To identify the characteristics of chronic patients and their environment in order to predict the nursing workload required 1 year after their inclusion in a home care program.
MethodsA longitudinal study was carried out in 72 primary health care teams in Catalonia (Spain) with a 1-year follow-up of 1,068 home care patients over 64 years old. The variables collected from each patient included data on health and social status (Charlson and Barthel indexes and the Pfeiffer, Braden and Gijon scales), carer overburden (Zarit scale), hospital admissions, use of emergency services, self-perceived health (SF-12) and the number of health worker visits.
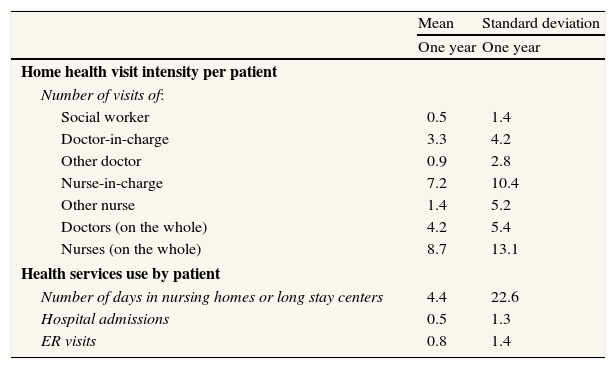
ResultsPatients received 7.2 (SD 10.4) visits per year from their nurse-in-charge, out of a total of 8.7 (SD 13.1) nursing visits per year. Risk factors for receiving more nursing visits at home were male gender (IRR=1.42, 95%CI: 1.20-1.67), dependency for daily activities (IRR=1.65, 95%CI: 1.29-2.13), decubitus ulcers (IRR=4.03, 95%CI: 2.27-7.14) and receiving emergency medical care at home (IRR=1.65, 95%CI: 1.31-2.07). In contrast, patients with major cognitive impairment (IRR=0.78, 95%CI: 0.63-0.98) had a lower probability of receiving nursing visits at home.
ConclusionsWorkload can be predicted by patients’ clinical characteristics. The positive correlation of workload with variables related to disease severity and the negative correlation with variables related to cognitive impairment show that home care nursing in Catalonia is basically demand-oriented.
Identificar las características basales de los pacientes crónicos y su entorno que predicen la carga de trabajo de enfermería durante el año siguiente a su inclusión en un programa de atención domiciliaria (ATDOM).
MétodosEstudio longitudinal realizado en 72 equipos de atención primaria de salud en Cataluña. Seguimiento durante un año de 1068 pacientes de ATDOM mayores de 64 años de edad. Variables recogidas: nivel de salud y situación social (test de Charlson, Barthel, Pfeiffer, Braden y Gijón); sobrecarga del cuidador (Test de Zarit); ingresos hospitalarios y visitas a urgencias; estado subjetivo de salud (SF-12); visitas de los profesionales de salud.
ResultadosLos pacientes recibieron 7,2 (DE: 10,4) visitas anuales de su enfermera habitual. Observamos que tienen más riesgo de recibir visitas de enfermería los pacientes varones (IRR=1,42, IC95%: 1,20-1,67), con dependencia para las actividades de la vida diaria (IRR=1,65, IC95%: 1,29-2,13), afectados por úlceras por decúbito (IRR=4,03, IC95%: 2,27-7,14) y que precisaron servicios de atención de urgencia a domicilio (IRR=1,65, IC95%: 1,31-2,07). Por otro lado, los pacientes con deterioro cognitivo importante tienen menos probabilidad de recibir visitas de su enfermera (IRR=0,78, IC95%: 0,63-0,98).
ConclusionesLas características clínicas de los pacientes permiten predecir la carga de trabajo de enfermería. Esta relación positiva de la carga de trabajo con las variables relacionadas con la gravedad de la enfermedad y la relación negativa con el deterioro cognitivo muestra que la enfermería domiciliaria en Cataluña está básicamente orientada a la demanda.
The development of home care programs in Catalonia (Spain) has been favored by increased life expectancy, changes in the traditional Mediterranean family structure, reduced length of hospital stay, and the shortage of nursing homes and long term hospital wards, combined with the desire of the elderly to continue living in the community. This region of Spain has a National Health Service that provides healthcare to all citizens free of charge at the moment of delivery. A total of 340 teams, covering a geographically delimited area from 5 to 25 thousand inhabitants each, provide primary care. Each team carries out a home care program intended for patients who cannot visit the health center to receive primary care services. As in other developed countries, nurses lead the home care programs1. In Catalonia, primary care nurses devote 5h a week to this activity, twice the time devoted by physicians and social workers2. As care providers, nurses play a central role in promoting health, reducing functional status impairment and ensuring the continuity of care by the different health professionals who provide services to these patients3.
Because of the large volume of resources allocated to this program and the need to rationalize the nursing workforce, current practices and the factors that affect the nursing workload must be evaluated, even though measuring the role of nursing care is extremely difficult, given the complex, multitasking characteristics of this work4.
Several factors related to disease severity and comorbidity have been identified as being associated with nursing workload, although these results are very much influenced by the nursing organization system used and by the patients’ needs assessment carried out by the nurses5–7. However, the majority of these studies were carried out in cultures and health services that differ substantially from Catalan services1,8–10. To plan future nursing activity and identify opportunities for improvement, the programs currently used in Catalonia must be evaluated. The purpose of our study was to identify the variables that would allow us to predict the nursing workload needed to treat patients 1 year after admission to a home care program. These variables were based on the characteristics of patients over 64 years of age, their families and the health and social services they received. This information may be of great help to primary care teams in predicting nursing requirements after initial patient assessment.
MethodsThe methodology of this longitudinal study can be consulted in Gené et al11. The current analysis is based on the data from the initial assessment and the first year of follow-up.
The patient inclusion criteria were as follows: non-institutionalized chronic patients over 64 years of age who were unable to travel to the primary healthcare center to seek healthcare and who had been included in a home care program from July 1 to December 31, 2005 or patients who, during this inclusion period, had already been in the program for less than 12 months.
The patient exclusion criteria were the following: patients who refused to participate, transitory patients (followed-up by the team for less than 9 months/year), patients with a life expectancy of less than 4 months (according to the healthcare professional's prognosis), patients provided temporary care after surgery and those with dementia whose carers also had dementia (hampering data collection).
Data collectionFor patient recruitment purposes, each of the 378 primary healthcare professionals (general practitioners, nurses and social workers) who agreed to participate in the study randomly selected an average of three patients who fulfilled the inclusion criteria. Each health professional participating in the study acted as a collaborative researcher and was responsible for administering the questionnaires used in the study and for the gathering the necessary patient information from the clinical visit, clinical records and reports from other healthcare providers.
The following data were collected from each patient: comorbidity level (Charlson index) 12, functional status (Barthel index) 13, cognitive status (Pfeiffer scale) 14, presence of decubitus ulcers, risk of development of ulcers (Braden scale) 15, subjective health status (SF-12) 16, social risk (Gijon social scale) 17, use of health services (palliative care, home care rehabilitation and others), formal and informal social help (home help, teleassistance, meal on wheels, volunteer care, day center stays and others) and carer burden (Zarit scale) 18. Data on hospital admissions, emergency room visits and home emergency visits were extracted from the patients’ clinical records by the collaborative researchers. During the first year after recruitment, we collected data on visits by primary healthcare personnel (general practitioner, nurses and social workers). All the above-mentioned questionnaires have been validated to enable their use in the Spanish context.
Researchers participating in the study received training for data collection standardization. Data were analyzed centrally. A continuous data quality assurance process was carried out to minimize errors and information loss. A research team member validated 10% of the data gathered by collaborative researchers from the patients’ original clinical records.
Sample sizeWe used Granmo software to perform the sample size calculations (cohort studies and relative risk option). Although our objective was not to focus exclusively on the exposure variable ‘presence of decubitus ulcers’, we had to choose a reference exposure variable for the sample size calculation. We agreed to choose this ‘decubitus ulcer variable’ because it was recognized in the literature as the item most closely related to nursing activity19. Accepting an alpha risk of 0.05 and a beta risk of 0.20 in a bilateral contrast, 116 patients were needed in the exposed group (with decubitus ulcers) and 707 in the unexposed group to detect a minimum relative risk of 1.3, with a disease ratio of 0.5 in the unexposed group, expecting a proportion of missing values of 10%.
Statistical analysisQualitative variables were described by frequency tables and quantitative variables by the mean and the standard deviation. The dependent variable used in our study was nursing visits in the first year of follow-up. We used the variables collected in the initial assessment to predict nursing visits received by patients the following year.
Our dependent variable of nursing visits followed a Poisson distribution. A negative binomial model20 was required because of data overdispersion. In the bivariate analysis we selected the variables with a p<0.10 and added other important variables to these variables in the multivariate model. Because the time between the first and second data collections was not constant, an offset parameter was included in the model.
The statistical analysis was carried out using the SPSS 13 program (univariate analysis) and STATA 9.1 (bivariate and multivariate analysis).
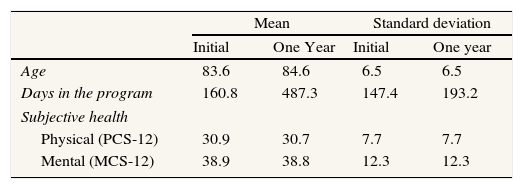
ResultsOf the 1,068 patients enrolled in the study, 1,002 were followed-up for a year. Patient characteristics are shown in Table 1. The characteristics of the 66 patients that did not complete the follow-up were not significantly different from those of the remaining patients. The proportion of patients with severe dependency, cognitive impairment, social problems and risk of decubitus ulcers increased in the follow-up year. However, comorbidity and self-perceived health did not vary significantly during this period. Tobacco and alcohol consumption decreased and almost 20% of the patients died.
Patient characteristics at initial assessment (N=1,068) and after 1 year of follow-up (N=1002).
| Mean | Standard deviation | |||
| Initial | One Year | Initial | One year | |
| Age | 83.6 | 84.6 | 6.5 | 6.5 |
| Days in the program | 160.8 | 487.3 | 147.4 | 193.2 |
| Subjective health | ||||
| Physical (PCS-12) | 30.9 | 30.7 | 7.7 | 7.7 |
| Mental (MCS-12) | 38.9 | 38.8 | 12.3 | 12.3 |
| Frequency | % | |||
| Initial | One year | Initial | One year | |
| Women | 710 | 659 | 66.5 | 66.2 |
| Comorbidity | ||||
| Charlson | ||||
| 0 | 173 | 136 | 16.2 | 16 |
| 1 | 268 | 207 | 25.1 | 24.3 |
| 2 or more | 622 | 508 | 58.7 | 59.7 |
| Dependency level | ||||
| Total dependence | 113 | 118 | 10.6 | 13.7 |
| (Barthel index) | ||||
| Severe dependence | 73 | 77 | 6.8 | 8.9 |
| Moderate dependence | 197 | 144 | 18.5 | 6.7 |
| Low dependence | 616 | 480 | 57.7 | 55.7 |
| Autonomous | 68 | 43 | 6.4 | 5 |
| Cognitive status | ||||
| Normal | 566 | 397 | 53.1 | 48.8 |
| (Pfeiffer scale) | ||||
| Low deterioration | 194 | 148 | 18.2 | 18.2 |
| Moderate deterioration | 164 | 120 | 15.4 | 14.7 |
| Serious deterioration | 142 | 149 | 13.3 | 18.3 |
| Ulcer risk | ||||
| High | 49 | 58 | 4.6 | 6.8 |
| (Braden scale) | ||||
| Moderate | 86 | 72 | 8.1 | 8.4 |
| Low | 922 | 724 | 87.3 | 84.8 |
| Ulcers | ||||
| No presence | 924 | 794 | 86.5 | 86.4 |
| Social Risk | ||||
| No social risk | 534 | 400 | 50.7 | 48.8 |
| (Gijon scale) | ||||
| Social Risk | 391 | 314 | 37.1 | 38.3 |
| Social problems | 128 | 105 | 12.2 | 12.8 |
| Toxic habits | ||||
| Non-smoker | 1034 | 891 | 96.8 | 97.1 |
| Abstains from alcohol | 977 | 858 | 91.5 | 93.8 |
| Program discharge | ||||
| Death at home | 83 | 27 | ||
| Death at hospital | 112 | 36.5 | ||
| Definitive admission to a nursing home | 49 | 16 | ||
| Change of address | 28 | 9.1 | ||
| Other | 35 | 11.4 | ||
Cases with missing values were not included in the analysis.
PCS-12: Physical Component Summary of the 12-item Short Form Health Survey; MCS-12: Mental Component Summary of the 12-item Short Form Health Survey.
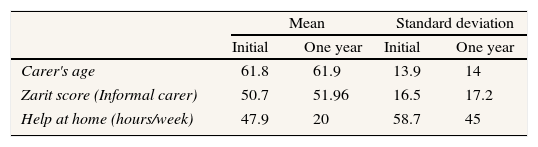
Table 2 shows carer characteristics at the initial assessment and 1 year later. Table 3 shows the use of health and social services by the patients in the study during the 1-year follow-up. The number of women acting as informal carers increased, as did perceived carer burden and formal home care.
Carer characteristics at initial assessment (N=1068) and after 1 year of follow-up (N=1002).
| Mean | Standard deviation | |||
| Initial | One year | Initial | One year | |
| Carer's age | 61.8 | 61.9 | 13.9 | 14 |
| Zarit score (Informal carer) | 50.7 | 51.96 | 16.5 | 17.2 |
| Help at home (hours/week) | 47.9 | 20 | 58.7 | 45 |
| Frequency | % | |||
| Initial | One year | Initial | One year | |
| With informal carer | 879 | 739 | 82.3 | 82.5 |
| With home help | 401 | 360 | 37.5 | 39.7 |
| Informal carer women | 673 | 595 | 63.0 | 78.3 |
| Level of carer overload (Zarit score) | ||||
| No carer overload | 378 | 277 | 43.7 | 42.1 |
| Low overload | 186 | 128 | 21.5 | 19.5 |
| Heavy overload | 301 | 253 | 34.8 | 38.4 |
Cases with missing values were not included in the analysis.
Health and social services use (initial and at 1 year of follow-up) (N=1068 and N=1002).
| Mean | Standard deviation | |
| One year | One year | |
| Home health visit intensity per patient | ||
| Number of visits of: | ||
| Social worker | 0.5 | 1.4 |
| Doctor-in-charge | 3.3 | 4.2 |
| Other doctor | 0.9 | 2.8 |
| Nurse-in-charge | 7.2 | 10.4 |
| Other nurse | 1.4 | 5.2 |
| Doctors (on the whole) | 4.2 | 5.4 |
| Nurses (on the whole) | 8.7 | 13.1 |
| Health services use by patient | ||
| Number of days in nursing homes or long stay centers | 4.4 | 22.6 |
| Hospital admissions | 0.5 | 1.3 |
| ER visits | 0.8 | 1.4 |
| Frequency | % | |||
| Initial | One year | Initial | One year | |
| Visits to other health services in the previous year | ||||
| Number of visits of: | ||||
| PADES (palliative services) | 31 | 40 | 2.9 | 4.3 |
| 061 (ER ambulance services) | 146 | 206 | 13.7 | 22.5 |
| Private health services | 76 | 78 | 7.1 | 8.5 |
| Hospital at home service | 4 | 20 | 0.4 | 2.2 |
| ER visits at home | 121 | 115 | 11.3 | 12.4 |
| Day hospital | 22 | 24 | 2.1 | 2.6 |
| Home rehabilitation | 103 | 78 | 9.6 | 8.5 |
| Social services visits in the previous year | ||||
| Help at home (private) | 401 | 360 | 37.5 | 39.7 |
| Telephone assistance | 88 | 134 | 8.2 | 14.9 |
| Food delivery services | 10 | 11 | 0.9 | 1.2 |
| Volunteers | 14 | 22 | 1.3 | 2.4 |
| Day centers | 15 | 15 | 1.4 | 1.7 |
Cases with missing values were not included in the analysis.
ER: emergency room.
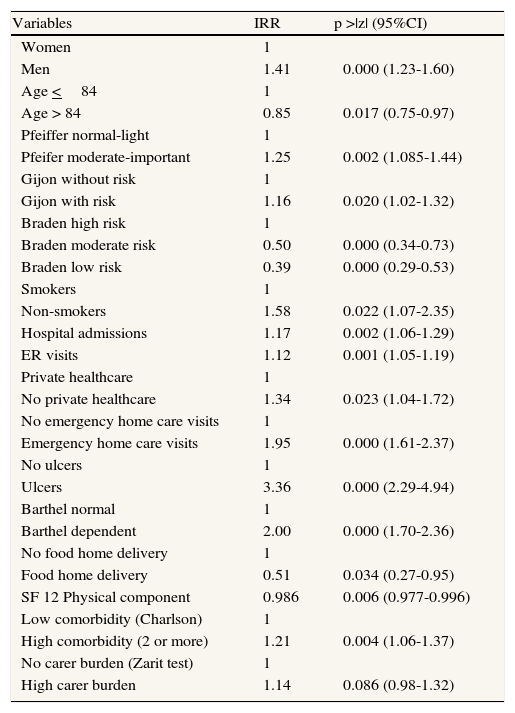
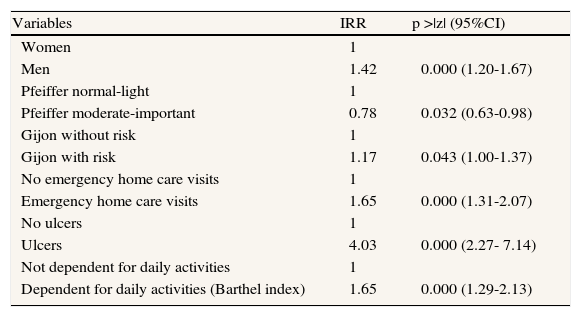
Table 4 displays the results of the bivariate analysis, showing the relationship between the patients’ characteristics at the initial assessment and the nursing workload in the following year. The results of the multivariate analysis are shown in Table 5. Patients with ulcers had a four-fold higher risk of receiving nursing home visits the year after their inclusion in the program. The probability of receiving more nursing visits the following year increased by 40% in men, 65% in patients dependent for daily activities, 20% in those with social problems, and 65% in those who received emergency home visits prior to the initial assessment. In contrast, patients with major cognitive impairment had a lower probability of receiving nursing visits at home.
Initial patient characteristics associated with nursing visits in the subsequent year: bivariate analysis.
| Variables | IRR | p >|z| (95%CI) |
| Women | 1 | |
| Men | 1.41 | 0.000 (1.23-1.60) |
| Age <84 | 1 | |
| Age > 84 | 0.85 | 0.017 (0.75-0.97) |
| Pfeiffer normal-light | 1 | |
| Pfeifer moderate-important | 1.25 | 0.002 (1.085-1.44) |
| Gijon without risk | 1 | |
| Gijon with risk | 1.16 | 0.020 (1.02-1.32) |
| Braden high risk | 1 | |
| Braden moderate risk | 0.50 | 0.000 (0.34-0.73) |
| Braden low risk | 0.39 | 0.000 (0.29-0.53) |
| Smokers | 1 | |
| Non-smokers | 1.58 | 0.022 (1.07-2.35) |
| Hospital admissions | 1.17 | 0.002 (1.06-1.29) |
| ER visits | 1.12 | 0.001 (1.05-1.19) |
| Private healthcare | 1 | |
| No private healthcare | 1.34 | 0.023 (1.04-1.72) |
| No emergency home care visits | 1 | |
| Emergency home care visits | 1.95 | 0.000 (1.61-2.37) |
| No ulcers | 1 | |
| Ulcers | 3.36 | 0.000 (2.29-4.94) |
| Barthel normal | 1 | |
| Barthel dependent | 2.00 | 0.000 (1.70-2.36) |
| No food home delivery | 1 | |
| Food home delivery | 0.51 | 0.034 (0.27-0.95) |
| SF 12 Physical component | 0.986 | 0.006 (0.977-0.996) |
| Low comorbidity (Charlson) | 1 | |
| High comorbidity (2 or more) | 1.21 | 0.004 (1.06-1.37) |
| No carer burden (Zarit test) | 1 | |
| High carer burden | 1.14 | 0.086 (0.98-1.32) |
IRR: incidence relative risk; 95%CI: 95% confidence interval of the IRR; SF12: 12-item Short Form Health Survey; ER: emergency room.
Cases with missing values are not included in the analysis.
Initial patient characteristics associated with nursing visits in the subsequent year. Multivariate analysis: negative binomial model (N=890).
| Variables | IRR | p >|z| (95%CI) |
| Women | 1 | |
| Men | 1.42 | 0.000 (1.20-1.67) |
| Pfeiffer normal-light | 1 | |
| Pfeiffer moderate-important | 0.78 | 0.032 (0.63-0.98) |
| Gijon without risk | 1 | |
| Gijon with risk | 1.17 | 0.043 (1.00-1.37) |
| No emergency home care visits | 1 | |
| Emergency home care visits | 1.65 | 0.000 (1.31-2.07) |
| No ulcers | 1 | |
| Ulcers | 4.03 | 0.000 (2.27- 7.14) |
| Not dependent for daily activities | 1 | |
| Dependent for daily activities (Barthel index) | 1.65 | 0.000 (1.29-2.13) |
IRR: incidence relative risk; 95%CI: 95% confidence interval of the IRR.
Cases with missing values are not included in the analysis.
Home care patients in Catalonia receive an average of nine nurse visits per year with high variability among patients. The cohort assessment showed that the number of visits can be predicted by the patient characteristics identified at the initial assessment. The risk of receiving more nursing visits increased particularly in patients with decubitus ulcers, men, those dependent for daily activities, patients with social problems and those who received emergency visits at home prior to the initial assessment. In contrast, people with major cognitive impairment had a lower probability of receiving home visits from nurses.
The absence of standardized procedures for home care nursing in Catalonia favors variability and implies that current practices are more due to patient and environment characteristics than to a standardized intervention program with different healthcare providers. The research methodology does not allow us to see the sample as representative of the home care provided in Catalonia because the researchers joined the study voluntarily and were not randomly selected. However, the large sample size, the diversity of providers, the even geographical distribution of the primary healthcare teams and the quality of the data collected make this study the best available description of the home care provided in Catalonia. Although the number of visits cannot be an accurate measurement of nursing professionals’ performance, its universality and simplicity make it a good indicator of nursing workload. This indicator does not accurately reflect variations in consultation length due to the different procedures carried out, but clearly measures the number of patients that a nurse can care for per day. In home care, a high percentage of working time is spent travelling, particularly in rural areas. Our results may not predict the precise workload needed for a single patient but can help us to plan the human resources needed to cover a defined population.
The presence of decubitus ulcers is the variable that most strongly predicts the number of home care nursing visits in the subsequent year. Decubitus ulcers are related to deterioration in health and are consequently associated with more clinical care19,21. In our study, the risk of receiving nursing visits in the following year was four times greater in patients with decubitus ulcers at the initial assessment than in those without. The incidence of decubitus ulcers in bedridden patients is a clear indicator of the quality of nursing care, although the prevalence of ulcers in home care patients predicts the nursing workload22.
As other authors have found, male patients receive more home care nursing visits23. Although gender inequalities in access to healthcare services have been identified in Catalonia24, the additional activity observed in the study might be explained by the higher morbidity of the elderly male population25,26 and informal carer demand. In our sample, men were less healthy than women, even though on average they were younger. Male patients also benefitted from more informal carers than women, with a higher proportion of the carers feeling overburdened.
Dependency for daily living activities is an understandable predictor of home care nursing workload, also identified by other authors27,28, while dependency for instrumental living activities also implies more home care nursing8. Our dependent patients also had the poorest health.
In our study, higher-educated and affluent populations did not receive more home care services, as has been described in other environments8–10. On the contrary, in Catalonia social factors do not make access to home care nursing more difficult: populations with higher social risk receive more services.
Emergency care visits are an indicator of patient complexity used to identify over-users of hospital services21. In our study, patients who used out-of-hours home care services also had an increased risk of more nursing home care visits. This group of patients also benefitted from more informal carers. Despite their higher level of dependency, the elevated use of home services by this group might be explained by the advocacy role of their informal caregivers, as may be the case with male patients. Certain population groups are known to over-use health care services, even though they need them less29,30.
Multivariate analysis showed that the increased nursing activity in patients with abnormal Pfeiffer scale scores found in the bivariate analysis was not due to cognitive impairment but to other factors, such as the presence of decubitus ulcers. One explanation for this finding may be that patients with cognitive impairment benefit more from social and family support than from nursing care. Other authors also found that cognitive impairment was not related to more nursing visits31, except in patients living alone32.
The results of this study suggest that nursing care in Catalonia is demand-led33. Activity is not only explained by variables related to health needs, such as decubitus ulcers or the degree of dependency, but is also associated with variables linked to demand, such as the availability of an informal caregiver in the case of male patients or in the group using out-of-hours services. In line with this argument, those that seek fewer healthcare services, such as smokers or patients with a high level of cognitive impairment, receive less nursing home care. For the same reason, people living alone do not appear to be high consumers of home care services10,32. The same situation is found in countries with preventive home care programs with special follow-up plans for this group of patients.
A set of patient characteristics described by other authors did not appear to be significant in our multivariate analysis, such as age1,9,10, hospital or nursing home admissions21, low levels of self-perceived health8, pain34, or the number of persons living in the same household7. Some of these characteristics, such as low levels of self-perceived health, were identified in the bivariate analysis, but became neutralized in the multivariate analysis because of their close relationship and the higher power of the characteristics finally found to be significant.
Our results show that decubitus ulcers were the patient characteristic that best predicted nursing workload in home care. Thus efforts should focus on prevention of these ulcers through interventions that include appropriate support surfaces such as special mattresses, repositioning at least every 4h, nutritional status, moisturizing and surveillance of at-risk skin sites. Most of these interventions can be achieved and improved in a home care environment if health education programs are offered to families. If home care services, which are currently entirely demand-oriented, are redirected to a more preventive approach, many decubitus ulcers might be avoided and consequently nursing workload would be reduced. Because ulcers require many nursing visits, reorientation toward prevention might benefit patients’ health and reduce hospital admissions35. The inclusion of special mattresses in the list of orthopedic devices covered by the National Health Service and the patient care education provided by nurses to families are measures that could be both cost-effective and beneficial for the health of the patients and their carers.
Author contributionsJ. Gené, A. Hidalgo and J.C. Contel designed the study. All the Research Team HC>65 collected the data, coordinated by A. Borràs. A. Borràs and M. Piñeiro analyzed the data. A. Borràs and J. Gené drafted the manuscript. All the authors contributed ideas, interpreted the findings and checked the first manuscript. All the authors approved the final version of the manuscript.
FundingThis research project was financed by a grant from the Catalan Agency for Health Technology Assessment and Research (CAHTA) in 2004. The project was also partially financed by a research grant from the Fundación MAPFRE.
Conflict of interestNone.
Research Team HC>65 (Appendix 1). The full list of participants has been published elsewhere: Gené J, et al. Los problemas de salud también explican la utilización de servicios sociales en atención domiciliaria. Aten Primaria. 2009;41:91-101.