To describe the quality of clinical records of deliveries and births by quantitative assessing the unfilled variables in birth data collection forms and their implications at Maternity Hospital, in the municipality of Lubango, Angola.
MethodThe study was conducted from January to August 2018. It adopted a quantitative research design, analysed variables not filled in a total of 202 birth record forms collected for 3 months (secondary data).
ResultsThe findings revealed that 80% of the sections of the entire set of information about obstetrical history were not filled in. This occurred with a relatively high frequency resulting in some of the relevant variables being left blank, such as antenatal diagnosis (94%) and the number of last menstruation (91%).
ConclusionsThe rate of missing fundamental information from the clinical birth record are high. This result has important implications in evaluating the quality of data and may, consequently, jeopardize: 1) the evaluation of the prenatal assistance, 2) the clinical assistance at delivery, and 3) decision-making for preventive and intervening procedures.
Describir la calidad de los registros clínicos de partos y nacimientos mediante la evaluación cuantitativa de las variables no cumplimentadas en los formularios de recolección de datos de nacimiento y sus implicaciones en el Hospital de Maternidad de Lubango, Angola.
MétodoEl estudio se realizó de enero a agosto de 2018. Adoptó un diseño de investigación cuantitativa y analizó variables no cumplimentadas en un total de 202 registros de nacimiento recolectados durante 3 meses (datos secundarios).
ResultadosLos hallazgos revelaron que el 80% de las secciones de todo el conjunto de información sobre la historia obstétrica no se completaron. Esto ocurrió con una frecuencia relativamente alta, lo que provocó que algunas de las variables relevantes se dejaran en blanco, como el diagnóstico prenatal (94%) y el número de la última menstruación (91%).
ConclusionesLa tasa de falta de información fundamental en el registro clínico de nacimientos es alta. Estos resultados tienen implicaciones importantes en la evaluación de la calidad de los datos y, en consecuencia, pueden poner en peligro: 1) la evaluación de la asistencia prenatal, 2) la asistencia clínica al parto y 3) la toma de decisiones para los procedimientos preventivos e intervinientes.
Provision of health care must ensure that it is the best for the clients. Services of assisting a pregnant woman should be rendered with safety to assure each woman and her new-borns the benefits of current scientific advances (evidence-based medicine), establishing in this way the practice of anticipation and prevention of obstetrical risks. To increase women, access to healthcare services and warrant the quality accomplishing a basic set of procedures are currently mandatory.1–3 Therefore, it is necessary to have data that describes the assistance to the mother and the new-borns from prenatal and labour to the puerperium.
The World Health Organization notes that the main aim of assisting a pregnant woman is to secure a healthy parturient and healthy new-born, with a minimum of clinical interventions. However, a set of practices and attitudes must be considered to attain a healthy labour and birth, as well as to prevent maternal and perinatal morbimortality.4
The existence of relevant information in the clinical birth records supports medical decision-making and reinforces breastfeeding guidelines, foetal well-being, labour, and puerperium. Thus, all the information related to the assistance granted to the parturient should be adequately collected and recorded in the pregnant woman's clinical file, which must be used as an analysis and evaluation tool of the labour evolution phases.5–7
There is a large amount of hospital information and associated data processing, and give the heterogeneity of health information systems, it is not easy to keep a single record of the activities of information systems and process stakeholders inside and outside the health institutions.8,9
The different information systems in use in hospital environments make the management and protection of patient data highly complex. The new requirements imposed on healthcare institutions, mainly in terms of security and protection of patient data, have forced the global healthcare sector to constantly evolve in the adoption of increasingly innovative information systems. Such as the use of decision support tools, as well as measures related to the traceability of information within health institutions and their relationship with external entities.8–10
However, to ensure that there is a prevalent and reliable utilization of the information recorded in these files, it is essential that the filling is done comprehensively, complete, and responsibly, so that this tool may promote the sharing of information among healthcare professional teams involved in current assistance and future appointments.11–15
The (re)use of data from hospital information systems is highly dependent on the quality of data collected by health professionals at the individual health facility level. Therefore, continuous monitoring and investment in hospital information systems are needed to improve data collection. These systems and data must be as reliable and as authentic as possible to meet the needs of hospital care, hospital management, and scientific research. Information and communication technologies bring a new approach to the quality of clinical records based on electronic hospital information systems.16–19
The information contained in the medical records constitutes an essential means of communication and sharing of data among health professional teams, mainly when this data is given meaning, and its registration is performed stringently with acceptable standard quality, which allows an overall view of the patient and warrants the sustainability of data, consequently the granted assistance.20–22
The literature consulted shows that hospital records were poorly filled out, that is, most of the variables analyzed, except for some variables, presented a rate of completion lower 90%. There are several reasons given for not completely filling out the medical records, among them, the main one has been the lack of time of the health professionals, especially those a work in emergencies rooms.23
The results point to the necessary caution regarding the use of official information on live births, in the sense that possible failures can interfere with the proper use of information on the maternal and child population, calculation of rates and planning of health actions for this population group. As well as arouses the attention of managers, regarding the maintenance of quality of hospital records and regarding the improvement of the stages of data collection, processing, and dissemination of health Information.24
The analyzed studies show that the partograph's devaluation is a reality of most institutions that provide obstetric care. It was found that professionals have a low level of knowledge about the use of the partograph and the interpretation of its records. Therefore, considering the findings, it is suggested that should be provided regular training on the use of the instrument. Furthermore, it is recommended to reinforce the use of the instrument through indicators and incentives that allow monitoring the practice of its use, elaboration and adoption of a protocol that includes the partograph in the assistance to labour.10,25,26
Several studies have concluded that obstetric professionals need to become aware of the importance of using the partograph and should start using this tool properly. The objective is a better monitoring and ease of graphic observation of the labour follow-up. Adherence to this practice could make vaginal obstetric care a safe, effective, and positive support for women in an interventionist model of care.25,27,28
It is necessary to intensify the guidance of those directly involved in data collection and to stimulate interest in the production of reliable information for the construction of more trustworthy information systems. In this way, the decisions to be made would be supported by data that reflect the reality of the event in question. For example, what could be reflected in intervention assistance and health policies to improve maternal and newborn health indicators.24,29
The large amount of information collected by many professionals into hospital records helps to build patient stories from admission to discharge. It is worth noting that both medical and nursing information are essential for the realization of the clinical process. However, there are many complaints related to eligibility and discontinuity of this information, often bringing irreversible damage to the user, the institution, health professionals, and society.
The purpose of this study is to describes the quality of clinical records of deliveries and births by quantitatively assessing the unfilled variables in birth data collection forms and their implications at Maternity Hospital, in the municipality of Lubango, Angola.
MethodStudy design and contextThe current study is part of a project to implement an electronic data system in Medical Admission, Archive, and Statistical Services, for the Maternity Hospital in Lubango municipality, Huila province in Angola. The interest in this research arose after assessing the “clinical records of childbirths” used for inserting data during the testing phase of the designed prototype called Obscare_Lubango.
This is a quantitative and cross-sectional study based on the analysis of secondary data from the delivery information system in Lubango Maternity Hospital, based on the data for the year 2016.
Survey population and sampleThis study was based in the expectant mothers’ clinical records of childbirths occurred between October to December 2016. The data collection process occurred from January to August 2018. The target hospital has a capacity of 180 beds and, according to the annual report produced in 2016, this institution carried out a total amount of 13,268 births.
Our target population are all expectant mothers, assisted in the concerned hospital, during 2016 fourth quarter which had a delivery by spontaneous expulsion (eutocic) or by cesarean section or other obstetric mechanical forms (dystocic). For this study, 202 records of births and deliveries conducted in the fourth quarter of 2016 were available by the hospital management to test the prototype of the electronic information system “ObsCare-Lubango”. It is a non-random sample.
Data collection techniquesSeveral interviews were performed with the person in charge and technicians who deal with the medical admission, archive, and statistical services to obtain their opinion on implementing an electronic data system in this area. Thus, we had the opportunity to observe and experience the forms of organization of the hospital clinical data and be informed about the data flowcharts, the procedures or protocols regularly adopted for data collection, processing, and presentation of collected data at the hospital level.
The data on deliveries and births can be collected in one of three different form templates: clinical form of childbirth, the partograph and clinical file of the patient's identification. These are described below:
- •
Model 1: the clinical form of childbirth. This is a national form template provided by the Angolan Ministry of Health and is considered the original one. It is divided into two parts: one part with the expectant mothers’ data and another with the new-born children's data.
- •
Model 2: the partograph. Based on the interview results, we learned that sometimes it was not possible to fill the original form (model 1), due to shortage of forms delivered by the Ministry of Health and the hospital incapacity to copy such temple. Consequently, the hospital created a new one, adopted from model 1 and that includes three pages. The computerized first page consists of the expectant mother's identification; the second computerized page contains some areas for triage by nurses (physical and obstetrical examinations). The third page is blank to record the new-born's data.
- •
Model 3: the clinical file of the patient's identification. This model is also the result of the adaptation of model 1. It has three pages: the first contains the expectant mother's identification data; the second includes information on the obstetrical triage, i.e., the physical and obstetrical examinations; the third page is entirely blank to record the summary of the labour event and the summary information of the new-born. The difference between the second model and this third one is that the latter includes some different areas.
Since the Ministry of Health does not have the capacity to continuously provide model 1, the hospital has also adapted models 2 and 3 for data collection. Since the data were collected using the three different models, the only option was to use all three models to avoid losing information during the analysis period.
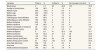
The three models in use at this institution present similar and different items and variables, as shown in Table 1. In the present study, all the unfilled variables in each area of information are appraised within the three templates used in the target institution. First, the procedure used to apply the reliability criterium of the data recorded in the “clinical records of childbirth” was quantifying the total number of the unfilled variables. Next, the unfilled variables frequency and the number of variables not included in certain “clinical records of childbirth” were verified, making thus, regularly the total sum of the analysed sheets.
Number of variables to be collected in each model per group of procedures.
| Groups | Number of data collection variables | Number of variables considered in the study* | ||
|---|---|---|---|---|
| Model 1(clinical form of childbirth) | Model 2(partograph) | Model 3(clinical file of the patient's identification) | ||
| Parturient identification | 11 | 15 | 24 | 19 |
| Obstetric history | 22 | 0 | 0 | 22 |
| Physical and obstetric examinations | 20 | 16 | 13 | 22 |
| Delivery data | 7 | 011 | 011 | 13 |
| New-born data | 11 | 13 | ||
In this study to describe the quality of information recorded in the Clinical obstetric form, we assessed the unfilled variables included in the templates for collecting the data regarding deliveries and births. All data were divided into five groups, namely:
- •
Data group of the mothers’ identification: consists of nineteen variables such as name, age, race, place of residence, blood type, etc., which allow the identification of mothers for archival, statistical, and professional purposes, in addition to individualizing patient care.
- •
Data group of the obstetric history: is a set of twenty-two variables from prenatal, clinical, and obstetric history, such as the number of consultations, pregnancies, deliveries, abortions, that support the elaboration of a diagnosis for obstetric risk assessment.
- •
Data group on physical and obstetric examinations of the parturient: is a set of twenty-two variables, seven of which are physical examination variables and the remaining fifteen of which are obstetric examination variables. These include laboratory results, maternal vital signs, uterine height, uterine dynamics, foetal heart rate, labour development, which allow health care professionals to analyse and assign other related factors or risk factors and make possible preliminary nursing diagnoses.
- •
Data group of deliveries: it is a coherent set of thirteen variables that assess the duration of labour, the mode of delivery by spontaneous expulsion (eutocic) or by caesarean section or other obstetric mechanical forms (dystocic), fetal presentation and postpartum haemorrhage. Thus, the mother's health status can be assessed in the last minutes of labour and afterwards.
- •
Data group on new-born and maternity discharge: is a set of thirteen variables that identify and assess the new-born's health status, allowing for more accurate care until discharge from the hospital. The variables include the race of the new-born, gender, weight (gr), APGAR, administration of the first vaccinations, and a preliminary diagnosis that allows assessing the condition of the output, whether it is expected, dead, or otherwise.
To better quantify the absence of the information, the variables were classified as follows:
- •
Filled variables: those included in the model with annotations (e.g., were filled in) regardless of their legibility or illegibility.
- •
Unfilled variables: those included in the model without any annotations (e.g., were not filled in).
- •
Not included variables: those contained only in some sheets (given that we worked with information from the three models).
The data collected for the present study was subject to descriptive statistics interpretation and analysis by using the frequencies to describe the categorical variables presented through absolute and relative frequency tables resulting from the use of the Software Statistical Package for Social Sciences (SPSS) version 21.0 as a supporting tool.
Ethical considerationsThe study was conducted with the permission of the General Director of the Hospital. Although this is not direct research on human subjects, the documents examined contain private and confidential information, so we endeavoured to comply with the standards and administrative procedures established by the general and clinical management of the hospital, which evaluated and approved the implementation of the project through Note No. 95/GDG/HMIN-L/2017, signed by the Director-General of the said hospital Maternity Irene Neto in Lubango on June 5, 2017.
ResultsThe results are presented in order of the five data groups of information recorded in the obstetric clinical form, based on the models in use, to collect the data, namely: 1) data group of the mothers’ identification; 2) data group, of the obstetric history; 3) data group on physical and obstetric examinations of the parturient; 4) data group of delivery, and 5) data group on new-born and maternity discharge.
Regarding the data obtained from the variable “expectant mother identification”, it was noted that out of 202 revised “clinical records of childbirth”, 75.5% of areas were filled in, 7.6% were unfilled, and 16.9% of them did not contain some variables. It is essential to highlight that 99% of the forms were not completed, the blood group variable; 84.2% of them do not include the expectant mothers’ municipality of residence, yet, as it can be observed, 96% and 34.2% of the total number of records did not contain the workplace and the expectant mother profession, respectively (Table 2).
Information recorded in the clinical form. data group of the mothers’ identification (n=202).
| Variables | Filled in | % | Unfilled in | % | Not included in the form | % |
|---|---|---|---|---|---|---|
| Blood group | 2 | 1.0 | 46 | 22.8 | 154 | 76.2 |
| Number of clinical forms | 199 | 98.5 | 3 | 1.5 | 0 | 0.0 |
| Mothers name | 202 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Mothers age | 202 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Mothers race | 199 | 98.5 | 3 | 1.5 | 0 | 0.0 |
| Father's name affilitation | 201 | 99.5 | 1 | 0.5 | 0 | 0.0 |
| Mother's name affilitation | 199 | 98.5 | 3 | 1.5 | 0 | 0.0 |
| Mothers birthplace | 202 | 100 | 0 | 0.0 | 0 | 0.0 |
| Mothers residence | 195 | 96.5 | 7 | 3.5 | 0 | 0.0 |
| Mothers municipality of residence | 32 | 15.8 | 19 | 9.4 | 151 | 74.8 |
| Husband's name | 201 | 99.5 | 1 | 0.5 | 0 | 0.0 |
| Mothers workplace | 8 | 4.0 | 41 | 20.3 | 153 | 75.7 |
| Mothers profession | 133 | 65.8 | 21 | 10.4 | 48 | 23.8 |
| Mothers marital status | 149 | 73.8 | 5 | 2.5 | 48 | 23.8 |
| Mothers literacy qualification | 134 | 66.3 | 20 | 9.9 | 48 | 23.8 |
| Mothers family phone number | 51 | 25.2 | 103 | 51.0 | 48 | 23.8 |
| Entry date (dd/mm/yy) | 202 | 100 | 0 | 0.0 | 0 | 0.0 |
| Entry time | 200 | 99.0 | 2 | 1.0 | 0 | 0.0 |
| Health professional signature | 186 | 92.1 | 16 | 7.9 | 0 | 0.0 |
About the “information recorded in the clinical form, in the data group, of the obstetric history”, shows that of the 202 clinical obstetric records examined, only 20% had completed the twenty-two variables in the obstetric history data group. The group of variables that did not complete included the number of prenatal consultations (94.5%), number of pregnancies (76.7%), number of abortions (80.2%), date of last birth (90.6%), and date of last menstruation (91.8%) (Table 3).
Information recorded in the clinical form, in the data group, of the obstetric history (n=202).
| Variables | Filled in | % | Unfilled in | % | Not included in the form | % |
|---|---|---|---|---|---|---|
| Did pre-birth consultations (yes/no) | 11 | 5.4 | 37 | 18.3 | 154 | 76.2 |
| Medical centre/post full name | 10 | 5.0 | 38 | 18.8 | 154 | 76.2 |
| Number of examinations (1, 2 or more) | 28 | 13.9 | 20 | 9.9 | 154 | 76.2 |
| Number of unknown examinations | 0 | 0.0 | 48 | 23.8 | 154 | 76.2 |
| High obstetric risk (yes/no) | 19 | 9.4 | 29 | 14.4 | 154 | 76.2 |
| If yes, what is the cause of the obstetric high risk? | 18 | 8.9 | 30 | 14.9 | 154 | 76.2 |
| Number of gestations | 47 | 23.3 | 1 | 0.5 | 154 | 76.2 |
| Number of deliveries | 44 | 21.8 | 4 | 2.0 | 154 | 76.2 |
| Number of dead born | 41 | 20.3 | 7 | 3.5 | 154 | 76.2 |
| Number of dead children | 40 | 19.8 | 8 | 4.0 | 154 | 76.2 |
| Number of alive children | 40 | 19.8 | 8 | 4.0 | 154 | 76.2 |
| Number of abortions | 40 | 19.8 | 8 | 4.0 | 154 | 76.2 |
| Number of caesareans | 40 | 19.8 | 8 | 4.0 | 154 | 76.2 |
| Number of forceps | 40 | 19.8 | 8 | 4.0 | 154 | 76.2 |
| Number of suction cups | 40 | 19.8 | 8 | 4.0 | 154 | 76.2 |
| Date of last labour | 19 | 9.4 | 29 | 14.4 | 154 | 76.2 |
| History of haemorrhages | 6 | 3.0 | 42 | 20.8 | 154 | 76.2 |
| Date of last menstruation | 17 | 8.4 | 31 | 15.3 | 154 | 76.2 |
| Probable date of delivery | 16 | 7.9 | 32 | 15.8 | 154 | 76.2 |
| Gestation period (week or months) | 192 | 95.0 | 10 | 5.0 | 0 | 0.0 |
| Complication of the current pregnancy (yes/no, which one?) | 15 | 7.4 | 33 | 16.3 | 154 | 76.2 |
| Main complaint | 167 | 82.7 | 35 | 17.3 | 0 | 0.0 |
The “information recorded in the Clinical form, in the data group on physical and obstetric examinations of the parturient“we see that, as for the regarding general physical examinations, seven variables were considered, and shows that out of the total number of the clinical forms of birth revised (40.1%), the digital vaginal examination variable was not filled, i.e., it is not included in the form. Likewise, the data for expectant mothers’ pulse and body temperature measurements were not recorded, accounting for 72.8% and 98.5%, respectively. The data relating to”obstetric examinations” that obstetric palpation procedures reveal high frequencies of incompleteness, i.e., this variable does not exist in the data form about the quality of contractions (77.2%), uterine tone (86.6%), and polo (the presentation part of the foetus head in the pelvis) (80.7%) (Table 4).
Information recorded in the clinical form, in the data group on physical and obstetric examinations of the parturient (n=2020).
| Variables | Filled in | % | Unfilled in | % | Not included in the form | % |
|---|---|---|---|---|---|---|
| Information on general physical examinations | ||||||
| Overall state (good, reasonable or bad) | 191 | 94.6 | 11 | 5.4 | 0 | 0.0 |
| Blood pressure (___/___mmHg) | 184 | 91.1 | 18 | 8.9 | 0 | 0.0 |
| Digital vaginal examination (TV) | 121 | 59.9 | 37 | 18.3 | 44 | 21.8 |
| Pulse (_ per minutes) | 55 | 27.2 | 147 | 72.8 | 0 | 0.0 |
| Temperature | 3 | 1.5 | 199 | 98.5 | 0 | 0.0 |
| Mucosae (coloured, uncoloured) | 185 | 91.6 | 17 | 8.4 | 0 | 0.0 |
| Oedemas (no/yes; if yes, number of crosses) | 193 | 95.5 | 9 | 4.5 | 0 | 0.0 |
| Obstetric exam information | ||||||
| Palpation | ||||||
| Uterine dynamics | 176 | 87.1 | 26 | 12.9 | 0 | 0.0 |
| Quality of contractions | 46 | 22.8 | 2 | 1.0 | 154 | 76.2 |
| Uterine tonus | 27 | 13.4 | 21 | 10.4 | 154 | 76.2 |
| Polo (movable, embedded) | 39 | 19.3 | 9 | 4.5 | 154 | 76.2 |
| Plan (I, II, III, IV) | 173 | 85.6 | 29 | 14.4 | 0 | 0.0 |
| Uterine height (cm) | 194 | 96.0 | 8 | 4.0 | 0 | 0.0 |
| Foetal heart rate | 186 | 92.1 | 16 | 7.9 | 0 | 0.0 |
| Foetus presentation | 193 | 95.5 | 9 | 4.5 | 0 | 0.0 |
| Digital vaginal examination | ||||||
| Cervix (thick, medium, thin) | 182 | 90.1 | 20 | 9.9 | 0 | 0.0 |
| Dilatation | 196 | 97.0 | 6 | 3.0 | 0 | 0.0 |
| Amniotic sac (integral) | 160 | 79.2 | 42 | 20.8 | 0 | 0.0 |
| Amniotic sac (broken) | 30 | 14.9 | 172 | 85.1 | 0 | 0.0 |
| Amniotic fluid | 106 | 52.5 | 96 | 47.5 | 0 | 0.0 |
| Preliminary diagnosis | 47 | 23.3 | 1 | 0.5 | 154 | 76.2 |
| Signature | 147 | 72.8 | 55 | 27.2 | 0 | 0.0 |
The result in “obstetric examinations“shows some high frequencies of information absence in specific digital vaginal examination procedures. Also, it can be seen, 79.2% of the amniotic sac (integral) variable frequencies were filled in the right area, which implies that the remaining 20.8% not filled in should be attributed to the broken amniotic sac. Nevertheless, within the broken amniotic sac, only 14.9% were filled. Another information to consider is the unfilled variables about the amniotic fluid colouring (47.5%) and the preliminary diagnosis (76.7%) (Table 4).
The information recorded in the clinical form related to the data group of deliveries related to the period of foetal expulsion (partograph) and after foetal expulsion, ending after the placenta delivery. Concerning “partograph”, 72.6% of the variables were filled, whereas the remaining 27.4% of them were not filled. It should be highlighted that the high frequency of unfilled variables related to the type of labour and other obstetric mechanic forms account for 23% and 72%, respectively, of the total number of unfilled variables (Table 5).
Information recorded in the clinical form, related to the data group of deliveries (n=202).
| Variables | Filled in | % | Unfilled in | % | Not included in the form | % |
|---|---|---|---|---|---|---|
| Partogram | ||||||
| Date of labour (__/__/___) | 197 | 97.5 | 5 | 2.5 | 0 | 0.0 |
| Hour of labour (__/__) | 197 | 97.5 | 5 | 2.5 | 0 | 0.0 |
| Type of deliveries (eutocic, dystocic, caesarean) | 139 | 68.8 | 63 | 31.2 | 0 | 0.0 |
| Presentation (cephalic, vicious cephalic, pelvic) | 197 | 97.5 | 5 | 2.5 | 0 | 0.0 |
| Other obstetric mechanical forms (forceps, suction) | 3 | 1.5 | 199 | 98.5 | 0 | 0.0 |
| Dequitature (placenta) | ||||||
| Date (_/_/_) | 39 | 19.3 | 9 | 4.5 | 154 | 76.2 |
| Hour (_/_) | 40 | 19.8 | 8 | 4.0 | 154 | 76.2 |
| Process (spontaneous, by expression, by hand) | 39 | 19.3 | 9 | 4.5 | 154 | 76.2 |
| Form (complete, incomplete, membrane remnant) | 190 | 94.1 | 12 | 5.9 | 0 | 0.0 |
| Postpartum haemorrhage | 155 | 76.7 | 47 | 23.3 | 0 | 0.0 |
| Perineum epistemic state (yes/no) | 33 | 16.3 | 169 | 83.7 | 0 | 0.0 |
| Perineum laceration state (No, 1st, 2nd, 3rd) | 37 | 18.3 | 165 | 81.7 | 0 | 0.0 |
| Laceration cervix (yes/no) | 26 | 12.9 | 176 | 87.1 | 0 | 0.0 |
Regarding the data related to ending after the placenta delivery, relative high frequencies of unfilled or not included information in the form, such as date (80.7%), hour (80.2%), and placenta expulsion process (80.7%). Furthermore, it should be noted a failure of unfilled information related to postpartum haemorrhages (23.3%); perineal state”episiotomy“(83.7%); perineal state”laceration“(81.7%), and cervical tear (87.1%) (Table 5).
Concerning “information recorded in the clinical form, in the data group on new-born and maternity discharge”, the result indicates that within the information related to the new-born, 79% of the variables were recorded. However, out of the total number of forms, 77.7% were not filled with information on the race variable. Likewise, within the information related to nursery ward admissions, 63% of related variables do not exist in the sheet, and 31.9% were not filled. Thus, most analysed”clinical forms of birth“did not complete this area, nor was the variable related to the mother's state when leaving the hospital (Table 6).
Information recorded in the clinical form, in the data group on new-born and maternity discharge (n=202).
| Variable | Filled in | % | Unfilled in | % | Not included in the form | % |
|---|---|---|---|---|---|---|
| New-born | ||||||
| New-born race | 45 | 22.3 | 157 | 77.7 | 0 | 0.0 |
| New-born gender (male/female) | 192 | 95.0 | 10 | 5.0 | 0 | 0.0 |
| New-born weight (g) | 191 | 94.6 | 11 | 5.4 | 0 | 0.0 |
| APGAR (1st minute, 5th minute) | 192 | 95.0 | 10 | 5.0 | 0 | 0.0 |
| Health professional signature | 178 | 88.1 | 24 | 11.0. | 0 | 0.0 |
| Nursery observations | ||||||
| Nursery observations notes | 47 | 23.3 | 155 | 76.7 | 0 | 0.0 |
| Eye prophylaxis (yes/no) | 2 | 1.0 | 45 | 22.3 | 155 | 76.7 |
| Vaccination (BCG, poliomyelitis) | 1 | 0.5 | 46 | 22.8 | 155 | 76.7 |
| Admission in the nursery | 0 | 0.0 | 47 | 23.3 | 155 | 76.7 |
| Decisive diagnosis | 0 | 0.0 | 47 | 23.3 | 155 | 76.7 |
| Date of the new-born discharge from nursery (dd/mm/yy) | 0 | 0.0 | 47 | 23.3 | 155 | 76.7 |
| Discharge | ||||||
| Condition of output (normal, dead, other) | 1 | 0.5 | 47 | 23.3 | 154 | 76.2 |
| Date of mother's discharge | 196 | 97.0 | 6 | 3.0 | 0 | 0.0 |
Based on the premise that the records are a criterion for evaluating the quality of the assistance provided, some authors reiterate the importance of certain aspects to be considered in these records, such as the legibility of the records, their completeness’correct and complete completion of the data collection instrument.30–33
When the nursing team performs some activities, but does not record them, it makes quality care impossible and prevents the capture of data to subsidize the planning of actions to be developed with the patient and the population in general. The professionals need to value the importance of their notes to organize and plan their assistance, always filling their records completely.32,33
The information contained in obstetric records is essential for clinical decision-making to ensure maternal health during pregnancy and delivery. As blood loss (haemorrhage) is one of the causes of maternal death, the fact that the blood type variable was not filled out in most (99%) of the obstetric clinical records analysed is worrying. Another worrying result is the fact that in 80% of these forms, the variables in the obstetric history data group were not filled out. Failure to complete essential variables, such as vital signs, quality of contractions, uterine tone, provisional diagnosis of care, vaccination data and observation notes from the new-born's nursery in the infant ward, should be considered as a case of very worrisome failure with implications for support and assessment of obstetric risk.
Several studies consider the good quality of data recorded in clinical records as very relevant for: decision-making, scheduling of health actions, which in turn facilitate access to care and continuity of care provided. However, the lack of standardization and the failure to fill in the variables in the forms demonstrate their failures in the data collection processes and, consequently, weaknesses in the hospital information system.2,5,11
Obtaining information that supports decision-making to improve the health of a population is essential for health managers, as this knowledge is used in planning, organizing, and evaluating health interventions and services. In addition, as a basis for diagnosing the health situation, decision-makers need reliable information on the morbidity and mortality profile, risk factors and their determinants, demographic characteristics, and health services.31,33,34
Having a goods statistic on vital events contribute to the continuous improvement of population health, and their dissemination favors a positive social impact of the actions undertaken. However, health information is not always of good quality, depending directly on the coverage of the events recorded and the reliability of the data collected.10,24,34,35
Patient identification is a crucial administrative procedure for obtaining a set of necessary data that allow linking with other extremely important information for clinical decision-making. As the results of our study show, the lack of information about the blood group variable of the parturient may prevent the medical team from making decisions about the need for blood transfusion, which is common in obstetric care in hospitals in Angola. The detection of the weaknesses of the health system in Angola, and the interpretation of the worrying indicators of maternal health in the country, are affected by the lack of reliable information, making it difficult to implement measures to improve maternal and child care.21
The results show the high frequency of non-completion of most variables in the obstetric history group. Among other variables in this group, the lack of information about prenatal care is concerned, namely data on medical or nursing care for pregnant women from conception to the beginning of labour. This is a gap that hinders the clinical decision-making process. Therefore, information about prenatal consultations is essential, as they serve to reduce maternal and child mortality, identify diseases and changes that threaten health, and prepare women for a healthy lifestyle before and after childbirth. Several studies show the potential of prenatal data collection as a basic source of epidemiological information. However, its reliability is compromised by the fact that these data are not collected at other levels of care and in information systems, and the collection models are incomplete in some aspects.12,13,16
The information about the physical examinations aims to observe and monitor physiological changes and identify existing maternal knowledge for better guidance of procedures that play a vital role in the parturient health. Unfortunately, the results show no information on some variables in this group, such as vital signs, pulse per minute, and temperature. Therefore, it can be considered a dangerous gap for childbirth care data.
As for the set of obstetric exam variables, these include obstetric palpation procedures to recognize the foetus, its situation, presentation, and position, to obtain a pregnancy diagnosis, identify the number of foetuses, assess foetal size and weight, as well as evaluate labour service and check the number of contractions. It is important to highlight here that the variables of the digital vaginal exam, in which the occurrence of expulsion of foetuses in emergency rooms or wards (deliveries outside the delivery room) can be presumed, were also not fulfilled. This procedure makes it possible to assess the progress of the pregnancy or check for signs of the beginning of the delivery service, as well as early identification of any complications for the mother or baby. In addition, it can provide information to prevent delayed labour and identify abnormalities during labour to ensure the quality of delivery care, thus reducing maternal and foetal mortality and morbidity. Studies on maternal and child care show that the absence of this information limits health professionals in obtaining data that allow them to have an overview of the evolutionary phase of the foetus’ expulsion, which can lead to errors.3,15
Labour marks the end of pregnancy and the birth of the child who developed in the mother's womb. In the variables of the partograph, there was a failure in recording the type of delivery and high percentages of non-completed/not included in the template (e.g., lack of date and time of the placental expulsion process). Studies show that the absence of this information can affect clinical decision-making in case the mother returns to the hospital with postpartum problems or even pregnant.4
Childbirth is a very special moment for mother and baby, both physically and psychologically. For this reason, the first exams are performed with the new-born to assess its level of adaptation to life outside the placenta by weighing and submitting it to other specific tests and evaluating the optimization of breathing; APGAR Index, ocular prophylaxis, first vaccinations, among others. These variables are essential information to ensure good care for the baby. There are almost no records of admissions of babies to nurseries. Some of the variables analysed in this item also have data quality problems and not recording them can affect the new-born's surveillance status.
When we asked some stakeholders in the hospital information system (e.g., emergency department and delivery room nurses) about the reasons for not capturing some of the essential variables of the delivery record, one of the most common answers was “the delivery record template has too many fields to be filled in, and that cannot be captured at the same time as caring for a pregnant woman who is in labour”.
About the opinion of each interviewee regarding the main gaps in the availability of information at the hospital level, the following answers should be noted, among others:
- •
“Lack of organization of hospital archives… the inadequate filling of models and books by nurses and doctors who sometimes lack records… lack of specific training in the statistical area for the professionals who collect the information.”
Regarding the proposal to improve the process of collecting, processing, and analysing statistical data collected in the hospital, among others, we have selected the following suggestions:
- •
“I would like us to have an organized computer system to better perform data collection for research purposes or even specific information about the services provided in a given period… Frequent training for staff involved in the collection, processing, and analysis of statistical data.”
Scientific and clinical research depends, to a large extent, on the access and (re)use of clinical records generated and resulting from the provision of care. Given the constraints of the entire process in the Lubango maternity information system, namely because it is carried out in a traditional way (manually with sheets of paper), the responses and suggestions of the actors involved in this data collection process should be considered not only as a manifestation of the weaknesses of this information system, but also as an opportunity to change towards the organization of a new hospital information system with computerized preferences that will support the administrative and clinical decision-making process.
It should also be noted that the daily record, computerized or not, of the collected data is not enough. These data must necessarily be critically analysed and linked to clinical characteristics, so that they can be properly interpreted.12,18,20
LimitationsThe impossibility of evaluating the integrity of the information collected in the forms, and the absence of a manual for filling out the clinical delivery forms are some of the limitations of this information collection system and, consequently, the study.
ConclusionsThe analysis of the results showed that the quality of the information contained in the “clinical records of childbirth” is poor. There are weaknesses in completing the data by the health professionals (nurses and doctors) of the Lubango Maternity Hospital. Also, several important information was left blank, and, in some cases, the adapted form templates do not contain such variables.
The essential information related to clinical aspects obtained high percentages of not being filled in or does not appear in the sheet, mainly in obstetrics background and physical examinations. These failures may compromise the quality and evaluation of prenatal care and procedures in labour and call into question the validity of decisions to be taken in preventive and interventional actions.
The analysis of the records allowed us to have an overview of the failures that occurred while filling in the “clinical records of childbirth” of Lubango Maternity Hospital, province of Huila in Angola, as is the case of the births where hardly any babies were admitted to the nurseries, which has its influence on the state of health of new-borns monitoring, as well as questioning the reliability of data.
We believe that this research may be relevant for health professionals, who perform as the main actors in registering and filling out the information collection forms in use in this health institution. This will allow them to make a critical analysis of their activities and improve their decision-making actions.
A reflection on the subject can make these health professionals aware of the importance of correctly filling out childbirth forms and their participation in improving the quality of information, and consequently, in the improvement of pregnant women's care.
- •
There is no literature on what is currently known about the types and quality of maternal-child health records in Angola's maternities. However, there is evidence from other studies that the socio-cultural conditions, education, race/color, and marital status of pregnant women, when properly completed, provide a more accurate assessment of social vulnerability and risk factors for mothers and newborns.
- •
Professionals need to be sensitized to the proper records of assistance provided to pregnant women, requiring monitoring through supervision contained in the records made so that flaws in filling it out are detected.
- •
The quality of records in hospital information systems impacts the improvement of health care delivery, hospital management, and scientific research.
- •
This study is the first to be carried out in this health region of Angola, which assesses the quality of the records made in the clinical birth records and contributes to reinforcing the need for training and periodic qualification of professionals for acceptable use of the health system. prenatal and birth information.
- •
The results of this study may lead to behavioral changes in health professionals and hospital managers due to the need to improve the quality of proper data collection and raise awareness of the importance of these data in supporting maternal and child care.
- •
The article warns of the severe consequences that deficiencies in the collection of obstetric information can have on delivering services in the various maternity facilities. Therefore, health policymakers in Angola urgently need to change their information systems from paper records to information systems based on information technologies, preferably low-cost or open-source electronic medical records software.
Mercedes Carrasco Portiño.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsTomas Hambili had the main responsibility for bibliographic research, manuscript. Tomas Hambili and Tiago Costas were responsible for data collection and statistical analysis. The authors Anabela Almeida and Ricardo Correia actively contributed to all parts of the article, including the interpretation of the data, revision and approval of the text. In addition, all authors contributed to preparing the data collection instrument and approved the final version
FundingThis study had no funding from any organization. The researcher uses his funds for transportation and reproducing materials.
Conflicts of interestThe authors declare that there is no conflict of interests.