This study provides an overview of the perceptions of primary care professionals on how the current primary health care (PHC) attributes in Spain could influence health-related responses to intimate partner violence (IPV).
MethodsA qualitative study was conducted using semi-structured interviews with 160 health professionals working in 16 PHC centres in Spain. Data were analysed using a qualitative content analysis.
ResultsFour categories emerged from the interview analysis: those committed to the PHC approach, but with difficulties implementing it; community work relying on voluntarism; multidisciplinary team work or professionals who work together?; and continuity of care hindered by heavy work load. Participants felt that person-centred care as well as other attributes of the PHC approach facilitated detecting IPV and a better response to the problem. However, they also pointed out that the current management of the health system (workload, weak supervision and little feedback, misdistribution of human and material resources, etc.) does not facilitate the sustainability of such an approach.
ConclusionThere is a gap between the theoretical attributes of PHC and the “reality” of how these attributes are managed in everyday work, and how this influences IPV care.
Este estudio presenta las percepciones de profesionales de atención primaria sobre cómo los atributos de la atención primaria en España pueden influenciar las respuestas sanitarias a la violencia del compañero íntimo (VCI).
MétodosEstudio cualitativo con entrevistas semiestructuradas con 160 profesionales sanitarios de 16 centros de atención primaria en España. Los datos se analizaron con el enfoque de análisis de contenido.
ResultadosDel análisis de las entrevistas emergieron cuatro categorías: Implicados/as con el enfoque de primaria, pero enfrentando dificultades para implementarlo; El trabajo comunitario depende del voluntarismo; ¿Trabajo multidisciplinario o profesionales que trabajan juntos?; y Continuidad amenazada por la sobrecarga de trabajo. Los participantes consideraron que la atención centrada en la persona y otros atributos del enfoque de atención primaria facilitaban la detección de VCI y una mejor respuesta a este problema. Sin embargo, también reconocieron que la forma en que se gestionan los servicios sanitarios (sobrecarga de trabajo, débil supervisión y escaso feed-back, distribución de los recursos humanos y materiales, etc.) no facilita la sostenibilidad de este enfoque.
ConclusiónExiste una brecha entre los atributos teóricos de la atención primaria y la «realidad» de cómo estos atributos se gestionan en la actividad profesional del día a día y de qué manera esta influye en la atención a la VCI.
Men's intimate partner violence (IPV) against women, is a global public health problem and has devastating effects on the health and wellbeing of women and children.1–3 Health care services, and especially primary health care facilities, can play a key role in alleviating the effects of IPV, since they are the gatekeepers of the health system and therefore the public institutions most frequently accessed by women exposed to IPV, even if not all of them will disclose this situation.1,4–7 In this study IPV was defined as “any behaviour within an intimate relationship that causes physical, sexual or psychological harm, including acts of physical aggression, sexual coercion, psychological abuse and controlling behaviours”,3 and it was explicitly stated that the focus was on IPV exerted by men against women.
When it comes to implementing promotive and preventive interventions against complex problems that transcend the traditional responsibilities of the health system, a primary health care (PHC) approach characterized by the attributes of person/family-centred, longitudinal, comprehensive, coordinated and community-oriented care, is considered to be more effective.8–10 The attributes of PHC initially proposed by Barbara Starfield as a set of dimensions to measure adequacy of the primary care organization and its characteristics for service delivery, have been extensively described as positively associated to successful provision of preventive services.10,11 Under these attributes, multidisciplinary teams working in PHC act as a key interface linking ambulatory care with hospital and specialty services, and individual care with other community-social services. Some studies point out that these features of PHC could positively contribute to the implementation of comprehensive responses to IPV.12–14
Since the early 80's when the health care system in Spain underwent a major transformation, health delivery has become sectorized and focus has been placed on first-line health care facilities −called primary health care centres (PHCC)− where the health care workforce is organized around multidisciplinary teams.15 The Spanish PHCC have been developing and expanding, showing improved integration of services, good coordination of care, and an appropriate family-orientation within the services. In regards to the health care response to IPV in Spain, the actions have included: training of health care professionals, developing protocols, and establishing monitoring systems.
As of 2015, there are 13,187 PHCC in Spain, and the health system has performed well in international comparisons.16–19 Primary care scores for Spain are among the highest in Europe in terms of governance, access, continuity and structural aspects, medium in terms of coordination and comprehensiveness and lower in terms of efficiency.19 The current financial crisis has led to austerity measures within the Spanish health care system, including reduced public spending, salary reductions and reduced services for certain groups like undocumented migrants.16,18,20–22 This situation constitutes a challenge for effectively dealing with health problems in general,20 and IPV in particular.
This study aims to provide a snapshot of the different perceptions of professionals working in first-line health facilities on how the current operationalization of PHC attributes in Spain could influence the responses to IPV.
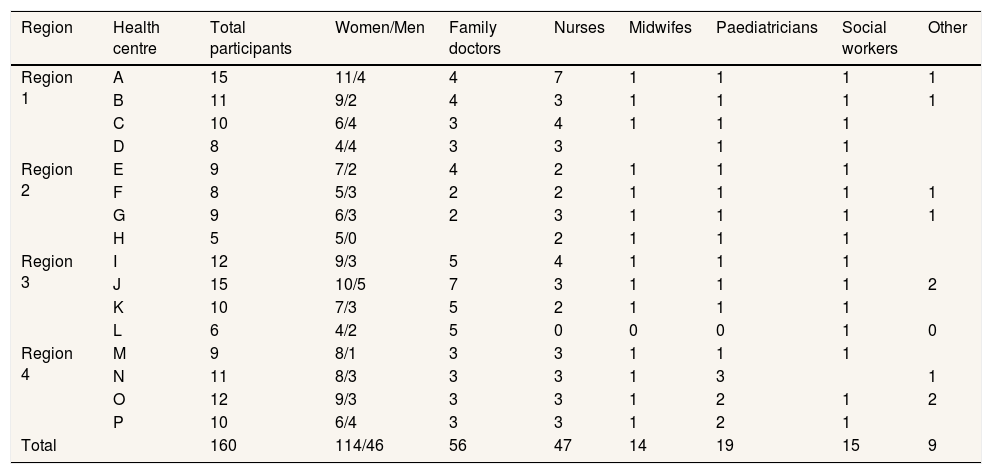
MethodsParticipants and data collectionFor this qualitative study, we conducted semi-structured individual interviews with 160 health professionals working in 16 PHCCs, located in four different regions. Semi-structured interviews allow to direct the issues to be covered, while at the same time is flexible enough to incorporate new emerging issues. It was also chosen to enhance homogeneity of data collection, since four interviewers were involved in this process. Professional backgrounds varied (Tables 1–3). The duration of the interviews ranged from 15minutes to more than one hour.
Number and main characteristics of interviewed primary health care professionals. Spain, 2013.
| Region | Health centre | Total participants | Women/Men | Family doctors | Nurses | Midwifes | Paediatricians | Social workers | Other |
|---|---|---|---|---|---|---|---|---|---|
| Region 1 | A | 15 | 11/4 | 4 | 7 | 1 | 1 | 1 | 1 |
| B | 11 | 9/2 | 4 | 3 | 1 | 1 | 1 | 1 | |
| C | 10 | 6/4 | 3 | 4 | 1 | 1 | 1 | ||
| D | 8 | 4/4 | 3 | 3 | 1 | 1 | |||
| Region 2 | E | 9 | 7/2 | 4 | 2 | 1 | 1 | 1 | |
| F | 8 | 5/3 | 2 | 2 | 1 | 1 | 1 | 1 | |
| G | 9 | 6/3 | 2 | 3 | 1 | 1 | 1 | 1 | |
| H | 5 | 5/0 | 2 | 1 | 1 | 1 | |||
| Region 3 | I | 12 | 9/3 | 5 | 4 | 1 | 1 | 1 | |
| J | 15 | 10/5 | 7 | 3 | 1 | 1 | 1 | 2 | |
| K | 10 | 7/3 | 5 | 2 | 1 | 1 | 1 | ||
| L | 6 | 4/2 | 5 | 0 | 0 | 0 | 1 | 0 | |
| Region 4 | M | 9 | 8/1 | 3 | 3 | 1 | 1 | 1 | |
| N | 11 | 8/3 | 3 | 3 | 1 | 3 | 1 | ||
| O | 12 | 9/3 | 3 | 3 | 1 | 2 | 1 | 2 | |
| P | 10 | 6/4 | 3 | 3 | 1 | 2 | 1 | ||
| Total | 160 | 114/46 | 56 | 47 | 14 | 19 | 15 | 9 | |
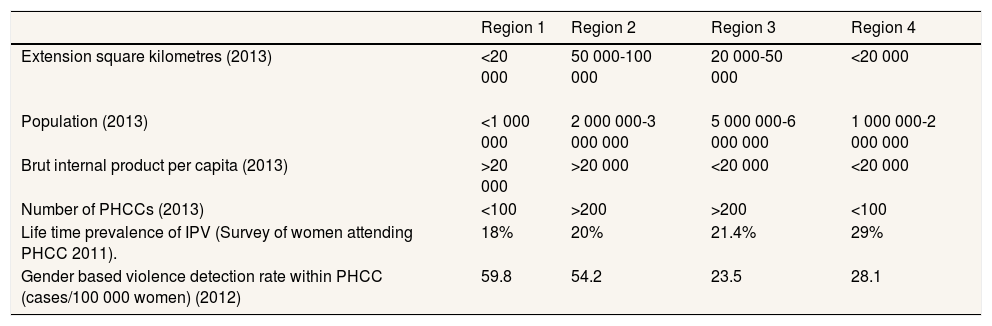
Selected characteristics of the studied autonomous regions. Spain.
| Region 1 | Region 2 | Region 3 | Region 4 | |
|---|---|---|---|---|
| Extension square kilometres (2013) | <20 000 | 50 000-100 000 | 20 000-50 000 | <20 000 |
| Population (2013) | <1 000 000 | 2 000 000-3 000 000 | 5 000 000-6 000 000 | 1 000 000-2 000 000 |
| Brut internal product per capita (2013) | >20 000 | >20 000 | <20 000 | <20 000 |
| Number of PHCCs (2013) | <100 | >200 | >200 | <100 |
| Life time prevalence of IPV (Survey of women attending PHCC 2011). | 18% | 20% | 21.4% | 29% |
| Gender based violence detection rate within PHCC (cases/100 000 women) (2012) | 59.8 | 54.2 | 23.5 | 28.1 |
IPV: intimate partner violence; PHCC: primary health care centres.
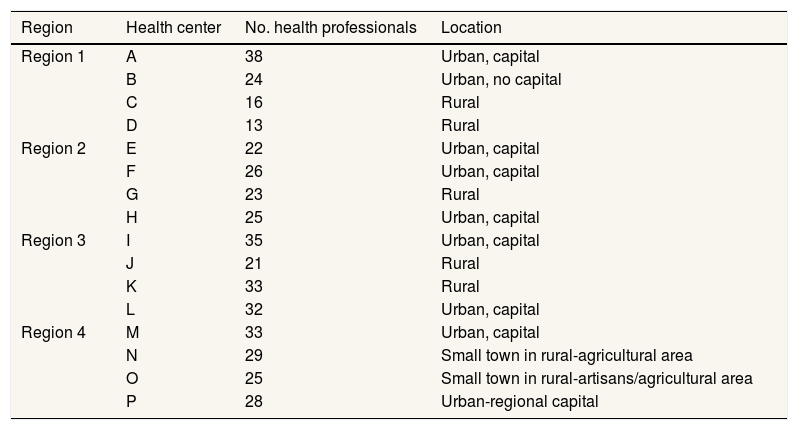
Selected characteristics of the studied primary health care centres teams. Spain, 2013.
| Region | Health center | No. health professionals | Location |
|---|---|---|---|
| Region 1 | A | 38 | Urban, capital |
| B | 24 | Urban, no capital | |
| C | 16 | Rural | |
| D | 13 | Rural | |
| Region 2 | E | 22 | Urban, capital |
| F | 26 | Urban, capital | |
| G | 23 | Rural | |
| H | 25 | Urban, capital | |
| Region 3 | I | 35 | Urban, capital |
| J | 21 | Rural | |
| K | 33 | Rural | |
| L | 32 | Urban, capital | |
| Region 4 | M | 33 | Urban, capital |
| N | 29 | Small town in rural-agricultural area | |
| O | 25 | Small town in rural-artisans/agricultural area | |
| P | 28 | Urban-regional capital |
Four of the authors conducted the interviews in Spanish from January 2013 until March 2014, which were digitally recorded and verbatim transcribed. The aspects explored included perceptions on the PHC team's response to IPV, how IPV had been integrated in teamwork, individual differences and involvement, and relationships within the team.
This study was part of a larger evaluation project exploring how to develop a health care response to IPV within 16 PHCC teams located in four different regions in Spain.14 In each PHCC we invited to participate in the interviews professionals from different backgrounds in order to have a broader perspective. During the interviews the relevance of the PHC approach for implementing a health-care response to IPV emerged strongly; we therefore decided to explore this issue further in the present study, following an emergent design.23
Data analysisFor this study, all the original transcriptions in Spanish were analyzed using qualitative content analysis,24 focusing on the connections (and disconnections) between the implementation of a PHC approach and the health-care response to IPV. After reading the interview transcripts several times, meaning units that referred to PHC approach and IPV response were identified, and codes were developed. Codes were grouped together to build categories and subcategories, that reflected the manifest content of the text.
Ethical approval for this study was granted by the Ethical Committee of the University of Alicante (Spain). The study was presented to the health teams participating. Written informed consent was sought from all of the participants in the study.
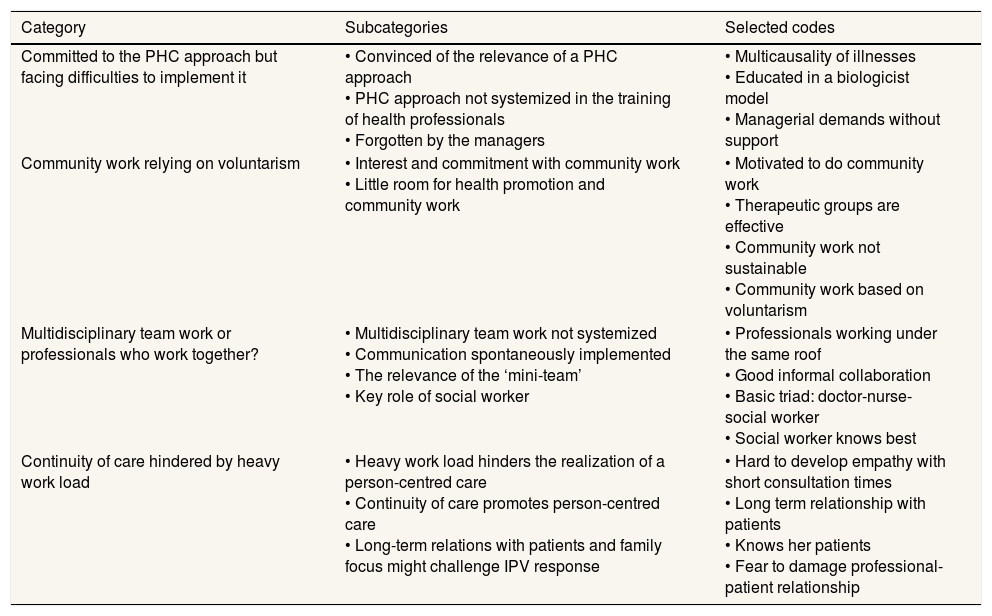
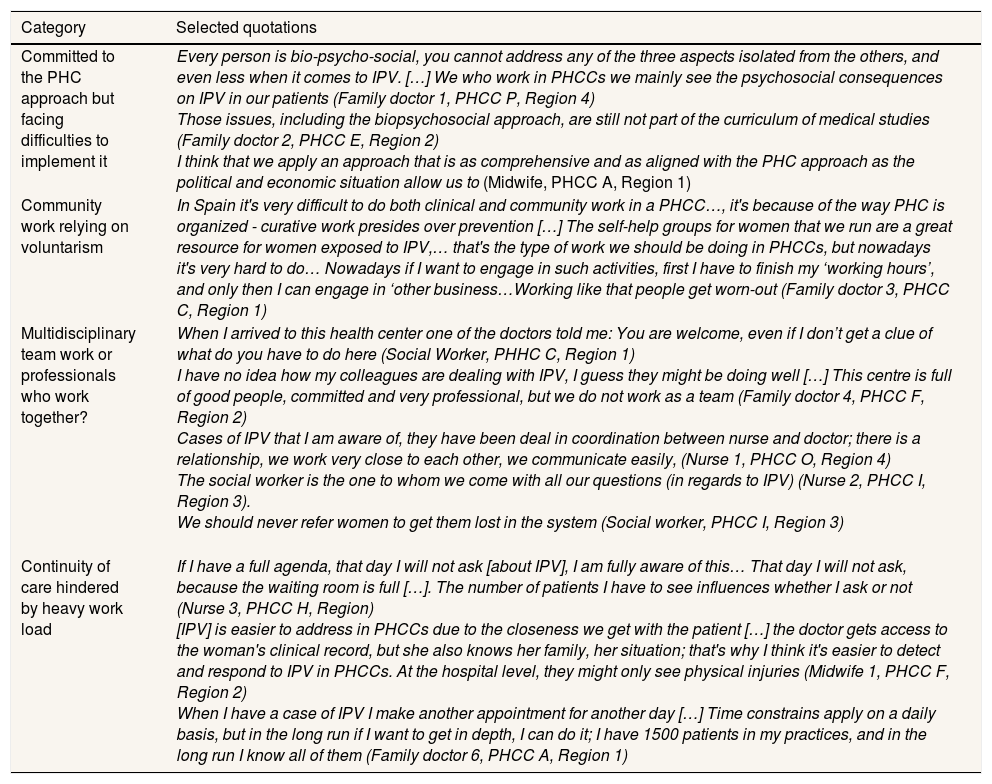
ResultsFrom the analysis of the interviews four categories emerged: Committed to the PHC approach but facing difficulties to implement it, Community work relying on voluntarism, Multidisciplinary team work, and Continuity of care hindered by heavy work load. Table 4 displays the categories, subcategories and selected codes, while Table 5 displays selected quotations for each category.
Categories, subcategories and selected codes emerging from the analysis of the interviews. Spain.
| Category | Subcategories | Selected codes |
|---|---|---|
| Committed to the PHC approach but facing difficulties to implement it | • Convinced of the relevance of a PHC approach • PHC approach not systemized in the training of health professionals • Forgotten by the managers | • Multicausality of illnesses • Educated in a biologicist model • Managerial demands without support |
| Community work relying on voluntarism | • Interest and commitment with community work • Little room for health promotion and community work | • Motivated to do community work • Therapeutic groups are effective • Community work not sustainable • Community work based on voluntarism |
| Multidisciplinary team work or professionals who work together? | • Multidisciplinary team work not systemized • Communication spontaneously implemented • The relevance of the ‘mini-team’ • Key role of social worker | • Professionals working under the same roof • Good informal collaboration • Basic triad: doctor-nurse-social worker • Social worker knows best |
| Continuity of care hindered by heavy work load | • Heavy work load hinders the realization of a person-centred care • Continuity of care promotes person-centred care • Long-term relations with patients and family focus might challenge IPV response | • Hard to develop empathy with short consultation times • Long term relationship with patients • Knows her patients • Fear to damage professional-patient relationship |
PHC: primary health care.
Categories and selected quotations.
| Category | Selected quotations |
|---|---|
| Committed to the PHC approach but facing difficulties to implement it | Every person is bio-psycho-social, you cannot address any of the three aspects isolated from the others, and even less when it comes to IPV. […] We who work in PHCCs we mainly see the psychosocial consequences on IPV in our patients (Family doctor 1, PHCC P, Region 4) Those issues, including the biopsychosocial approach, are still not part of the curriculum of medical studies (Family doctor 2, PHCC E, Region 2) I think that we apply an approach that is as comprehensive and as aligned with the PHC approach as the political and economic situation allow us to (Midwife, PHCC A, Region 1) |
| Community work relying on voluntarism | In Spain it's very difficult to do both clinical and community work in a PHCC…, it's because of the way PHC is organized - curative work presides over prevention […] The self-help groups for women that we run are a great resource for women exposed to IPV,… that's the type of work we should be doing in PHCCs, but nowadays it's very hard to do… Nowadays if I want to engage in such activities, first I have to finish my ‘working hours’, and only then I can engage in ‘other business…Working like that people get worn-out (Family doctor 3, PHCC C, Region 1) |
| Multidisciplinary team work or professionals who work together? | When I arrived to this health center one of the doctors told me: You are welcome, even if I don’t get a clue of what do you have to do here (Social Worker, PHHC C, Region 1) I have no idea how my colleagues are dealing with IPV, I guess they might be doing well […] This centre is full of good people, committed and very professional, but we do not work as a team (Family doctor 4, PHCC F, Region 2) Cases of IPV that I am aware of, they have been deal in coordination between nurse and doctor; there is a relationship, we work very close to each other, we communicate easily, (Nurse 1, PHCC O, Region 4) The social worker is the one to whom we come with all our questions (in regards to IPV) (Nurse 2, PHCC I, Region 3). We should never refer women to get them lost in the system (Social worker, PHCC I, Region 3) |
| Continuity of care hindered by heavy work load | If I have a full agenda, that day I will not ask [about IPV], I am fully aware of this… That day I will not ask, because the waiting room is full […]. The number of patients I have to see influences whether I ask or not (Nurse 3, PHCC H, Region) [IPV] is easier to address in PHCCs due to the closeness we get with the patient […] the doctor gets access to the woman's clinical record, but she also knows her family, her situation; that's why I think it's easier to detect and respond to IPV in PHCCs. At the hospital level, they might only see physical injuries (Midwife 1, PHCC F, Region 2) When I have a case of IPV I make another appointment for another day […] Time constrains apply on a daily basis, but in the long run if I want to get in depth, I can do it; I have 1500 patients in my practices, and in the long run I know all of them (Family doctor 6, PHCC A, Region 1) |
The participants in this study were convinced of the importance of implementing a PHC approach in general and, specifically in regards to IPV. Participants considered that the patient/person was at the core of the PHC approach. This implied that health professionals should not only ‘fix’ the health problem that brought each patient to the health centre but also explore the psychological and emotional spheres and the social context, in order to best respond to her/his health needs. They considered that such an approach facilitated the detection of IPV and promoted a better response (Table 5).
However, participants complained that health professionals received more training in a biomedical approach and far less training on the principles and attributes of the PHC approach. As a consequence, health professionals felt they were less prepared to respond to health problems with a strong social and/or emotional component, such as IPV (Table 5).
Despite policies and programs that promote PHC, participants felt that a lot of demands were put on them while the working environment did not support their efforts to implement a PHC approach in their everyday practice (Table 5).
Faced with such a discouraging environment, some of the participants felt dispirited while others engaged in initiatives to improve the PHC competencies of health professionals, through engaging in medical associations, training medical residents, etc.
Community work relying on voluntarismFive of the visited PHCC were implementing health promotion or community-based initiatives related with IPV prevention, such as self-help groups with women. In all of those centres, the medical coordinator facilitated such activities, although sometimes conflicts emerged when colleagues had to ‘cover’ for professionals who were engaged in community/health promotion work.
Participants acknowledged that such initiatives were implemented and sustained through the personal interest and commitment of a group of professionals, usually headed by the social worker. If such professionals got tired or moved to another centre, then the initiatives got discontinued. They identified a number of barriers for sustaining the community-orientation of the PHC approach: workload, scarce and unequal support from the managerial level, the consideration of community work as optional, the fact that health care professionals might neither be well prepared nor accustomed to engage in such activities (Table 5).
Multidisciplinary team work or professionals who work together?The interviewed health professionals considered that health policies and programs in Spain put emphasis on the importance of team work and multidisciplinarity. However, they considered that there was a gap between such policies and their implementation, since structures to promote and facilitate work as multidisciplinary teams have failed to be sustained as part of the routines of the health professionals. Professionals’ hierarchies were also considered a barrier to work as a multidisciplinary team. The expertise of certain professionals like physiotherapists, midwives and nurses was not as valued as that of medical doctors. In certain health centers, social workers complained about the scarce knowledge and recognition of their expertise (Table 5).
Continuous references were made to a very individualistic style of work, in which it was difficult for professionals to know how their colleagues were responding to IPV or to other health problems (Table 5).
Due to the lack of guidelines structuring the work of multidisciplinary teams, professionals pointed out that team work had to rely on the good communication and relationships between the colleagues at an informal level. Communication during coffee-breaks, knocking on the door of a colleague to discuss particular cases, or informal meetings were opportunities to discuss issues that emerged during consultations, including IPV cases.
The health professionals participating in this study acknowledged the key role of what they called the mini-team, namely the family doctor and nurse who were assigned to the same patient. Coordination with paediatricians or midwifes, was more erratic and strongly dependent on the personal interest of certain professionals. On the contrary the existence of a social worker within the team was considered as a cornerstone for responding to IPV due to their expertise on this and other issues considered ‘social’ (Table 5).
The most committed professionals warned of the risks of reducing multidisciplinary work to “referring” patients as a way to getting rid of them. They firmly supported that once a woman disclosed IPV with a professional, she or he should stay with her, and refer only when the woman wanted to (Table 5).
Continuity of care hindered by heavy work loadParticipants complained about how work load and short consultation times hindered the implementation of person-centred care as well as threatened the coordination of services. They felt that this was especially deleterious for the detection and response to IPV.
Despite the work overload, participants acknowledged that the way PHC centres work in Spain facilitated the establishment of relationships of trust between health professionals and patients, and such relationships were perceived as enhancing the likelihood of detecting and disclosing IPV. Participants also mentioned that the short consultation times were somehow compensated by continuity over time.
However, this long-term relationship established with patients was considered by some participants as an obstacle to the detection of IPV due to over-confidence on ‘knowing everything about their patients’ or fear of breaking a good professional-patient relationship by bringing up a sensitive topic. The family focus of the PHCCs as well as the fact that families are usually assigned to the same health professionals allowed a broader knowledge of the situation of each patient. However, this characteristic became a challenge in cases of IPV, when the same health professional was assigned to both the victim and the aggressor. This situation brought complications in terms of security, confidentiality and/or the emotional burden.
DiscussionThis study captures both professionals’ perceptions on the current (weak) presentation of PHC attributes in Spain and their views on how such attributes, when actually present, can promote a comprehensive response to IPV.
In line with our findings, other studies evidence that a PHC approach facilitates the integration of healthcare responses to complex health problems, i.e. mental health.25 Previous studies in Spain support the importance of the PHC approach as a relevant condition triggering better responses to IPV.13,14 However, participants also acknowledged the challenges to sustain the PHC approach in Spain due to the weak training provided both during undergraduate studies and in-service. Moreover, the implementation of a person-centred bio-psycho-social approach might risk focusing on solutions at the individual level, while the root of many health problems in general and IPV in particular lies mainly at the broader social level.26
Complaints about the effect of health care austerity measures on the work load of primary health care teams in Spain have been reported in other studies.20 This study describes how health care professionals perceived their deleterious effect for the sustainability of the PHC attributes and for responding to IPV. However, such complains could also represent ways to justify evading responsibilities, in an issue that remains controversial. One cannot forget that the health system reproduces the gender order of a given society, strongly influencing professionals’ practices, attitudes and priorities.27,28
Community-orientation is commonly recognized as one of the most challenging attributes to achieve when implementing a PHC approach within health systems.8,16 Previous studies in Spain show that this attribute has been not in focus within the Spanish PHC in general, and even less in regards to IPV.29 Lack of support from the managerial level and the fact that community work has not been included within the objectives evaluated annually have been mentioned as hindering community-orientation of PHC in Spain.30,31 This study coincides with these findings but also points out another key issue: community work in relation with IPV is considered important and PHC teams do engage in such initiatives, although in a voluntary basis, very much depending on individual professionals’ commitment, which makes work hard to sustain. As the WHO guidelines point out, a health care response should involve not only detection and referral, but also preventive and community work.7 Such work can contribute to professionals’ perceived self-efficacy in dealing with IPV, since they might feel that they have ‘something to offer’.13,14 The existence of various community activities and localized initiatives to promote community work might facilitate changes towards a stronger community-orientation.32,33
Multidisciplinary team work is important to offer an IPV response centred on the diverse needs of women exposed to IPV1,7; i.e., the nurse and medical doctor can detect and follow up, the social worker can work therapeutically and connect the woman with other resources, the paediatrician can explore the effects of IPV on her children. The organization of the Spanish PHC services allows patients to meet different professionals in the same facility; the integration of social workers within PHC teams seems especially relevant for offering a comprehensive health care response to IPV and for connecting the PHCC with other resources. However, the mere existence of different professions under the same roof does not ensure that cases of IPV receive a multidisciplinary and coordinated response. In order to do so, team-supporting structures should be developed, establishing clear goals, division of labor, training of team members in their personal roles and in team functioning. Such structures appeared to be weak in Spain, and were too dependent on professionals’ voluntarism, which hinders their sustainability and effectiveness. A review of facilitators and barriers to inter-professional collaboration pointed out that perceived hierarchy was the main conceptual barrier hindering collaboration, which was also pointed out in our study and others.27,34 Multidisciplinary training could facilitate change on health professionals’ perceptions and enhance awareness of each other's roles.34
The most committed professionals in this study also highlighted the importance of building and keeping trust with women who disclose IPV and that referring or consultation with other professionals should not become an easy scape. Building trust is also mentioned as part of the WHO recommendations.7
This study showed that the way PHCCs are organized in Spain allows longitudinal continuity and ensures the establishment of long term relationship with patients that, to a certain extent, compensate for the short(ening) consultation times. On the one hand, the findings from this study coincide with other studies that show that building trust relationships between health professionals and women exposed to IPV is key in order to improve IPV detection and response.4,5 On the other hand, this study also points out that close relationships between professionals and patients might prevent detection due to over confidence or fear of damaging the relationship from the point of view of the professional. The family-focused PHCCs in Spain might enhance professionals’ knowledge of the patient's situation but also possesses great challenges to the implementation of IPV responses; i.e. safety for both the professionals and the victims might be put at risk. It is important to note that the WHO guidelines fail to address this aspect thoroughly.7
This study was based in a specific setting, Spain, a country with a decentralized and universal public health system, an extensive network of PHCCs, and where health policies against IPV have flourished. These characteristics are shared by a number of Western EU countries, and thus our results may be transferable to them.
As we have described before, this research was part of a larger study in which exploring the linkage between the attributes of PHC and IPV was not the main focus; thus, we may have failed to inquire in greater depth on relevant issues. However, the central role of the PHC attributes in shaping PHC team responses to IPV, and the challenges to sustaining such attributes emerged from the data, and this was what motivated this study. We argue that following an emergent design adds to the study's dependability, which contributes to research trustworthiness.23
Since the participation was voluntary it is likely that the sample over represents the perceptions of those professionals more sensitized with IPV. The higher proportion of women in the sample might reflect this as well. However, an effort was made to invite professionals who were more skeptical with the topic, although this was not always successful.
Due to the study design we cannot claim that a causal relation exists between PHC attributes and IPV responses. However, we consider that this study is a first step for improving our understanding on how PHC attributes can contribute to better health care responses to IPV and the complexity of their implementation in the day to day practices of PHCC teams.
The implementation of primary health care attributes −person/family-centred, longitudinal, comprehensive, coordinated and community oriented− facilitates the implementation of interventions against complex problems.
What does this study add to the literature?Health care professionals perceived that a primary health care approach facilitates more comprehensive responses to intimate partner violence, but existing health system's structures were not conducive. In order to implement more comprehensive and sustainable health care responses to intimate partner violence, health systems should strengthen the realization of the primary health care attributes.
María Teresa Ruiz Cantero.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsI. Goicolea was the PI in this project, proposed the idea for this manuscript, organized the structure and developed the first draft. E. Briones-Vozmediano, L. Otero-Garcia and M. Garcia have been involved in the entire project, participated in data collection and analysis and have critically revised successive manuscripts. P. Mosquera and C. Vives-Cases have been involved in the entire project, have participated in the analysis of the data have critically revised the successive manuscripts. All authors have approved the final version of the manuscript and all agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FundingThis study has been funded through a COFAS grant (supported by COFUND action within the Marie Curie Action People, in the Seventh Framework programme and the Swedish Council for Working Life and Social Research/FAS-Forskningsradet för arbetsliv och socialvetenskap) through a competitive call. This work was partly supported by the Umeå Center for Global Health Research, funded by FAS, the Swedish Council for Working Life and Social Research (Grant no. 2006-1512).
Conflicts of interestThe authors declare that there is no conflict of interest. One of the authors (E. Briones-Vozmediano) belongs to the Gaceta Sanitaria editorial committee, but was not involved in the editorial process of the manuscript.
The authors are grateful to the Observatory of Women's Health of the Spanish Ministry of Health, and to the professionals in charge of IPV programs within the regional health system for facilitating access to relevant information and contacts. The authors are especially grateful to the primary health care teams and to the women patients who participated in this study, who shared their time, enthusiasm, experiences and expertise, and facilitated access to unpublished information.