To explore general practitioner (GP) training, continuing professional development, scope of practice, ethical issues and challenges in the working environment in three European countries.
MethodQualitative study of 35 GPs from England, Germany and Spain working in urban primary care practices. Participants were recruited using convenience and snowball sampling techniques. Semi-structured interviews were recorded, transcribed and analysed by four independent researchers adopting a thematic approach.
ResultsEntrance to and length of GP training differ between the three countries, while continuing professional development is required in all three, although with different characteristics. Key variations in the scope of practice include whether there is a gatekeeping role, whether GPs work in multidisciplinary teams or singlehandedly, the existence of appraisal processes, and the balance between administrative and clinical tasks. However, similar challenges, including the need to adapt to an ageing population, end-of-life care, ethical dilemmas, the impact of austerity measures, limited time for patients and gaps in coordination between primary and secondary care are experienced by GPs in all three countries.
ConclusionPrimary health care variations have strong historical roots, derived from the different national experiences and the range of clinical services delivered by GPs. There is a need for an accessible source of information for GPs themselves and those responsible for safety and quality standards of the healthcare workforce. This paper maps out the current situation before Brexit is being implemented in the UK which could see many of the current EU arrangements and legislation to assure professional mobility between the UK and the rest of Europe dismantled.
Analizar la formación, el desarrollo profesional continuado, el ámbito de práctica, las cuestiones éticas y los retos en el entorno laboral de los médicos de atención primaria en tres países europeos.
MétodoEstudio cualitativo de 35 médicos de atención primaria de Inglaterra, Alemania y España que trabajan en centros urbanos de atención primaria. Se reclutó a los participantes utilizando técnicas de muestreo de oportunidad y con efecto multiplicador. Se registraron, transcribieron y analizaron entrevistas semiestructuradas realizadas por cuatro investigadores independientes, quienes adoptaron un enfoque temático.
ResultadosEl acceso y la duración de la formación del médico de atención primaria difieren entre los tres países, mientras que se requiere desarrollo profesional continuado en los tres, aunque con características diferentes. Las variaciones clave en el ámbito de la práctica incluyen la existencia de un papel curativo, si el trabajo de médico de atención primaria se realiza en equipos multidisciplinarios o de manera individual, la existencia de procesos de valoración, y el equilibrio entre las tareas administrativas y clínicas. Sin embargo, los médicos de atención primaria en los tres países se enfrentan a retos similares, que incluyen la necesidad de adaptarse al envejecimiento de la población, la atención al final de la vida, el impacto de las medidas de austeridad, la limitación del tiempo de dedicación al paciente, y las brechas en cuanto a coordinación entre la atención primaria y secundaria.
ConclusiónLas variaciones de la atención primaria tienen fuertes raíces históricas, que se derivan de las diferentes experiencias nacionales y el rango de los servicios clínicos proporcionados por los médicos de atención primaria. Existe una necesidad de fuentes de información accesibles para dichos médicos, y aquellos responsables de los estándares de seguridad y calidad del personal sanitario. Este trabajo esboza la situación actual que está siendo implementada en el Reino Unido con anterioridad al Brexit, que podría vislumbrar muchos de los acuerdos y legislaciones actuales de la UE para garantizar la movilidad profesional entre el Reino Unido y el resto de la Europa desmantelada.
The increasing number of doctors relocating for work within the EU1,2 benefit from the newly revised EU Directive 2005/36/EC which stipulates the mutual recognition of professional qualifications.3 The United Kingdom (UK) is a popular destination for doctors from other EU Member States from a broad spectrum of specialties;4 in 2015, more than 10% (29,376) of doctors on the General Medical Council register had qualified in another Member State, of whom nearly 4,055 are general practitioners (GPs) (6.2% of all UK GPs).5,6 This growth in mobility has given rise to concerns about standards of postgraduate training and continuous professional development (CPD). The EU Directive 2005/36/EC considers general practice a distinct post-graduate medical qualification, although separate from other postgraduate medical specialties, however it does not regulate quality and content of training or transferability of skills, merely specifying the minimum time required to gain the post-graduate medical qualification to become a general practitioner (currently a minimum of least three years on a full-time basis).7
Once the right to practice is conferred by licensing and/or registration, the requirements for maintaining this status vary extensively among countries.8 The EU initiative does not take into account the presence of compulsory re-licensing in certain EU countries (e.g. the UK) which requires health professionals to undergo revalidation at regular intervals and participate in continuing professional development, including annual appraisals.9 There are concerns that this lack of formalised, regular assessment of a GPs’ suitability to practise may jeopardise quality of care.10,11 In addition there have been concerns that inability to assess language abilities or access to fitness to practice records from the practitioner's home country's regulator also pose a potential risk to patient safety. Recent changes to the directive have addressed some of these issues; language testing by regulators (and not just employers) has been permitted since June 2014,12 and a European professional card designed to give regulators access to more information about doctors from across Europe has been introduced.12
Primary care in Europe is undergoing continuous changes in response to the growth of multi-morbidity, whilst battling funding constraints following the economic crisis. There are serious concerns about low recruitment and staff retention in the UK, which will likely increase demand for GPs from the rest of the EU.13,14 However, there is little recent comparative literature on GP training and scope of practice among European countries. What exists examines the organization of specialty training among various EU countries,15 assessment of trainees’ and trainers’ knowledge,16 educational expectations of GP trainers,17 funding of vocational programmes for general practice,18 service profiles of GPs,19 length of consultation,20 general cross-country experiences,21,22 communication in general practice23,24 and ethical issues25,26. All these studies reveal numerous differences. While most of these studies focus on just one of the characteristics of general practice, this paper aims to provide a broader perspective, examining several aspects including postgraduate GP training, scope of practice, challenges and experiences of GPs in three countries: England, Germany and Spain.
For the purpose of this paper when we refer to general practice we take the definition of general practice/family medicine as set out by the European association of the World Organisation of Family Doctors (WONCA).27
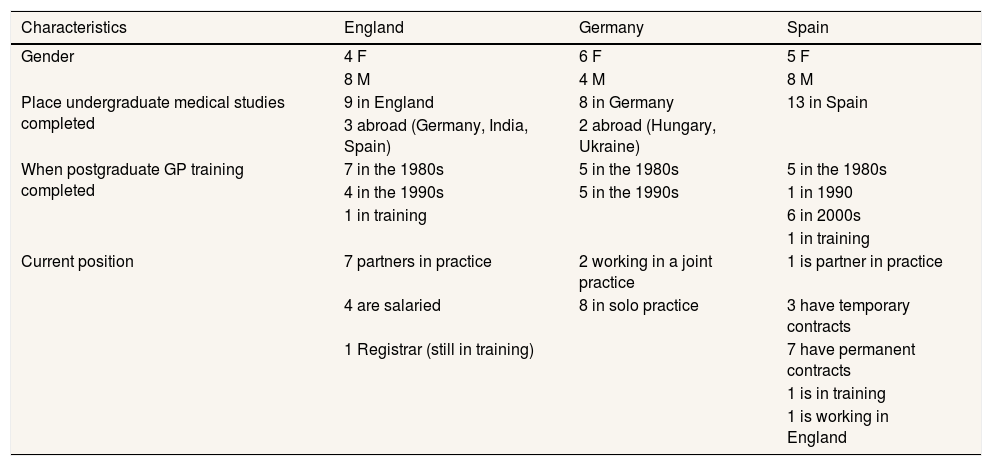
MethodsSemi-structured interviews were conducted between 2013 and 2014 with 35 general practitioners practising in London for England (n=12), Berlin for Germany (n=10), and in Barcelona and Madrid for Spain (n=13) (Table 1). Interviewees were eligible if they had undertaken or were currently in post-graduate GP training in their respective countries. Participants were recruited using convenience and snowball sampling techniques. A common topic guide covering themes related to medical training and scope of practice was developed in collaboration with medical experts. All interviewees gave consent for the interviews to be audio-recorded. Interviews lasted between 45 and 90minutes and were conducted in English, German, Catalan or Spanish, were digitally recorded and then fully transcribed in the respective language. Transcripts were coded independently and analysed in NVivo10 and ATLAS.ti 6.2 software packages using a common coding frame that had been developed both deductively –based on the topic guide– and inductively, following analysis of the transcripts. Data were analysed initially within each country by four independent researchers. In a second step the completed coding frames, written summaries and key quotes (translated into English) were reviewed by two authors who then completed the comparative analysis. We selected themes on the basis of their frequency in the interview data and their ability to identify similarities and differences between countries. Interpretation of the data is also informed by the researchers’ knowledge of the differences between the health systems, as interviewees may not have raised organisational aspects that they take for granted. Interview data was complemented with the review of secondary sources and questionnaires administered in each country8,28,29 to provide an accurate account of GP training and continuing professional development in the three selected countries.
Characteristics of interviewees.
| Characteristics | England | Germany | Spain |
|---|---|---|---|
| Gender | 4 F | 6 F | 5 F |
| 8 M | 4 M | 8 M | |
| Place undergraduate medical studies completed | 9 in England | 8 in Germany | 13 in Spain |
| 3 abroad (Germany, India, Spain) | 2 abroad (Hungary, Ukraine) | ||
| When postgraduate GP training completed | 7 in the 1980s | 5 in the 1980s | 5 in the 1980s |
| 4 in the 1990s | 5 in the 1990s | 1 in 1990 | |
| 1 in training | 6 in 2000s | ||
| 1 in training | |||
| Current position | 7 partners in practice | 2 working in a joint practice | 1 is partner in practice |
| 4 are salaried | 8 in solo practice | 3 have temporary contracts | |
| 1 Registrar (still in training) | 7 have permanent contracts | ||
| 1 is in training | |||
| 1 is working in England |
Ethical approval was provided by London School of Hygiene and Tropical Medicine Ethical Committee.
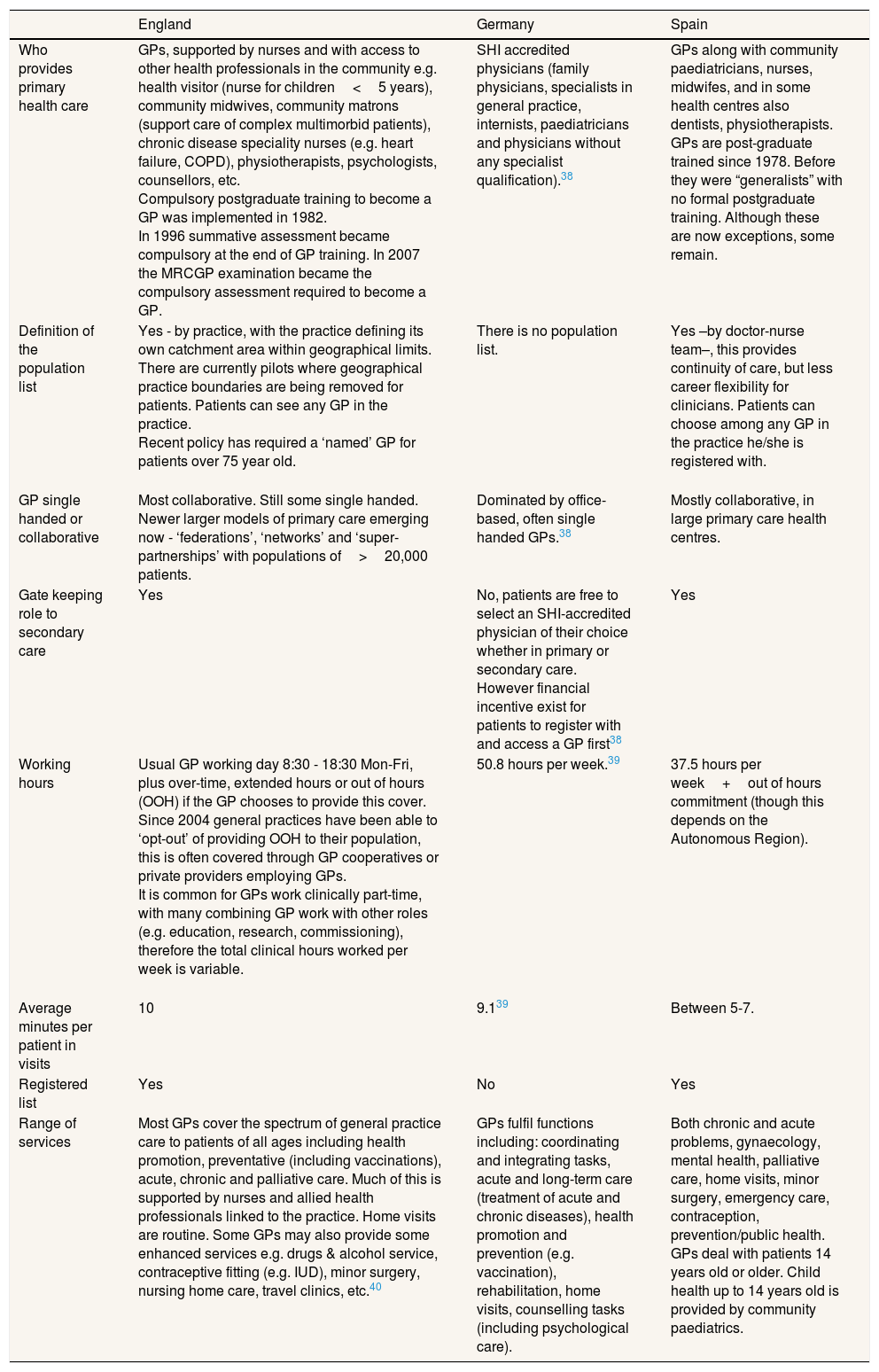
ResultsThe themes emerging from the interviews were: admission and duration of GP training; continuing professional development; scope of practice (practice organization and multidisciplinary teams; and administrative vs. clinical duties); ethical dilemmas and challenges; and areas for improvement. As noted above, there are some factors that, although not raised by interviewees, need to be considered in interpreting the findings. Thus, Spanish and German GPs do not routinely see children or deal with many of the gynaecological and ante- and post-natal aspects of care undertaken by GPs in the UK. GPs have a gate keeping role in England and Spain but not in Germany (Table 2 provides more background information on each system).
General practitioners characteristics for England, Germany, and Spain.
| England | Germany | Spain | |
|---|---|---|---|
| Who provides primary health care | GPs, supported by nurses and with access to other health professionals in the community e.g. health visitor (nurse for children<5 years), community midwives, community matrons (support care of complex multimorbid patients), chronic disease speciality nurses (e.g. heart failure, COPD), physiotherapists, psychologists, counsellors, etc. Compulsory postgraduate training to become a GP was implemented in 1982. In 1996 summative assessment became compulsory at the end of GP training. In 2007 the MRCGP examination became the compulsory assessment required to become a GP. | SHI accredited physicians (family physicians, specialists in general practice, internists, paediatricians and physicians without any specialist qualification).38 | GPs along with community paediatricians, nurses, midwifes, and in some health centres also dentists, physiotherapists. GPs are post-graduate trained since 1978. Before they were “generalists” with no formal postgraduate training. Although these are now exceptions, some remain. |
| Definition of the population list | Yes - by practice, with the practice defining its own catchment area within geographical limits. There are currently pilots where geographical practice boundaries are being removed for patients. Patients can see any GP in the practice. Recent policy has required a ‘named’ GP for patients over 75 year old. | There is no population list. | Yes –by doctor-nurse team–, this provides continuity of care, but less career flexibility for clinicians. Patients can choose among any GP in the practice he/she is registered with. |
| GP single handed or collaborative | Most collaborative. Still some single handed. Newer larger models of primary care emerging now - ‘federations’, ‘networks’ and ‘super-partnerships’ with populations of>20,000 patients. | Dominated by office-based, often single handed GPs.38 | Mostly collaborative, in large primary care health centres. |
| Gate keeping role to secondary care | Yes | No, patients are free to select an SHI-accredited physician of their choice whether in primary or secondary care. However financial incentive exist for patients to register with and access a GP first38 | Yes |
| Working hours | Usual GP working day 8:30 - 18:30 Mon-Fri, plus over-time, extended hours or out of hours (OOH) if the GP chooses to provide this cover. Since 2004 general practices have been able to ‘opt-out’ of providing OOH to their population, this is often covered through GP cooperatives or private providers employing GPs. It is common for GPs work clinically part-time, with many combining GP work with other roles (e.g. education, research, commissioning), therefore the total clinical hours worked per week is variable. | 50.8 hours per week.39 | 37.5 hours per week+out of hours commitment (though this depends on the Autonomous Region). |
| Average minutes per patient in visits | 10 | 9.139 | Between 5-7. |
| Registered list | Yes | No | Yes |
| Range of services | Most GPs cover the spectrum of general practice care to patients of all ages including health promotion, preventative (including vaccinations), acute, chronic and palliative care. Much of this is supported by nurses and allied health professionals linked to the practice. Home visits are routine. Some GPs may also provide some enhanced services e.g. drugs & alcohol service, contraceptive fitting (e.g. IUD), minor surgery, nursing home care, travel clinics, etc.40 | GPs fulfil functions including: coordinating and integrating tasks, acute and long-term care (treatment of acute and chronic diseases), health promotion and prevention (e.g. vaccination), rehabilitation, home visits, counselling tasks (including psychological care). | Both chronic and acute problems, gynaecology, mental health, palliative care, home visits, minor surgery, emergency care, contraception, prevention/public health. GPs deal with patients 14 years old or older. Child health up to 14 years old is provided by community paediatrics. |
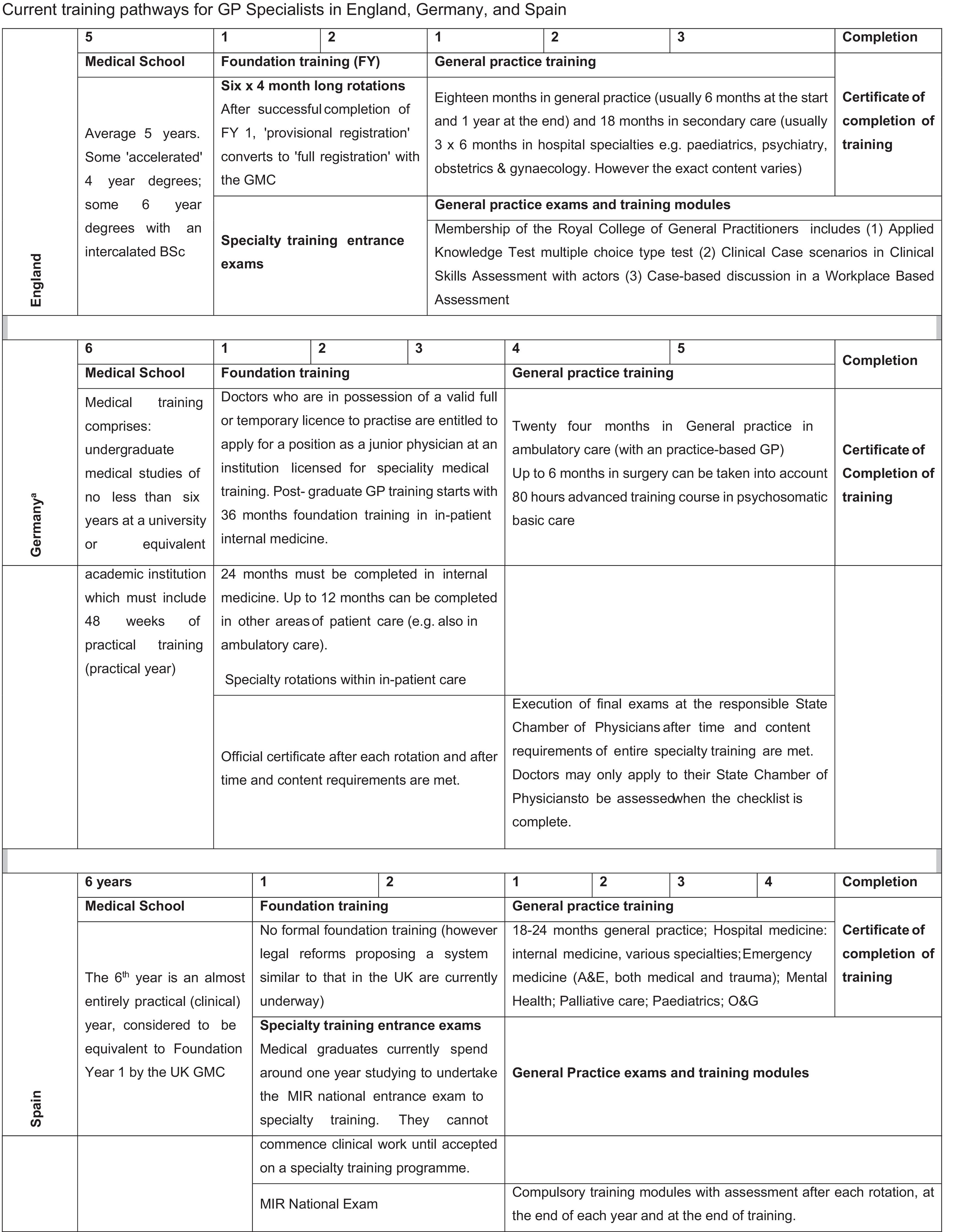
Each country has its own requirements for entry into GP training with the duration of post-graduate training lasting between three and five years (Fig. 1). In Germany, doctors who have completed their basic medical training and are in possession of a valid full or temporary licence to practise are entitled to apply for a position as a junior physician. Doctors who wish to become a GP apply at an institution licensed for medical training in this area of specialisation. Their GP training in a paid junior position usually starts after successful job interview with a position in inpatient care in internal medicine over a period of 36 months, followed by 24 months in general practice at an ambulatory unit under the supervision of a practise-based GP. During their five years of training, junior physicians must fulfil the requirements stipulated in the GP speciality training regulations and guidelines on the content of speciality training. Overall, post-graduate GP training takes five years to complete in Germany.
Current training pathways for GP Specialists in England, Germany, and Spain.
aThere is no standardized specialty training at federal level in Germany. The Regional Medical Chambers (‘as corporations under public law’) are responsible for the specialization and advanced training of doctors. Regulations on the content and configuration of speciality training are laid out in state by-laws and the autonomous statutes of the State Chambers of Physicians. The template of the Federal Chamber of Physicians with the guidelines for the specialty training only has a recommendatory character, thus specialty training guidelines can differ in detail among the federal ‘Länder’ (Bundesärztekammer, 2014).
In Spain entry to all postgraduate medical training is based on results in a national multiple-choice examination of clinical knowledge (known as MIR exam), combined with undergraduate qualifications. There is no formal foundation training prior to general practice training, although the sixth undergraduate year in Spain is considered equivalent to the UK's foundation year 1, as it is largely practical. This is likely to change soon, with a new specialty training law being drafted in Spain, drawing on the UK's current model with 2 years of foundation training prior to entry specialist training with a four year duration (Law SCO/1198/2005).
In England, prospective trainees are judged on the basis of an initial application form, then a multiple-choice exam, and finally an interview with a strong focus on certain competencies. The process was described as competitive but generally fair: “It is really good, I would say it is probably the most structured, most organized, most fair and most evolved application process of all the specialties and almost kind of enjoyable to do” (UK03). With the inclusion of foundation years training, it means that five years of post-graduate training are required to become a GP in the UK, although the actual ‘GP vocational training scheme is only three years. In addition, the mandatory two-year foundation training programme, which precedes the standard three years of GP vocational training, often includes four months in general practice. Four-year GP vocational training programmes are being piloted in certain parts of the UK and proposals to increase training to five years have also been explored. The possibility of extended training was perceived positively by most GPs interviewed: “I think the extension of the GP training is a good thing. I think three years is not long enough to get all of the experience that you need to in a way that you continue learning on the job, glad that it has been recognized and I certainly found that the additional year was very useful” (UK10).
Continuing professional development (CPD)In Germany, where there is a strict division between doctors caring for inpatients in hospitals and those providing outpatient (ambulatory) care, which include GPs, a point-based CPD system is obligatory for all doctors who provide ambulatory care to patients covered by Social Health Insurance (SHI), who comprise the majority of the population. Interviewees reported being required to pursue a number of approved theoretical and practical courses, presenting evidence of participation to the regional medical chambers every five years. Those failing to do so may be punished with a reduction of reimbursement and, if they fail to show evidence of sufficient training within a further two years, their licence can be withdrawn.
GP in England must complete 250hours of CPD in a 5-year period. They are appraised annually and undergo revalidation (renewal of licence to practice) every 5 years, based on a portfolio of evidence, including reflective notes on participation in CPD, audit, quality improvement activities, analysis of significant events, evidence of team working and patient feedback.
GPs in Spain related difficulties in undertaking CPD activity due to recent budget cuts, increased workload and reduced time. More newly qualified GPs also reported concerns about lack of support for professional development at their workplaces. There is little or no protected learning time, particularly for those employed on short-term contracts or locum posts. Continuous training was often referred to as a ‘personal decision’, as there is no compulsory minimum number of CPD hours in Spain. Professional societies have varied training courses, some of which are either free of charge or at a low price for their members (but membership fees apply). Pharmaceutical companies sometimes offer free courses, but most Spanish interviewees expressed unhappiness with industry involvement in the organization of training: “It is a very important thing that continuous training attendance stops being oriented by pharmaceutical industry. They eliminated most of the continuous training. There is just very little continuous professional training offered” (SP03).
Scope of practice1) GP practice organization and multidisciplinary teamsIn Spain, most GPs are employed under salaried contract in the public health care system and work in primary health care centres. Registration with the Regional Medical Council is compulsory. Spanish interviewees described how changes in hierarchical structures (e.g. between physicians and nurses) encouraged multi-professional team working in primary care. In Spain there are also community paediatricians, dentists and midwifes, and occasionally physiotherapists, working in the same building. Most Spanish interviewees described team working as advantageous: “It is an advantage that we are unaware of, but we have it here” (SP08). However, there were concerns raised regarding coordination between primary and secondary care.
In contrast, in Germany most GPs are self-employed, working in office-based solo practices, although some work in group practices or in health centres. To be allowed to provide services billable to the SHI, based on a complicated mix of capitation and fee for service, they must be accredited by the Regional Association of SHI Physicians. All but one interviewee reported employing medical assistants (‘Arzthelferin’) who complete three years of vocational training, and whose role combines administrative and some minor clinical tasks (e.g. measuring blood pressure). The GPs described themselves as employers who delegate tasks: “I am the head of the practice and I am actually responsible for everything. But I have three employees and of course I try to delegate part of my work, everything there is to do in terms of office work. Besides my medical work I am also the employer, the boss, I am responsible for my practice, also for the management of the business” (DE05). Two German GPs described how their medical assistants undertook advanced training to extend their competencies to enable them to conduct home visits, case management, medication review and prevention activities.
This has some features similar to England, where partners in GP practices have a contract with the National Health Service (NHS) and may employ other GPs on salaries, and other health professionals such as nurses and administrative staff. Interviewees in England reported collaborating “fairly closely” with other healthcare professionals, particularly in larger general practices which usually have expanded capacity for allied healthcare workers including drug/alcohol workers, psychologists and district nurses. There are also increasing numbers of general practices where hospital specialists run outpatient clinics in the community.
2) Administrative vs. clinical dutiesIn all of the countries, administrative tasks are reported to occupy increasing amounts of a GP's time. In addition to the traditional administrative tasks, such as processing referrals, laboratory results, and correspondence from hospitals, English GPs seemed to have an especially heavy load, including extensive performance reporting, audits, meetings with patient groups, and engagement with the local clinical commissioning group. These GPs reported that they spent roughly equal amounts of time on administration and clinical work: “50–50 time spent between patients and managerial tasks” (UK01). The amount of administrative work may vary between partners and salaried doctors. Salaried doctors may have heavier clinical workload whereas partners may take on more of the administrative responsibilities related to the management of the practice.
German GPs also complained of a heavy administrative workload, but it was less than in England “...more than one hour per day. Six to eight hours per week, at least. You can easily count on seven hours for administrative things, this is madness” (DE03). Spanish GPs also reported spending too much time on administrative tasks and further highlighted the increasing administrative workload arising from patient's requests for certificates for incapacity/benefit claims and fitness to work assessments.
Ethical dilemmasIn each country, GPs described having to deal with ethical challenges. In Germany, a common theme was how to support end of life decisions and the possibility of having medically assisted suicide in the near future. One participant referred to the ethical challenge of caring for dying patients who are “held back [kept alive] by machines”. Another GP mentioned “an ethical issue that might arise in the future is most certainly the care and treatment of the continuously growing elderly population” (GP07), particularly “dying and medically assisted suicide to those whose situation is hopeless and who don’t want to be in this world anymore (GP07)”.
Spanish GPs expressed concern about recent changes in entitlement to care for undocumented immigrants and the impact of austerity measures on patients’ health and healthcare provision. The issues most often mentioned included the inability of patients to afford the newly introduced co-payments and their unwillingness to exclude undocumented migrants from accessing primary health care services.
In England common concerns included patient confidentiality and consent, rationing of healthcare due to scarce resources, dealing with what were seen as inappropriate requests by patients, and balancing patient needs with respect for autonomy and choice. There was general agreement that GPs in England are under pressure: “...to curtail referrals [to hospital], also not to prescribe certain drugs because they are too expensive” (UK01).
Things that need improving and future challengesThere was widespread concern in all countries that increased bureaucracy reduced the time for patient care. A Spanish GP highlighted that “Our work is based on the relationship with the patient, and the relationship has deteriorated for sure because there is no time and no energy” (SP02). In Germany, younger GPs criticised what they saw as structural failures in their training, such as lack of professional guidance and too many rotations. In both Germany and Spain, participants cited the need to improve communication across the primary secondary care interface. Spanish GPs highlighted the consequences of the austerity measures, which they saw as having little clear rationale and impacting adversely on population health and quality of care.
A number of English GPs were also concerned about the Quality and Outcomes Framework (QOF).30 QOF is a payment scheme designed, in theory, to reward high quality care, with payments for performance against a package of quality indicators, such as control of certain chronic conditions and implementing preventative measures, but also some managerial measures. Although the scheme is voluntary, in practice almost every GP signs up to it as provides up to 30% of the practice's income. GPs argued that, although the rationale behind “balancing the perceived health needs of one individual against those for a whole population and the resources” (UK10) may seem obvious, “Referral behavior is very complex and it's very difficult to judge in practice on how they perform just by looking at how much they refer” (UK01), leading to concerns about whether it is leading to rationing of necessary care “GPs are being paid not to do things that they think may be appropriate. So… being paid to reduce your referrals to hospital is not acceptable” (UK09).
DiscussionWe explored similarities and differences in GP training, scope of practice and GP's perceptions across three EU Member State countries which differ in the organisation of their primary care systems. We identified notable differences in the training and scope of practice of GPs in the three countries, such as the application processes for entering GP training and length of postgraduate training but also some similarities and common challenges.
Strength and limitationsStrengths of this paper include its comparative research on a sample of European GPs, exploring several aspects of their training and practice. Furthermore, participants included a varied group of doctors, working in different primary health care settings, at different levels of seniority. We were able to undertake an in-depth analysis of their experiences and expertise on a series of topics, some of which were quite sensitive, such as the ethical dilemmas faced in their day-to-day practice. However, as the interviews were conducted in different languages and translated for the analysis there was a risk of missing details and contextual information, although where possible statements were verified through desk research.
An additional strength of the paper is that it provides the current state of affairs of GP training and scope of practice among European countries.
There is widespread agreement on the importance of engaging in continuing professional development, and mechanisms to do so were present in all countries although to varying degrees. It is considered “voluntary”, with no minimum number of credits in Spain but is compulsory in England and Germany. In addition, the UK and Germany have revalidation systems in place, although the former goes beyond that in any other European country.9 The more holistic assessment of clinical competencies and personal attributes used in England was seen as fair and effective, consistent with previous studies.31–33 In Spain the government approved a law that envisages the introduction of mandatory CPD and revalidation at regular intervals,34 although this has not yet been put in place, hindered in part by a lack of funding consequent on austerity measures.
The differences that have been described in this paper relate to the different ways the health care system is organized and funded in each country, as well as how GPs’ responsibilities and roles are defined. Key differences included whether GPs work in multidisciplinary teams or singlehandedly; and the varying time devoted to administrative and clinical activities. However, our interviewees also shared common concerns and challenges such as the need to adapt services to an ageing population (with increasing challenging multi-morbidity and thus polypharmacy), the need to improve coordination between primary and secondary care, the lack of time for patients and the ethical dilemmas that arise in their daily practice.
One clear difference related to how the financial crisis is affecting GPs’ ability to provide services. Whilst few German GPs spontaneously mentioned the issue, English GPs raised concerns about budgetary pressures, within which they included the QOF, even though this is formally seen as a means to improve quality, whilst Spanish GPs emphasised new co-payments and denial of access to healthcare by migrants 35. The latter issue may become a greater concern in England following the passage of legislation similar to that in Spain.36
It is important to note that the interviews were conducted before the UK voted to leave the European Union. This paper, therefore, adds to the evidence of the extreme complexity that the UK will face in disentangling itself from the existing arrangements. Health professional mobility will be a particularly challenging issue, given that many of those who voted to leave sought to prevent free movement of people, yet the National Health Service in the UK depends substantially on health professionals from other Member States. Moreover, this is happening a time when it is facing other major problems as a consequence of the referendum vote, such as increased costs of pharmaceuticals resulting from the large decline in the value of sterling.
It remains to be seen how the UK will address this issue, given the difficulty reconciling the wide range of views within the government at Westminster as well as the very different views in two of the nations of the UK, Scotland and Northern Ireland, which voted to remain. Thus, it is not yet clear that it will be possible to achieve a national consensus, let alone one that will be agreed by the remaining 27 member states. Many of them will also be affected by whatever the UK decides, given its status as one of the preferred destination countries among GPs across the EU. It is, however, clear that this vote has created enormous uncertainty, with very damaging consequences already emerging for British research. It will be important for the British authorities to provide some clarity as soon as possible to minimise the damage but, given their internal disagreements, this will be extremely challenging.
Ethical issues discussed by participants reflected distinct issues in the three countries at the time of the interviews. The combined findings are in line with a comparative literature on ethical difficulties among physicians across Europe.26,37
These differences have practical implications. As noted in the literature,38 GPs who are interested in moving to another country should be provided with information on the new health care system in which they will be practising and this should include ethical and professional regulatory frameworks.
Although mobility of both health professionals and patients has increased, comparative research on the scope of practice of health professionals has so far been limited. There is a clear need for a much better understanding of the scope of general practice across Europe. Regardless of differences in primary care systems and cultural and historical context, GPs in each country face common challenges such as lack of time for patients, financial constraints, difficulties in coordination of services, working in multidisciplinary teams, as well as the issues arising with an ageing population. Finally, it is important to note that the differences identified in this paper have strong historical roots, grounded on the different national experiences.
The current EU Directive 2005/36/EC has established a minimum training duration for post-graduate medical qualifications, leaving definitions of skills required and scope of practice to national authorities. Increased mobility of health professionals and lack of standardization is leading to concerns regarding fitness to practise safely in another European country and quality of care. However, there is little comparative research on GPs across Europe.
What does this study add to the literature?This paper seeks to address this gap by examining the commonalities and differences in training, continuing professional development, scope of practice, ethical issues and areas that could be improved in England, Germany, and Spain. Regardless of the differences in primary care systems, GPs in each country reported facing common challenges such as the lack of time for patients, financial constraints, difficulties in coordination services, the need to work more effectively in multidisciplinary teams, as well as the issues arising with an ageing population. This paper maps out the situation as at 2015, prior to the UK's referendum on membership of the EU although the implications of this vote remain extremely unclear, although in the worst scenario, they could see many of the existing EU arrangements and legislation to assure professional mobility dismantled, to the severe disadvantage of the UK.
Clara Bermúdez-Tamayo.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsConceived and designed the study: HLQ, MM. Conducted the interviews: HLQ. VS, IRG Analyzed the data: all authors. Wrote the first draft: KG, HLQ, VS, Contributed to writing subsequent drafts: All authors.
FundingThis work was supported by the European Union 7th Framework Programme EU Cross Border Care Collaboration (EUCBCC). Contract no: 242058. Sole responsibility lies with the authors and the European Commission is not responsible for any use that may be made of the information contained therein. The funder played no role in the design of the study, the interpretation of the findings, the writing of the paper, or the decision to submit.
Conflicts of interestNone.
The authors wish to thank all GPs who agreed to be interviewed and gave their time and views.