To estimate the additional cost attributable to nosocomial infection (NI) in a pediatric intensive care unit (PICU) and related factors.
MethodsA prospective cohort study was conducted in all children admitted to the PICU of a tertiary-care pediatric hospital between 2008 and 2009. Descriptive and bivariate analyses were conducted of total direct costs due to PICU stay and medical procedures in patients with and without NI. A log-linear regression model was performed to determine the factors associated with higher total cost.
ResultsA total of 443 patients were studied and the prevalence of NI was 11.3%. The difference in the median total cost was €30,791.4 per patient between groups with and without NI. The median cost of PICU length of stay in patients with NI was almost eight times higher than the median cost of patients without NI. In patients with NI, the highest costs related to medical procedures were associated with antibiotics, enteral and parenteral feeding, and imaging tests. In the multivariate model, the factors associated with higher cost were infection, the performance of cardiovascular surgery, urgent admission, a higher pediatric risk mortality score, and the presence of immunosuppression. By contrast, older children and those with surgical admission generated lower cost.
ConclusionsNI was associated with an increase in total cost, which implies that the prevention of these infections through specific interventions could be cost-effective and would help to increase the safety of healthcare systems.
El objetivo del estudio es estimar el coste adicional atribuible a la infección nosocomial (IN) en una Unidad Pediátrica de Cuidados Intensivos (UCIP) y sus factores asociados.
Métodoestudio de cohortes prospectivo de todos los pacientes ingresados en una UCIP de tercer nivel entre 2008 y 2009. Se realizó un análisis descriptivo y bivariante del coste total asociados a estancia en UCIP y procedimientos en pacientes con y sin IN. Mediante regresión lineal múltiple, se estimaron los factores asociados al incremento del coste total.
Resultadosse estudiaron 443 pacientes, la incidencia de IN fue 11,3%. La diferencia de las medianas en el coste total fue de 30.791,4€ por paciente entre los grupos con y sin IN. El coste mediano de la estancia de pacientes con IN fue casi ocho veces mayor que el coste mediano de los pacientes sin IN. En pacientes con IN, el coste asociado a procedimientos más elevado fue el de antibióticos, nutrición enteral y parenteral y pruebas de imagen. En el modelo multivariante los factores asociados con un mayor coste fueron: presencia de infección nosocomial, cirugía cardiovascular, tipo ingreso urgente, mayor índice pronóstico de mortalidad al ingreso y la presencia de inmunosupresión. Por el contrario, los de mayor edad y aquellos ingresados por cirugía presentaron un menor coste.
ConclusionesLa IN está asociada al incremento del coste total, lo que implica que la prevención de estas infecciones mediante intervenciones específicas podría resultar costo-efectiva, redundando en sistemas de salud más seguros.
In Pediatric Intensive Care Units (PICU), the prevalence of nosocomial infection (NI) is variable, ranging from 10 to 33%1,2, and incidence rates from 5.9 to 15 per 1,000 patient-days3,4. This is explained by the greater complexity of these patients affected by a variety of medical and surgical pathologies1.
NI is also considered one of the most costly problems for hospitals. The most important direct NI-associated cost comes from the increase in the excess of length of stay (LOS)5. Therefore, most reports focus on NI-related costs due to LOS, as it is quite easy to translate such costs to currency value, applying the local cost per hospitalization day6. Further studies also have taken into account the costs of diagnostic and medical procedures, derived from or due to the infection, as the most accurate way to calculate the NI-attributable cost7–10.
The study of NI-associated cost has evolved in time with the introduction of new cost estimation methods11–13. The most common comparative method used to analyse the cost of NI, is the prospective or retrospective observational study of the hospital environment14.
Few studies have assessed the impact of NI on total costs in PICU15, some of them have analysed the cost attributable to any type of NI in PICU7,11,12,16, others have focused only on nosocomial primary bloodstream infection8,9. The average cost attributable to NI described in literature ranges between €1,51017-53,0859 per patient.
The Spanish Public Healthcare System is a tax-financed system that offers universal coverage, which is different from privately-funded healthcare systems, where most of the published reports on NI-related cost have been performed5,7. The lack of previous Spanish reports about NI costs in PICU and the actual economical crisis in this country, justifies the present paper. The aim of the study is to estimate the cost attributable to nosocomial infection in a pediatric intensive care unit and its related factors.
MATERIAL AND METHODSStudy DesignProspective cohort study between September 2008 and July 2009. The study was carried out in a 16-bed multidisciplinary PICU of a tertiary-care university hospital of the Andalusian Public Health System. This Unit is a regional referent institution for highly complex procedures, and offers assistance to patients older than 28 days of age and also to neonates during the cardiovascular surgery postoperative period. All patients admitted in the PICU for less than 24hours were excluded (a total of 426 patients were excluded). Nine patients remained hospitalized at the end of the study.
VariablesThe dependent variable was total cost (only took into account the costs incurred in the PICU), which included the sum of the following cost items: PICU LOS, invasive mechanical ventilation, imaging and microbiological tests, enteral and total parenteral nutrition, antibiotherapy, consumables (central line, urinary catheter) and structure costs.
The following independent variables were collected: a) Sociodemographic and admission variables: Age, sex, type and cause of PICU admission and cause of discharge; b) Clinical variables: Presence of NI, classified according the definitions of the Centers of Disease Control and Prevention18; c) Risk factors for NI1: factors related to patient's intrinsic characteristics and factors related to surgery and other procedures made during PICU stay.
Sources of informationThe consumption of different resources (LOS, special feeding formulas and parenteral nutrition, days of mechanical ventilation, imaging and microbiological tests, antibiotherapy and consumables) was obtained from medical records and direct observation, all of which were validated with PICU pediatrician.
The cost of imaging procedures was obtained from the Andalusian Official Bulletin Board19. Cost of consumables, those related to PICU stay, nutrition, mechanical ventilation and antibiotherapy were obtained from the hospital accounting system. Costs of microbiological tests were obtained from an external reference laboratory20. All costs were updated to the present-day currency in Spain, the Euro (2009).
Costs estimation1) The estimation of PICU LOS (it includes the costs of PICU staff, consumable goods, catering, instruments and tools, inversions, cleaning, office material, conservation and repair, professional services and supplies for the PICU) was calculated according to the method suggested by Brazzi et al.21 2) The average cost per day of enteral feeding and total parenteral nutrition was calculated and attributed to each patient. 3) The average cost of invasive mechanical ventilation was calculated per patient according to the cost of acquisition, usage and lifespan. 4) For the estimation of the structure costs we used the method suggested by Mason et al.22, which means add 25% to the direct cost. All of them were validated with PICU pediatrician.
Data were collected from the clinical records by trained personnel in epidemiological surveillance and tabulated in a spreadsheet which was specifically designed for this study. The data collection model applied included consumable goods used per patient. These data were classified according to whether they were attributable or not to NI, depending on the most prevalent NI types. The criteria considered to attribute procedures to NI are shown in Table 1. Finally, the project was approved by the hospital Ethics Committee.
Criteria used to attribute medical procedures-related costs to nosocomial infection (NI).
| Type of medical procedure | Description |
|---|---|
| Use of central venous catheter | Catheter replacement due to suspected bloodstream infection will be attributed to NI, whenever the criteria set by the Centers for Disease Control and Prevention (CDC) are met. |
| Invasive Mechanical Ventilation | The onset and/or extension of invasive mechanical ventilation in case of clinical worsening of a patient with lower respiratory tract infection or as a result of worsening of other NI considered within the context of cost analysis. |
| Urinary catheter | The cost of the urinary catheter or its replacement will be attributed to NI whenever urinary tract infection acquired during the urinary catheterization period is confirmed. |
| Microbiological, Imaging and antibiotherapy tests | Any microbiological cultures, Imaging tests and antibiotic therapy required for the diagnosis and treatment of NI and which are not included in the medical protocol required by the cause of admission will be attributed to NI. |
NI definition, and infection rates (with 95% confidence intervals) proposed by the National Nosocomial Infections Surveillance System were estimated23. The chi-squared test was used to compare proportions (NI presence or absence).
NI costs were calculated from the hospital perspective. As a result, we only considered direct tangible costs of PICU for global NI (includes bloodstream infection, pneumonia, urinary tract infection and surgical site infection). In order to calculate average cost, the procedures required per patient, which were attributable to NI, were considered. To check whether these procedures were justified or not, patients’ clinical record and interviewed with pediatrician were reviewed.
First of all, a descriptive analysis was performed through mean, median, standard deviation and range. Subsequently, univariate analysis established differences between total cost and independent variables (Mann-Whitney U and Kruskal-Wallis tests for independent categorical variables, and linear regression analysis for independent continuous variables).
A multivariate linear regression was performed to determine the NI cost adjusted by different variables. The variable cost was log transformed, because it was not normally distributed. Clinically relevant variables, those which a priori would be expected to predict costs and those that were shown to be associated at a statistically significant level, were selected for inclusion in the model. The non-collinearity, homogeneity of variance of the variables and the homoscedasticity of the model as well as data fitting using Cook's Distance, the relationship between outliers and standard points and the normal distribution of outliers, were checked. The analysis was carried out using the statistical software package SPSS.v19.
ResultsThe number of patients enrolled in the study was 443 (57% were boys), with a median age of 1.5 years (percentile 25: 5.3 months- percentile 75: 6.2 years). The cause of admission was surgery in 58.5% of patients, being cardiovascular surgery the most common intervention (46.33%). Global mortality in the Unit was 6.3%. The most frequent procedures were: use of antibiotics, central venous catheterization and invasive mechanical ventilation (85%, 64% and 55%, respectively). Fifty patients suffered, at least, one episode of NI, which means a prevalence of patients with NI of 11.3%. The total number of NIs was 82 in 443 patients (14.71%). Table 2 shows the number of infections according to site and infection rates which ranged between 7.9% (bloodstream infections incidence) to 1.4% (other infections). 60.6% of the infected patients had a single episode of infection, 18.2% had two infections, and 16.7% had three infections. Two patients had up to 4 infections during admission to the Unit.
Incidence of nosocomial infection sites.
| Nosocomial Infection Site | Number of episodes | Frequency* (%) | Incidence Rate†(%) | Incidence Density Rate‡ |
|---|---|---|---|---|
| Bloodstream infection | 35 | 42.7 | 7.9 | 14.43 |
| Pneumonia | 23 | 28.0 | 5.2 | 15.76 |
| Surgical site infection | 11 | 13.4 | 2.5 | 4.25 |
| Urinary tract infection | 7 | 8.5 | 1.6 | - |
| Other infection | 6 | 7.3 | 1.4 | - |
* No. Nosocomial infections (NI)/total number of infections*100 †No. NI/total number of patients*100; ‡No. bloodstream infections per 1,000 days central line catheter; No. pneumonias per 1,000 days with mechanical ventilation; No. surgical site infection/total of surgical interventions *100.
Non significant differences were found between patients who had NI and those who didn’t according to gender, patient origin, presence of malformation and reason for admission. On the contrary, those with a younger age had a higher risk of NI in comparison to those who were older (Table 3).
Bivariant Analysis between nosocomial infection and sociodemographic and admission variables.
| Without Nosocomial Infection N (%) | With Nosocomial Infection N (%) | |
|---|---|---|
| Sexb | ||
| Boy | 228 (90.5%) | 24 (9.5%) |
| Girl | 165 (86.4%) | 26 (13.6%) |
| Procedenceb | ||
| Other hospital | 44 (88%) | 6 (12%) |
| Home | 48 (92.3%) | 4 (7.7%) |
| Operating room | 119 (93.7%) | 8 (6.3%) |
| Other service | 182 (85%) | 32 (15%) |
| Presence of malformationb | ||
| No | 195 (90.3%) | 21 (9.7%) |
| Yes | 198 (87.2%) | 29 (12.8%) |
| Cause of PICU admissionb | ||
| Medical | 159 (88.3%) | 21 (11.7%) |
| Surgical | 208 (88.1%) | 28 (11.9%) |
| Trauma | 12 (100%) | 0 (0%) |
| Transplant | 10 (90.9%) | 1 (9.1%) |
| Others | 4 (100%) | 0 (0%) |
| Age groupsa | ||
| 0-2 months | 44 (74,6%) | 15 (25.4%) |
| 3 months - 1 years | 109 (85.8%) | 18 (14.2%) |
| 2-5 years | 126 (95.5%) | 6 (4.5%) |
| 6-12 years | 74 (90.2%) | 8 (9.8%) |
| Over 12 years | 40 (93%) | 3 (7%) |
Table 4 shows the relationship between the total cost and independent variables for the patients admitted in the PICU. It highlights the higher median cost in children with less than 2 months of age (€6,903.30) and the difference in median cost between bloodstream infection and pneumonia (€37,356.68 and €34,912.96, respectively). Furthermore, the cost increase was proportional to the number of NI diagnosed, with a difference in median cost between having a single infection and 3 or 4 infections of €38,202.57.
Cost analysis of variables related to admission, patient's intrinsic characteristics, and variables related or due to procedures during pediatric intensive care unit (PICU) stay.
| Total Cost €Average (Median) | p | |
|---|---|---|
| Age groups | ||
| 0-2 months | 12,391.54 (6,903.30) | |
| 3 months - 1 years | 10,028.14 (4,047.99) | |
| 2-5 years | 6,626.95 (3,047.07) | |
| 6-12 years | 5,936.10 (3,064.88) | |
| Over 12 years | 6,112.18 (3,092.41) | <0.001b |
| Cause of PICU admission | ||
| Medical | 10,831.99 (4,234.83) | |
| Surgical | 6,466.42 (3,079.48) | |
| Trauma | 2,566.42 (2,087.45) | |
| Transplant | 8,646.17 (6,548.23) | |
| Others | 6,819.02 (4,862.94) | <0.001b |
| Type of admission | ||
| Elective | 6,175.98 (3,061.63) | |
| Emergency | 10,291.44 (4,215.44) | <0.001a |
| PRISM index | ||
| 0-10 | 5,823.08 (3,137.58) | |
| >10 | 14,416.39 (8,040.86) | <0.001a |
| Immunosuppression | ||
| No | 7,782.94 (3,179.44) | |
| Yes | 12,096.62 (6,174.37) | <0.001a |
| Previous respiratory disease | ||
| No | 7,018.44 (3,378.61) | |
| Yes | 27,812.31 (4,176.73) | 0.026a |
| Infection at admission in PICU | ||
| No | 6,866.32 (3,127.06) | |
| Yes | 11,759.96 (4,501.40) | <0.001a |
| Cause of discharge | ||
| Healing | 6,946.21 (3,203.70) | |
| Exitus | 21,681.17 (6,626.98) | |
| Unknownc | 22,420.13 (11,438.87) | <0.001b |
| Surgery during admission | ||
| No | 8,091.67 (4,048.02) | |
| Yes | 8,245.86 (3,183.97) | 0.106a |
| Cardiovascular surgery | ||
| No | 7,122.94 (3,059.62) | |
| Yes | 11,069.21 (5,157.50) | <0.001a |
| Mechanical ventilation | ||
| No | 3,559.82 (2,291.40) | |
| Yes | 11,969.72 (5,100.19) | <0.001a |
| Total parenteral feeding | ||
| No | 3,214.45 (3,430.33) | |
| Yes | 13,714.52 (9,089.37) | 0.03a |
| Immunosuppressive therapy | ||
| No | 5,908.44 (2,724.87) | |
| Yes | 10,506.52 (4,468.25) | <0.001a |
| Use of antibiotherapy | ||
| No | 3,571.58 (2,485.69) | |
| Yes | 9,000.77 (4,004.44) | 0.012a |
| No. of nosocomial infections | ||
| None | 4,657.19 (3,084.24) | |
| One | 19,041.84 (15,085.93) | |
| Two | 42,683.96 (35,019.31) | |
| Three-four | 63,213.73 (53,288.50) | <0.001b |
| Bloodstream infection | ||
| No | 5,830.76 (3,162.45) | |
| Yes | 43,187.44 (28,012.01) | <0.001a |
| Pneumonia | ||
| No | 6,458.08 (3,218.90) | |
| Yes | 41,371.04 (31,827.37) | <0.001a |
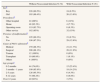
Table 5 shows the differences between infection and non-infection regarding cost. It is worth noting that about 70% of the total cost was due to LOS expenses. In this sense, median LOS of patients with NI was 24 days versus 3 days for those without NI (p<0.001). The difference in the median cost of LOS in NI-patients, was statistically different comparing it to those without NI (€18,695.35 and €2,386.64, respectively). Regarding the total cost of the patients with NI included, a difference in median cost of €20,947.94 (€30,791.41 average cost) was observed between patients with and without NI (p<0.001).
Cost in Euros (€) of children admitted in the Pediatric Intensive Unit (PICU) per patient with and without nosocomial infection.
| Without InfectionAverage (median) | With InfectionAverage (median) | |
|---|---|---|
| PICU-stay costa | 3601.21 (2386.64) | 27875.97 (18695.35) |
| Mechanical ventilation cost a | 4.27 (0) | 41.25 (34.09) |
| Imaging test costb | 63.67 (27.69) | 143.98 (101.53) |
| Feeding costa,b | 15.34 (5.80) | 20.85 (116.18) |
| Antibiotherapy costa | 20.85 (0.93) | 140.68 (33.40) |
| Microbiological test cost a | 83.25 (49.58) | 240.49 (135.54) |
| Central venous catheter related cost | 29.40 (39.16) | 70.50 (58.75) |
| Arterial catheter related cost | 2.70 (0) | 5.55 (8.41) |
| Direct costa | 3773.26 (2479.76) | 28406.39 (19238.12) |
| Total cost a,§ | 4716.58 (3099.70) | 35507.99 (24047.64) |
PICU: Pediatric Intensive Care Unit
p<0.005; ‡Parenteral feeding or specific infant formulas provided by the Pharmacy Service; §Total cost= direct cost plus 25%21
The multivariate analysis shows that those with bloodstream infections (p<0.001) and pneumonia (p= 0.008) have a greater cost than those without NI. It is worth noting that a higher cost in PICU was associated with cardiovascular surgery (p<0.001), urgent type of admission (p= 0.004), higher Pediatric Risk of Mortality index (p<0.001) and the presence of inmunosuppression (p<0.001). By contrast, older children and surgical type of admission (p= 0.009) presented a lower cost (Table 6).
Multivariate model of factors associated with the increase in total costs at the pediatric intensive care unit (n=443; R2 48%).
| p | β (95% CI) | ||
|---|---|---|---|
| Constant | <0.001 | 3.554 (3.397; 3.710) | |
| Age groups | 0-2 months | ||
| 2 months - 1 year | 0.003 | -0.172 (-0.287; -0.057) | |
| 1-5 years | 0.003 | -0.181 (-0.298; -0.063) | |
| 5-12 years | 0.001 | -0.217 (-0.343; -0.091) | |
| Over 12 years | 0.376 | -0.067 (-0.215; 0.081) | |
| Bloodstream infection | No | ||
| Yes | <0.001 | 0.648 (0.499; 0.797) | |
| Pneumonia | No | ||
| Yes | 0.008 | 0.254 (0.067; 0.442) | |
| Cardiovascular surgery | No | ||
| Yes | <0.001 | 0.287 (0.196; 0.378) | |
| Type of admission | Medical | ||
| Surgical | 0.009 | -0.149 (-0.260; -0.038) | |
| Immunosuppression | No | ||
| Yes | 0.001 | 0.199 (0.085; 0.312) | |
| Type of admission | Elective | ||
| Urgent | 0.004 | 0.157 (0.050; 0.264) | |
| PRISM index | <0.001 | 0.014 (0.007; 0.021) |
PRISM: Pediatric Risk of Mortality
The analysis of NI-related costs started in countries with privately-funded health care systems, followed by others with a hybrid system of private and public insurance, like Spain10,24–26. In these studies, the type of patients included and the healthcare systems where they were performed were very different, which hinders any possible comparison. However, all of them report a remarkable cost associated to NI7.
In the present study, estimated costs have been based upon prolonged PICU LOS and variable costs of different medical procedures, the latter being a direct attribution resulting from the NI presence, which is a better estimation of attributable costs. In this sense, Pittoni and Scatto27 remark the importance of taking into account direct variable costs to understand the real costs generated from a patient admitted in the intensive care unit, including non complex medical procedures as they may affect the result of cost analysis in an accumulative way.
The authors have performed a multivariate analysis using multiple linear regression models in order to assess factors associated with the total cost, as it is difficult to choose the matching factors between cases and controls without committing a selection bias. This follows the current trend in NI-related cost analysis (from 1990 to 1999, 14.3% of the studies performed multiple linear regression and from 2000-2006, 34.5% did so28).
In this study, we observed a difference of 21 days in PICU LOS between patients with and without NI. Although, the authors did not adjust by other variables, there was a difference in costs between both groups of more than €30,000. In spite of being statistically significant, it may not be exclusively due to NI. This analysis, although it has been the most frequently used in studies of costs for NI, has limitations, as it results from an average measure. Also, it does not reflect the real expenditure, considering that this is not uniform throughout the stay, and that, as the NI is time-dependent, it should measure the extension of the stay only after its diagnosis, and not for the entire stay12. Nevertheless, other studies carried out in PICU, despite of using a different methodology, and adjusted due to other factors like patients’ age or cause of PICU admission, show similar results, like, Slonim et al.8, who found a difference of 14 days, or Elward et al.9, with a mean hospital LOS cost of €24,619 in patients with NI.
It also must be taken into account the association between LOS and NI, which may be contradictory, since, although it is recognized by the literature that NI increases hospital stay29, some authors also consider LOS as a risk factor for the NI30 (longer hospitalizations leading to colonization of patients by pathogenic microorganisms, longer duration of invasive procedures and pharmacotherapy which favours the development of NI). However, the cost study presented here was part of a prospective study which also analyzed the risk factors associated with NI, not finding a significant association between LOS and NI. Therefore, in this paper, the authors have assumed that NI has influenced the increase in LOS, considering what referred by the literature and the results of the study for risk factors of NI.
Average cost of medical procedures in the current study was higher in the case of NI patients when compared with non-infected patients, where the use of antibiotherapy, feeding and imaging tests should be highlighted. In the case of bloodstream infection, the cost of catheters and antibiotics doubled the observed in patients with pneumonia, as in Pittoni and Scatto's case27, which remarks that one of the most difficult challenges is the bloodstream infection management, because of its wide array of possible treatments and elevated associated cost.
Globally, the cost of NI is within the range described in other studies performed in PICU5,7,9,11,17,31 (from €1,51017 to €53,0859). The last study showed higher costs, which may, in part, be justified by the use of a cost-estimation method based upon cost to charge ratios and the inclusion of more complex patients. The BI was the most costly NI, showing significant difference when compared to pneumonia, which it agrees with other studies5,32.
Nevertheless, the results from other studies which only report average values must be interpreted cautiously. Their costs estimations were obtained in different countries with a healthcare management which may not be equivalent to the Spanish Health System. Likewise, other costs should be considered, such as those derived from patients who die as a result of the NI; the cost of the medical procedures required by the treatment of NI beyond 48hours after discharge from PICU, or the indirect or intangible costs referred to productivity loss, and more specifically what the patient loses as a result of the infection and/or treatment (pain, suffering, loss of leisure time), which affects their quality of life.
Some of the variables that were associated with an increase of total cost (presence of NI, emergency admission, previous cardiovascular surgery and immunosuppression), were also been reported by other studies9,16,29. Other factors that may also increase the cost of the Unit were the cause of non surgical admission and comorbidities such as severe lesions in primary organs7,9,12,33. In the present study, only immunosuppression, as a patient's intrinsic factor, contributed in a statistically significant way to the model. In this sense, Gemke et al.34 stated that non previously programmed admissions did increase the use of resources and, consequently, total costs.
Another factor included in our model as a risk factor is cardiovascular surgery, which could be due to the high number of patients undergoing such surgery in the PICU, postoperative LOS, frequent infectious complications and prolonged use of medical procedures, which means an increase of total economic costs. The inclusion of this factor is supported by a recent report published by González et al.35, which states that prolonged admissions convey a greater use of medical resources, higher risk of NI and higher mortality rates among children admitted to PICU35. Other studies mention hospital stay1,14 and non survival in the Unit7,9,24 as factors capable of rising costs. These variables were only statistically significant in the bivariate analysis.
In conclusion, this paper has approached to NI-related economic cost, where most of the expenses are derived from the medical procedures made to the patient during PICU stay and its complications. The higher total cost per patient requires the implementation of specific cost-effective preventive measures to control NI, in order to minimize its effects in the health of pediatric patients and in medical costs.
Nosocomial infection in Pediatric Intensive Care Units has a significant impact on morbidity, mortality and economic cost. However, very few studies have performed an estimate of the economic cost of nosocomial infection in public health systems, since most of them are confined to privately funded healthcare systems and adult population.
What does this study adds?The present study provides an estimate of the economic cost of nosocomial infection in critically ill children, which may be useful to both economic managers and physicians about its repercussion in economic terms.
Miguel Ángel Negrín
Author's ContributionThe project's original idea was provided by R. López. A. Morillo and JM Aldana adapted the idea for the research project and its implementation in a Pediatric Intensive Care Unit. R. Valencia developed the project's methods, and performed the database and its depuration. The clinical data collection and the attribution of medical procedure-related costs to nosocomial infection were made by A. Morillo and R. López. A. Olry performed the economic analysis. M. Conde and M. Loscertales requested the costs information from the Departments of Pharmacology and Economic Management. A. Morillo wrote the first draft of the article, and was subsequently reviewed and approved by all authors.
FundingThis project has been funded by the Andalusian Regional Ministry of Health.
Conflicts of interestNone
To all the staff of the Pediatric Intensive Care Unit and the Department of Economic Management from Virgen del Rocío University Hospital, for their cooperation in this project.