| 20–35 | 60 | 85.7 |
| >35 | 8 | 11.4 |
| Education | ||
| Junior high school | 1 | 1.4 |
| Senior high school | 55 | 78.6 |
| Bachelor | 2 | 2.9 |
| Undergraduate | 12 | 17.1 |
| Profession | ||
| Housewife | 52 | 74.3 |
| Enterpreneurship | 1 | 1.4 |
| Informal sector | 9 | 12.9 |
| Civil servant | 8 | 11.4 |
| Paritas | ||
| Primipara | 38 | 54.3 |
| Multipara | 23 | 32.9 |
| Grande multipara | 9 | 12.9 |
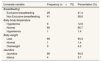
Distribution of respondents frequency based on breastfeeding, body temperature, body weight, and jaundice incidence in infants aged 0–72h.
| Univarate variable | Frequency (n=70) | Percentation (%) |
|---|---|---|
| Breastfeeding | ||
| Exclusive breastfeeding | 29 | 41.4 |
| Non Exclusive breastfeeding | 41 | 58.6 |
| Baby body temperature | ||
| Hypotermia | 9 | 12.9 |
| Normal | 60 | 85.7 |
| Hypertermia | 1 | 1.4 |
| Baby weight | ||
| Less | 66 | 94.3 |
| Normal | 1 | 1.4 |
| Overweight | 3 | 4.3 |
| Jaundice | ||
| Jaundice | 66 | 94.3 |
| Icterus | 4 | 5.7 |
Most breastfeeding did not provide exclusive breastfeeding; namely, 41 people (58.6%) and a small portion gave exclusive breastfeeding, 29 people (41.4%). The temperature of newborns was primarily normal; namely, 60 people (85.7%) and a small proportion had hypothermia, nine people (12.9%). Most of the weight decreased by 66 people (94.3%). Most of the jaundice was not jaundice; namely, 66 people (94.3%) and a small portion had jaundice, four people (5.7%) (Table 3).
Respondents who gave exclusive breastfeeding were 29 people with a normal overall body temperature of 29 people (100%). In comparison, those who were not exclusively breastfed 41 people mostly had normal baby body temperatures 31 people (75.6%), and a small part had body temperature one baby has hyperthermia (2.4%). The statistical analysis results using the Chi-Square test resulted in a p-value=0.016 (p<0.05), meaning that there was an effect of breastfeeding with body temperature in newborns 0–72h (Table 4).
The 29 respondents gave exclusive breastfeeding with the baby's weight mainly decreased by 28 people (96.6%), and there was one person (3.4%) whose baby's weight remained constant, while those who were not exclusively breastfed 41 people mostly had baby weight. Thirty-eight people (75.6%) decreased, and a small proportion of the baby's weight increased by three people (7.3%). The results of the statistical analysis of the Chi-Square test resulted in a p-value of 0.168 (p>0.05), meaning that there was no effect of breastfeeding on body weight in newborns 0–72h (Table 5).
The respondents who gave exclusive breastfeeding were 29 people who did not have jaundice, 29 people (100%) while those who were not exclusively breastfed, 41 people were mostly not jaundiced, namely 37 people (90.2%) and a small portion of jaundice, namely four people (9.8 people). %). The results of the statistical analysis of the Chi-Square test yielded a value of p=0.083 (p>0.05), meaning that there was no effect of breastfeeding with the incidence of jaundice in newborns 0–72h.
DiscussionThe study results showed an effect of breastfeeding on the body temperature of infants aged 0–72h, both exclusive breastfeeding and not exclusive breastfeeding, including all carrying out IMD, namely 70 people (100%).
Early initiation of breastfeeding (IMD) is a condition when the baby starts breastfeeding itself after birth, when the baby can be able to suckle on its own, with the criteria that the mother's skin contact with the baby's skin occurs in the first 60min after the baby is born This process is known as skin to skin between the baby and mother so that the warmth from the mother's skin can automatically affect the temperature of the newborn who is prone to heat loss.4
Johnson's theory says that a newborn's skin temperature is between 36°C and 36.5°C. Babies have difficulty regulating body temperature, and this makes them susceptible to hypothermia. A drop in temperature between 1°C and 2°C can occur within the first hour of birth. One of the efforts to prevent a decrease in the baby's temperature in the first hour of birth is early breastfeeding initiation. In addition, in theory, the mother's skin functions as an incubator, a thermoregulator for the baby. Mother's skin temperature is 1°C higher than mothers who are not giving birth; with the occurrence of skin-to-skin contact, the mother's skin temperature will automatically increase by 2°C.
The results of this study are in line with research conducted by Hatini.5 The effect of early initiation of breastfeeding (IMD) on the stability of the baby's body temperature in Jumpandang Baru and Kassikassi Makasar in 2015, namely the group that did the right and wrong IMD both experienced a stable body temperature. The correct IMD group had a stable temperature with an average of 37.05°C, while the babies who did the wrong IMD had a stable temperature with an average temperature of 36.86°C. Even the results of this study are in line with Rahmawati's research entitled The relationship between early initiation of breastfeeding and an increase in body temperature of newborns in the independent practice midwife Puji Lestari Mawung Trucuk.2 The result is a relationship between BMI and an increase in body temperature of newborns where the value of p=0.049 (p<0.05).
Meanwhile, mothers who did not give exclusive breastfeeding had a hypothermic baby's body temperature as many as nine people (22%), which was between 36.1°C to 36.4°C. So it happens that the newborn's body heat loss can be through evaporation, conduction, convection, and radiation.
In addition to hypothermia, there was hyperthermia in 1 person (2.4%) with a body temperature of 37.6°C in mothers who did not give exclusive breastfeeding. Hyperthermia is an increase in body temperature above the hypothalamic setting point when the heat loss mechanism is disturbed or influenced by heat, for example, the use of heating devices that are too hot, thick clothing resulting in dehydration and lack of fluids or from breast milk substitutes such as formula milk so that it occurs. In addition, the baby's sensitivity (allergies) and a heat reaction occur in the baby's body.
When examined from the characteristics of the respondents, the education level and the mother's occupation influence not giving exclusive breastfeeding. This is following several studies in which, knowledge results from “knowing,” which occurs after people have sensed a particular object. Formal education factors influence knowledge itself. While the study results were based on the baby's weight, it was found that there was no effect of breastfeeding on the weight of infants aged 0–72h. This happens that newborns often experience weight loss because, in the womb, the baby gets nutrition directly from the mother through the umbilical cord so that when outside the womb, the baby must try to get nutrition results of this study are in line with research6 with the title The Relationship Between Frequency, Duration of Breastfeeding With Baby Weight At the Mariani Maternity Polyclinic Medan. The result was that there was no relationship between the frequency of breastfeeding and the baby's weight p=0.815 (p>0.05), and also between the duration of breastfeeding and the baby's weight p=0.092 (p>0.05). So is research7 with the title Relationship of Breastfeeding with Growth and Development of 6 Months Old Babies at Nanggalo Health Center with analysis results p=0.696 and developmental values p=0.062. This study explains that there is no relationship between breastfeeding and the growth and development of infants aged six months.
Meanwhile, those who did not give exclusive breastfeeding had three babies’ weight gain (7.3%). Excess weight in formula-fed babies indicates obesity, and obesity can occur when viewed from the normal growth curve of breastfed babies. The weight gain of babies fed formula milk is higher than that of babies who are exclusively breastfed. However, this does not mean that babies fed formula milk are better than exclusively breastfed babies.
When examined from the characteristics of the respondents, maternal parity influences the inability to breastfeed. Parity has something to do with seeking information about a mother's knowledge of breastfeeding. The experience gained by the mother can expand one's knowledge in breastfeeding. That the experience of mothers in caring for children affects knowledge about exclusive breastfeeding and the physical and psychological readiness of experienced mothers will undoubtedly be more prepared than mothers who have not experienced.8
Then these results also showed that there was no effect of breastfeeding on the incidence of jaundice in infants aged 0–72. It happens that babies who are breastfed often pass meconium early, so they tend to have a low incidence of physiological jaundice. Babies who are breastfed will have lower bilirubin levels because they defecate more often. Babies who are late to expel meconium will have a buildup of bilirubin levels, resulting in physiological jaundice, non-breastfeeding babies can increase bilirubin levels by up to 15mg/dl.9
The results of this study are in line with Ismarika's research10 with the research title The relationship of colostrum administration, frequency, and duration of breastfeeding to physiological jaundice of neonates in pediatric polyclinic and neonatology ward dr. Soetomo Surabaya. The result was that only colostrum administration had a moderate relationship and correlation with the incidence of physiological jaundice in neonates (p=0.000) while breastfeeding frequency (p=0.129) and breastfeeding duration (p=0.524) had no relationship.
Meanwhile, those who did not give exclusive breastfeeding had physiological jaundice as many as four people (9.8%). Jaundice that occurs early (second or third day) is caused by insufficient food intake because milk production is still lacking so that direct bilirubin that has reached the intestines is not bound by food and is not bound by excreted through the anus with food.
This research aligns with research11 with the title Differences in the Time of Giving colostrum to the Incidence of Physiological Jaundice in Newborns at RSU. Prof. Dr. Margono Soekarjo results that newborns who are not given colostrum early tend to appear physiological jaundice which is 13.5 times greater than babies who are given colostrum early. In contrast, respondents who were given colostrum early tended to appear 0.074 times less physiological jaundice than normal newborns who were not given colostrum early.
Conclusions and suggestionsExclusive breastfeeding can maintain a newborn's body temperature in a normal temperature state. There is no difference between exclusive breastfeeding or not exclusive breastfeeding on weight loss of infants aged 0–72h. There is no effect of exclusive breastfeeding on the incidence of jaundice in infants aged 0–72h. It is recommended that there is a lactation counseling room for both mothers who are still in care and for mothers who are going home.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.