The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosThe purpose of this study is to examine the sexual behavior relationship with HIV/AIDS on homosexuals in Palu City and its risk factors.
MethodThe study was held using a case-control with a retrospective study. The number of samples on the case–control group is 90 respondents with 1:1 comparison. Sampling techniques and data collection based on the medical record of VCT in Anutapura Hospital by using the questionnaire. The data is processed using the univariate analysis, bivariate analysis by using chi-square, and multivariate analysis by using logistic regression analysis.
ResultsBased on bivariate analysis gained that there is a significant relationship of sexual behavior in homosexuals with HIV/AIDS in Palu City. Dependent variable is HIV/AIDS while the independent variable are the number of pairs p=0.004 (OR=12.6); Anal sex p=0.003 (OR=3.6); Oral ejaculation p=0.002 (OR=14.2); Oral sex-licking/rimming p=0.035 (OR=2.5); Fingering p=0.019 (OR=2.8); and interfemoral coitus p=0.011 (OR=3.0). Based on the modeling of multivariate logistic regression analysis obtained, dominant variables are the number of pairs, anal sex, and interfemoral coitus, so the most dominant variables are the number of pairs with OR=20.8. Homosexuals that have more than one couple do bareback sex, and interfemoral coitus have an estimated probability of HIV/AIDS in Palu City is 83.7%.
ConclusionThere is a significant influence between sexual behavior against HIV/AIDS in homosexuals at Palu City in 2020.
AIDS that were first discovered in 1981, has evolved into a global health problem. Based on information obtained from the Center for Disease Control and Prevention (CDC), The United States publishes a weekly morbidity and mortality report (MMWR) describing a rare case of lung infections Pneumocystis carinii pneumonia (PCP) in the body of five previously healthy gay youth in Los Angeles. The five young men had an unusual infection that showed that their immune system was not functioning, where two of the five young men had died when the report was issued. The edition of the MMWR report marked the beginning of the AIDS epidemic.1 About 60 million people have infected HIV, and 25 million have died from AIDS. This makes AIDS one of the most devastating epidemics in history. According to the World Health Organization (WHO) in 2014, the results of the HIV/AIDS Epidemic report in 2013, there were 35 million people infected with AIDS and 2.1 million new HIV infections, and there were 1.5 million people who died from AIDS. This means that there are 6,000 infections daily in 2013.2
The first AIDS case in Indonesia was reported in Bali in April 1987, where a Dutch tourist died in RSUP Sanglah Denpasar. In the beginning, HIV/AIDS in Indonesia had occurred in commercial sex workers (PSK) and its customers and homosexuals. After that, there began to be a transmission to the infected housewives from his partner and continued to the babies born to HIV-positive mothers.3
In Indonesia, almost all areas of the province are not free from HIV/AIDS. This is in accordance with the data of KEMENKES RI (2012) explaining the situation of HIV/AIDS in Indonesia since the first case was discovered until December 2012, HIV/AIDS has spread at 345 (69.4%) from 497 districts/cities in all provinces in Indonesia. Incidence of HIV/AIDS cases occurring with the highest transmission risk factors through heterosexual sex risk (58.7%), then injecting drugs (27.9%), homosexual (12.3%) and perinatal (1.1%). Estimates and projections of new HIV infections by key population groups in Indonesia, where male sex men (MSM) groups occupy the highest number of cases. Significantly increased the number of cases in the year 2011 to 14,532–28,640 in 2016.4
The provincial health office of Central Sulawesi is noting that the HIV/AIDS in Palu City is the most or highest compared to other districts in the province. Data from the Palu City public health Office until September 2017, epidemiologically HIV/AIDS in Palu City from 625 cases, HIV reported 378 cases and AIDS 247 cases, 94 the case was passed away. If viewed from the gender of males amounted to 357 cases, females 268 cases. Based on a lot of age groups of HIV/AIDS, events occur in groups of age 20–29 years (47.84%), 30–39 years (34.4%), 40–49 years (11.2%), and 15–19 years (2.56%). Based on the way its transmission, the most cumulative through heterosexual (53.9%), men sex men (34.3%), and unknown (11.8%).5
Currently, studies that explore more detail the extent of risky sexual behaviors which can result in them being infected with HIV/AIDS and what causes them to routinely and dare to exercise unsafe free sex activities regardless of the risk of being infected with HIV-AIDS is very limited. This research aims to find out the relationship between sexual behavior in homosexuals with HIV/AIDS in the city of Palu has a considerable homosexual population. Latest Data obtained from the HIV/AIDS program and PIMS (sexually transmitted infections Program) of Palu City Health Office year 2020 number of cases of 80 cases of shemale and 240 cases of MSM so homosexual in total are 320 cases.6
There are many people who are HIV/AIDS that close themselves because more people with infectious diseases tend to close themselves and shame to tell about the disease. The transmission factor of this disease occurs due to the presence of heterosexual (free sex), homosexuals, and the use of syringes, but the greatest factor is free sex and homosexual. The result of the research that will be done is necessary as a reference/basic framework to develop a reproductive health intervention in the form of a continuous and comprehensive behavioral change to the key population that contributes in the prevention of the control of the HIV/AIDS epidemic in Indonesia specifically in the city of Palu.
Material and methodThe research was conducted in Anantapura Regional Public Hospital of Palu City and KDS Banuata Pura Support Foundation of Palu City, Central Sulawesi, from February to June 2020. This type of research is observational with a retrospective case-control study. The dependent variable on the study is HIV/AIDS, while its independent variable is the number of pairs and sexual behaviors of homosexuals, which are anal sex, oral ejaculation, Oral-licking/rimming, fingering, and interfemoral coitus. The population of studies on this study was homosexuals (MSM and shemale) who had conducted VCT at the Anutapura Regional Public Hospital, Palu City. The total sample of the study was 90 respondents, with a comparison of 1:1. The details of samples were taken, i.e., 45 case samples:45 control samples from Anutapura Hospital. Data collection for primary data using directly shared questionnaires or online questionnaires and secondary data in the form of medical records and the history of HIV/AIDS and Sexual Transmitted Diseases. Data is processed with univariate analysis to determine the characteristics of respondents, then input data into bivariate analysis by using Chi-square for correlation test and multivariate analysis to get the regression equation model and find probability sexual behavior related to HIV/AIDS in Palu City.
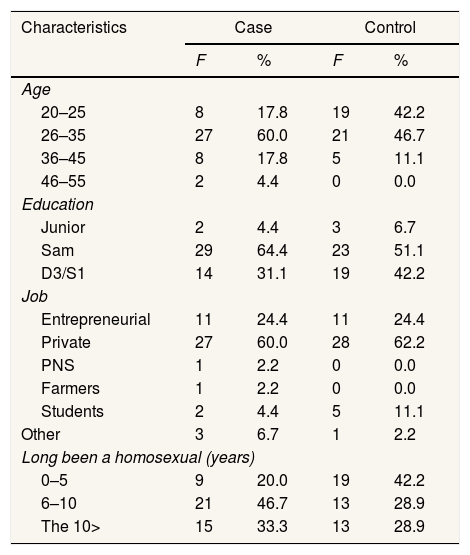
ResultRespondent characteristicsThe frequency distribution of respondents (homosexuals) for case groups and controls can be seen in Table 1.
Distribution of characteristics of respondent's cases and controls.
| Characteristics | Case | Control | ||
|---|---|---|---|---|
| F | % | F | % | |
| Age | ||||
| 20–25 | 8 | 17.8 | 19 | 42.2 |
| 26–35 | 27 | 60.0 | 21 | 46.7 |
| 36–45 | 8 | 17.8 | 5 | 11.1 |
| 46–55 | 2 | 4.4 | 0 | 0.0 |
| Education | ||||
| Junior | 2 | 4.4 | 3 | 6.7 |
| Sam | 29 | 64.4 | 23 | 51.1 |
| D3/S1 | 14 | 31.1 | 19 | 42.2 |
| Job | ||||
| Entrepreneurial | 11 | 24.4 | 11 | 24.4 |
| Private | 27 | 60.0 | 28 | 62.2 |
| PNS | 1 | 2.2 | 0 | 0.0 |
| Farmers | 1 | 2.2 | 0 | 0.0 |
| Students | 2 | 4.4 | 5 | 11.1 |
| Other | 3 | 6.7 | 1 | 2.2 |
| Long been a homosexual (years) | ||||
| 0–5 | 9 | 20.0 | 19 | 42.2 |
| 6–10 | 21 | 46.7 | 13 | 28.9 |
| The 10> | 15 | 33.3 | 13 | 28.9 |
HIV/AIDS cases respondent based on the most age in the category of the early adult age at a range of 26–35 years old (60%), while the least of which was in the category of the age of early elderly at the age range of 46–55 years old (4.4%). The respondents control based on the age most commonly in the category of the early adult age of 26–35 years old (46.7%), while the lowest in the age category of elderly 46–55 years old (0%). In terms of the last education, the majority of HIV/AIDS cases are high school graduates (64.4%), followed by bachelor graduates (31.1%), and junior high school (4.4%). Likewise, the majority of the control respondents were high school graduates (51.1%), followed by a bachelor graduate (42.2%) And the fewest junior high school graduates (6.7%).
Respondents in most cases worked as private employees (60%), followed by entrepreneurial (24.4%), students (4.4%), civil servants, and farmers (2.2%), and it does not work that is categorized as other (6.7%). At majority control, respondents worked in private companies (62.2%), then entrepreneurial (24.4%), students (11.1%), and others who are groups not working (2.2%). Respondents in most cases were males who became LSL 6–10 years (46.7%), followed by respondents who had been more than ten years living as the LSL (33.3%). And respondents who were only 0–5 years old to LSL (20%). While the control respondents dominated by the new LSL 0–5 years (42.2%), The rest were men who became LSL 6–10 years and more than ten years of equal number (28.9%).
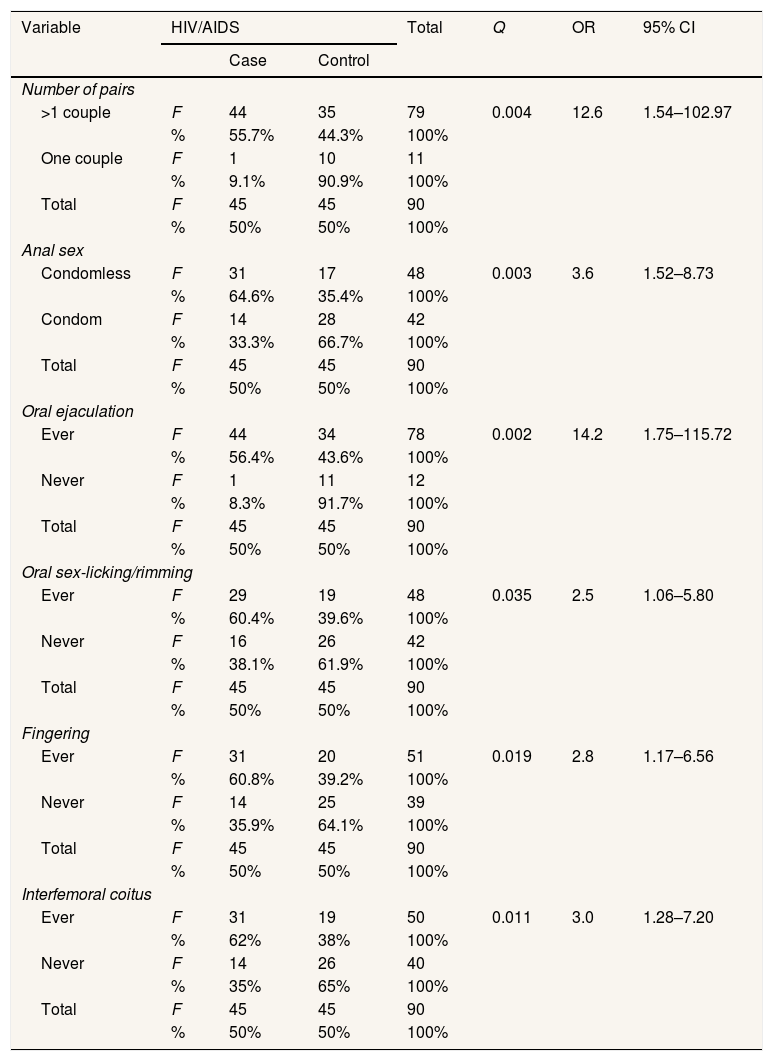
Bivariate analysisBivariate analysis is used to determine the relationship between independent variables and dependent variables that can be seen in Table 2. Based on the results of bivariate analysis obtained all variables in a row i.e. number of pairs (p=0.004; OR=12.6), anal sex (p=0.003; OR=3.6), oral ejaculation (p=0.002; OR=14.2), oral sex-licking/rimming (p=0.035; OR=2.5), fingering (p=0.019; OR=2.8) and interfemoral coitus (p=0.011; OR=3) has a value of p<0.05 which means there is a relationship and has a meaningful risk factor because the OR value of all variables >1 and all CI values of each variable does not contain the number 1 so that all risk factors relate to the dependent variable is HIV/AIDS.
Bivariate analysis results of dependent variables with independent variables.
| Variable | HIV/AIDS | Total | Q | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Case | Control | ||||||
| Number of pairs | |||||||
| >1 couple | F | 44 | 35 | 79 | 0.004 | 12.6 | 1.54–102.97 |
| % | 55.7% | 44.3% | 100% | ||||
| One couple | F | 1 | 10 | 11 | |||
| % | 9.1% | 90.9% | 100% | ||||
| Total | F | 45 | 45 | 90 | |||
| % | 50% | 50% | 100% | ||||
| Anal sex | |||||||
| Condomless | F | 31 | 17 | 48 | 0.003 | 3.6 | 1.52–8.73 |
| % | 64.6% | 35.4% | 100% | ||||
| Condom | F | 14 | 28 | 42 | |||
| % | 33.3% | 66.7% | 100% | ||||
| Total | F | 45 | 45 | 90 | |||
| % | 50% | 50% | 100% | ||||
| Oral ejaculation | |||||||
| Ever | F | 44 | 34 | 78 | 0.002 | 14.2 | 1.75–115.72 |
| % | 56.4% | 43.6% | 100% | ||||
| Never | F | 1 | 11 | 12 | |||
| % | 8.3% | 91.7% | 100% | ||||
| Total | F | 45 | 45 | 90 | |||
| % | 50% | 50% | 100% | ||||
| Oral sex-licking/rimming | |||||||
| Ever | F | 29 | 19 | 48 | 0.035 | 2.5 | 1.06–5.80 |
| % | 60.4% | 39.6% | 100% | ||||
| Never | F | 16 | 26 | 42 | |||
| % | 38.1% | 61.9% | 100% | ||||
| Total | F | 45 | 45 | 90 | |||
| % | 50% | 50% | 100% | ||||
| Fingering | |||||||
| Ever | F | 31 | 20 | 51 | 0.019 | 2.8 | 1.17–6.56 |
| % | 60.8% | 39.2% | 100% | ||||
| Never | F | 14 | 25 | 39 | |||
| % | 35.9% | 64.1% | 100% | ||||
| Total | F | 45 | 45 | 90 | |||
| % | 50% | 50% | 100% | ||||
| Interfemoral coitus | |||||||
| Ever | F | 31 | 19 | 50 | 0.011 | 3.0 | 1.28–7.20 |
| % | 62% | 38% | 100% | ||||
| Never | F | 14 | 26 | 40 | |||
| % | 35% | 65% | 100% | ||||
| Total | F | 45 | 45 | 90 | |||
| % | 50% | 50% | 100% | ||||
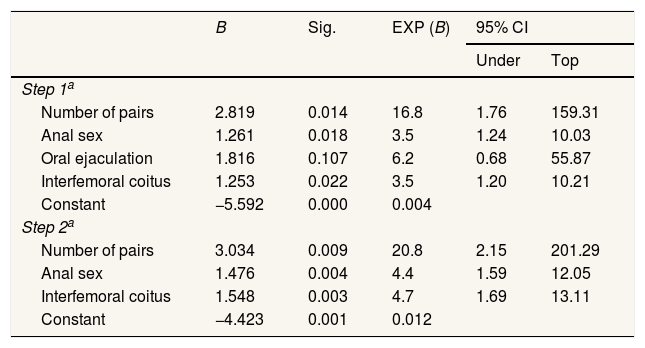
In the multivariate analysis, that will be done beforehand first selected variables that will be entered in the model. Variables that are included in the model analysis are variables that are in enough analysis to have a value of p<0.25. In the multivariate analysis, the variable selection in the input is based on the value of chi-square analysis by looking at the output of p-value in the line continuity correction with the help of the Statistical Package for the Social Sciences (SPSS) application program. The variables that met p<0.25 were inter-face sex (p=0.020), number of partners (p=0.010), anal sex (p=0.006). In the logistic regression analysis using the backward Wald method where the analysis of the results, a significant variable with p-value <0.05 is the final model chosen. Elimination is based on predictors that have a value of sig.>0.100.
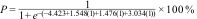
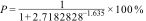
From the results of the model shown in Table 3 founds that are three independent variables, which are a number of pairs, anal sex dan interfemoral coitus. The Coefficient of each variables model put into the regression equation, so the probability of HIV/AIDS can be found as follows:
The final model of the logistic regression test is an influential risk factor with HIV/AIDS in homosexuals.
| B | Sig. | EXP (B) | 95% CI | ||
|---|---|---|---|---|---|
| Under | Top | ||||
| Step 1a | |||||
| Number of pairs | 2.819 | 0.014 | 16.8 | 1.76 | 159.31 |
| Anal sex | 1.261 | 0.018 | 3.5 | 1.24 | 10.03 |
| Oral ejaculation | 1.816 | 0.107 | 6.2 | 0.68 | 55.87 |
| Interfemoral coitus | 1.253 | 0.022 | 3.5 | 1.20 | 10.21 |
| Constant | −5.592 | 0.000 | 0.004 | ||
| Step 2a | |||||
| Number of pairs | 3.034 | 0.009 | 20.8 | 2.15 | 201.29 |
| Anal sex | 1.476 | 0.004 | 4.4 | 1.59 | 12.05 |
| Interfemoral coitus | 1.548 | 0.003 | 4.7 | 1.69 | 13.11 |
| Constant | −4.423 | 0.001 | 0.012 | ||
*1a, consecutive input variables are a number of pairs, anal sex, oral ejaculation, interfemoral coitus.
* 2a, oral ejaculation variable eliminated in the second step.
* Using the Backward Wald method.
Homosexuals that have more than one pair of couples, homosexuals who have sex without wearing condoms, and homosexuals who perform interfemoral coitus have a probability of infected HIV/AIDS by 83.7%.
DiscussionSexual behavior influence against HIV/AIDS in homosexual disease in Palu cityBased on the results of the chi-square statistical test obtained p-value=0.004 value with OR 12.6 (95% CI=1.54–102,97), which means there is a relationship between homosexuals having sex more than one partner with HIV/AIDS disease and at risk of 12.6 times greater infected by HIV/AIDS than those who only relate to one homosexual couple in Palu City. Based on the results of interviews from respondents to the research found, some respondents stated that they were not only sexually related to their spouse (girlfriends), but respondents had sexual intercourse with several other MSM for financial demands and satisfaction in having sex.
The sexual activity begins with seeking sexual partners through community meetings or other new MSM at regular meetings, public places, or other gay-only places they first meet in a viral manner on social media or other gay internet social Networks.7 The existence of a fixed pair did not close the possibility for LSL to have other sex partners. An average MSM has several sex partners and a relatively less courtship than a year; however, because the relationship contains warmth, the partner is referred to as a boyfriend.8
Based on the results of the chi-square statistical test obtained p-value=0.003 with OR 3.6 (95% CI=1.52–8.73), which means that there is a relationship between enjoying condomless anal sex in homosexuals with HIV/AIDS that are at risk of 3.6 times greater infected by HIV/AIDS than respondents who still use condoms. Based on the interview with the respondent obtained information about how to relate to the intimate/sexual intercourse of all the respondents in the city of Palu is by way of anal sex, all the respondents have had anal sex. Anal sex is a sexual activity performed by MSM/homosexuals to achieve its sexual gratification and is very dangerous because the anus contains many bacterial sources of disease. The Using condoms during sex performed will reduce sexual gratification in line with the results of research conducted Sidjabat (2017) in Semarang, which states MSM inconsistent with condoms have an infected risk of HIV/AIDS 3.4 times compared to those using condoms while performing sex. MSM does not use condoms for uncomfortable reasons or does not get satisfaction due to wearing condoms.7
The results of the chi-square statistical test obtained the p-value=0.002 value with OR 14.2 (95% CI=1.75–115.72); it can be concluded there is a relationship with oral ejaculation on the homosexuals with HIV/AIDS. And has a risk of 14.2 times greater to infected HIV/AIDS than homosexuals who have never done oral ejaculation. Based on the interview with the respondent who replied “yes” because of the desire of homosexual couples, while the answer “no” due to discomfort when having sex. Although the risk of transmission of HIV through oral sex is low, some factors may increase the risk, for example: due to injuries in the mouth or on the penis, bleeding gums, and other sexually transmitted diseases (STD). Complications from HIV/AIDS disease attack the most on oral/oral lesions that result in lesions/wounds (oral lesions). These lesions are caused by candida, herpes simplex, caposi sarcoma, oral HPV, gingivitis, HIV periodontitis, oral leukoplakia, weight loss, fatigue, and disability.9 Contrary to the statement stating that most experts agree that oral sex is not a high-risk behavior OF HIV-transmitted, the statement is based on the research results of Hartono (2009) revealed that fellatio (oral sex) have a low-risk level of HIV/AIDS transmission in the appeal with anal sex.10
Chi-square statistical test results obtained p-value=0.035 with OR 2.5 (95% CI=1.06–5.80), so it can be said that there is a relationship between sexual behavior that has been doing oral sex-licking/rimming in homosexuals with HIV/AIDS disease in the city of Palu and at risk of 2.5 times greater than those who do not have oral sex. From the interview with the respondent who replied “yes,” only rimming on his partner (boyfriend) and material demands, while the answer “no” because it does not enjoy the relationship of sex in rimming. Rimming behavior is done to obtain variation and enjoyment, but there is no data stating that the transmission of HIV/AIDS through rimming behavior.9 It was strengthened by the research of Sudin (2015) that rimming sex is merely as a sex variation. Anilingus/Rimming is also regarded as a risk that cannot be ignored, especially for couples receiving.10
The Chi-square statistical test results were obtained p-value=0.019 value with OR 2.8 (95% CI=1.17–6.56). So, it can be said that there is a connection to the anus is at risk 2.8 times greater to infected HIV/AIDS than those who have never put the finger on the anus in homosexuals with HIV/AIDS disease in the city of Palu. Based on the results of the interview with the respondent who replied “yes” doing so for material demands while the answer “no” because it does not enjoy when inserting a finger on the anus. The study results of Sudin (2015) stated that homosexuals had sex by plugging fingers into her partner's anus so that the anus was made for relaxing first before doing the anally, because if it was immediately inserted, it would feel pain. It starts using one finger then using two fingers.10 According to previous research that explains the fact that there has never been a case of HIV transmission by fingering (inserting finger into the anus/stimulates the finger). This behavior is at risk of transmitted HIV if the person does not keep his or her hands clean due to the wound or long nails resulting in the anticity blisters.11
Based on the statistical test results obtained p-value=0.011 with OR 3.0 (95% CI=1.28–7.20), which means that there is a relationship with interfemoral coitus in homosexuals with HIV/AIDS and is at risk of three times as large as infected with HIV/AIDS compared to homosexuals who have never performed interfemoral coitus in Palu City. The results of interviews with respondents answered “yes” due to material demands and to satisfy their partners (boyfriends) while responding “no” to not enjoying the way interfemoral coitus relates. Based on the research results of Sudin (2015) that interfemoral coitus would be at risk when there were friction injuries. Interfemoral coitus is considered a risk factor that can cause a person to be HIV-feted because an open wound is the entry HIV port.10
The most dominant sexual behaviorBased on the multivariate logistics regression analysis, the variable number of pairs is the dominant variable; in other words, it has the greatest influence on the model of the equation produced by the backward Wald method. This is in line with research conducted by Rumana (2019) through secondary data survey of integrated biology and Behavior (STBP) Ministry of Health in the region of Tangerang, Yogyakarta, and Makassar suggest that the reinforcing factor/amplifier that has a statistically meaningful relationship is the number of sexual partners (p-value=0.003), of which 405 respondents (67.6%) of a total of 599 respondents had a number of pairs of more than two people.12
The results of this study were in line with the research conducted by Susilowati (2009), which shows that respondents with a pattern of sex habits more than one partner had a risk of 2.886 times greater than the incidence of HIV and AIDS.13 The previous research also mentioned that respondents who had sexual partners ≥, two people, 2.36 times to be exposed to HIV AIDS compared with respondents who had only one spouse. The Research in Bukit Tinggi stated that the number of sexual partners is a risk factor FOR HIV AIDS transmission and statistically meaningful relationship between the number of sexual partners with the transmission OF HIV aids to the homosexual community (OR: 11.688 (95% CI, 2.082–65.605, p; 0.002) where couples who have sexual partners >1, 11.688 times are at risk to be infected WITH HIV AIDS when compared to respondents who only have one sexual partner. Therefore, the prevention efforts of HIV AIDS through loyal to the partner need to be more socialized and more effective again, especially in the homosexual community, considering the transmission of HIV/AIDS is riskier in this group. If they cannot be faithful, it is necessary to use condoms to avoid the risk of HIV transmission. Need better monitoring and evaluation so that the program can run effectively.
ConclusionThere is an influence between the sexual behavior of the number of pairs, the anal sex, the oral ejaculation, the anus-oral/rimming, fingering, and the interfemoral coitus on the homosexuals against HIV/AIDS in the city of Palu. Based on the results of a multivariate logistic regression test with the Backward Wald method acquired, the risk factor of probability infected by HIV/AIDS caused by risky sexual behavior in Palu city is 83.7%.
Conflicts of interestThe authors declare no conflict of interest.
The authors would like to thank the Dean and all Vice Dean, the Faculty of Public Health at Hasanuddin University, for the research funding.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.