The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosmenstrual pain is a common gynecological symptom at women on or near their menstrual period. Two third of them experienced moderate to severe pain. However, just several seek for medical help. This research aims to know the effect of ginger oil used on decreasing menstrual pain scale.
Materials and methodsthis cross over experimental study was held from February until May 2020 on 64 grade XI high school students at Palu city. Participants were grouping cluster randomly into group A which applied 5ml ginger oil five days before until the second day of the first menstrual period, and group B that given the same treatment in the next period. A visual pain scale measured the pain scale on the second day of the menstrual period.
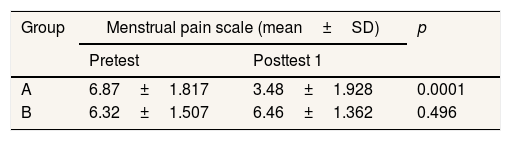
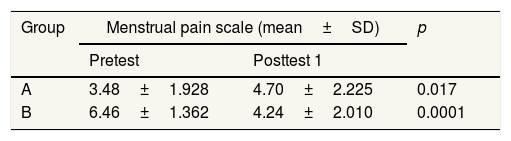
Resultmost participants were in the age of 17 years old. The study found a lowering of pain scale significantly at both groups after treatment. The main menstrual pain scale were 6.87 ± 1.817 and 6.46±1.362 decreased to 3.48±1.928 and 4.24±2.010 after treatment (p=0.0001). Differences between the two groups were significant in the first period (p=0.0001) but not significant in the second period (p=0.410).
Conclusionthe use of ginger oil several days before menstruation can reduce menstrual pain scale on students with primary dysmenorrhea; therefore, its use can be recommended to prevent the pain.
Menstrual pain is a common gynecological symptom affected by up to 90% women around the world.1 pain is felt like a cramp in the lower abdomen, thighs, and waist2 a few days before or in menstrual period. Most women who experienced menstrual pain have reported moderate to severe pain.3 Other studies also showed the same result.2 This is in line with our preliminary survey to determine the prevalence of menstrual pain among high school students in Palu city. Our finding showed 95% of students had experienced menstrual pain. 29.6% of students reported severe pain and 47.2% moderate pain, while mild pain was reported only by 18.2% of students. Menstrual pain on primary dysmenorrhea is due to the rise of prostaglandin leakage in endometrium.4 Prostaglandin is inflammatory agent,5 so it theoretically can be handled by the non-steroid anti-inflammatory drug. Treatment is aimed to relieve the pain.
Moderate and severe pain can disturb daily activity; however, most women prefer to self-treatment than seeking for health worker assistance to relieve pain.6 Based on the clinical algorithm for the treatment of primary dysmenorrhea in the nurse practitioner journal, treatment can be carried out pharmacologically, and nonpharmacological.7 Drugs that are often taken to relieve pain are ibuprofen,8 paracetamol, buscopan,9 syncopal and naproxen.10 63% women on a study reported no improvement after taking drugs.8 That leads women to turn to nonpharmacological treatment. Two-third of women reduce their menstrual pain with herbal medicine.11 Some herbal plants considered effective on relieving menstrual pain are ginger, parsley, mint, coriander, cinnamon, chamomile, turmeric, celery seeds, and fennel.12,13 Ginger is one of the herbals that has been considered effective in relieving menstrual pain.14 It has equal effectiveness as mefenamic acid and ibuprofen to reduce menstrual pain.15
Ginger also can be used topically to reduce pain.16 Some studies found ginger compress is effective in relieving menstrual pain scale.17 Our study is intended to determine the effect of ginger oil early on reducing menstrual pain scale at high school students. Ginger oil is made by the distillation process like other essential oil.18 In this study, ginger oil was used at night, starting five days before the menstrual period until the second day of the period. The finding of this study may provide the nonpharmacological choice for menstrual pain treatment for students.
Material and methodsStudy design and sampleThis cross over experimental study was held in Palu city from February until May 2020. The population in this study was grade XI high school student and randomized sampling clustery from SMAN1 Palu and SMAN 3 Palu. The inclusion criteria included age range 15–19 years old, had a regular menstrual cycle, and menstrual pain in the last three months, pain intensity was moderate to severe. They who had pelvic diseases, psychological problems, and refused given intervention were excluded from the study. The participants selected were assigned to two groups: group A (n=50), intervention is given in the second menstrual period, and group B (n=50), which is given intervention in the third menstrual period. They were evaluated at three menstrual periods; the first period in February was assigned as a pretest, the second and third period each were assigned as posttest one and posttest 2.
Intervention in this study was smearing 5ml of ginger oil on both soles of the feet, along the backbone, lower abdomen, and waist. It was undertaken at night13 for five days before the estimated first day until the second day of menstrual period19,20 for ten minutes. A research assistant helped the participant applying the oil. The first day of the period was estimated from the last three months menstrual cycle that confirmed at pretest. Group A was given intervention before posttest one, while group B was given before posttest 2. The menstrual pain scale was evaluated on the second day of the menstrual period or after the intervention ended. We used a pain visual analog scale to evaluate the pain by comparing the facial expression with the scale of pain from 1 to 10. This instrument has been applied in some studies to estimate menstrual pain.21,22 Review of three commonly used pain measures concluded pain visual analog scale as one of the valid and reliable instrument to use in clinical practice.23
Ginger oil used in this study was in commercial name varash, produced by PT Saddan Nusantara. The preparation is in the form of a 100ml plastic bottle. 5ml oil was equal with one bottle of cup preparation.
Ethical considerationThis study has been approved by the ethics committee of the public health faculty of Hasanuddin University. The Government National unity and politics department has also given permission for this study. The participant joined the study voluntarily after the procedure explanation was given. The informed consent form was signed before intervention knowing by proxy and teacher.
Data analysisData were computerized processing with the spss program. Wilcoxon signed-rank test was used to compare the menstrual pain scale before and after the intervention. Mann Whitney test was used to compare pain scale between two groups on posttest 1. Normally distributed data on group A was compared with paired t-test while independent t-test compared normally distributed posttest 2 data between both groups. A p-value of less than 0.05 considered significant statistically.
ResultThirty-six participants were dropped out during the study, remaining 64 participants until the end of the study. They were distributed in group A (n=23) and group B (n=41). The age of participants was in the range of 15–19, the most at 17 years old. They got their menarche on 10–15, the most 12 years old.
Table 1 shows that in group A, pain scale decreased from 6.87±1.817 before intervention to 3.48±1.928 after intervention (p=0.0001). It also decreased in group B from 6.46±1.362 on posttest 1 to 4.24±2.010 after intervention were given on posttest 2 (p=0.0001).
Pain measured in the second period of menstruation (posttest 1) showed a significant difference between group A and group B (p=0.0001), while no significant difference was showed in the posttest two measurements (p=0.410). But from Table 2, we can see the change of pain scale in both groups showed different patterns.
DiscussionOur study result showed there is ginger oil effect on decreasing menstrual pain scale. The effectiveness of ginger on reducing menstrual pain intensity has been approved. A pretest–posttest control group design study among college students found significant pain scale differences between control and group have given ginger tea.14,24 Another study among college students in pretest-posttest design also found the effect of red ginger stew on reducing menstrual pain intensity.25 Compared with another herb, ginger has the same effect with Rocella tea and turmeric on decreasing menstrual pain intensity.26
Ginger also has the same effect of relieving menstrual pain compared with a pharmacological agent. Randomized trials compare the effect of ginger, zinc, and placebo by Farzaneh Kashefi, et al. found that ginger had the same effect with zinc sulfate capsule on the improvement of menstrual pain in young women.27 On a randomized clinical trial by Marjan Ahmad Shirvani, they compared the effect of mefenamic acid and ginger to relieve pain in primary dysmenorrhea. The study concluded the same effect between both agent.28 Comparison study on double-blind clinical trial design also showed the same effectiveness between ginger, mefenamic acid, and ibuprofen in relieving menstrual pain.15,29 A cross over clinical trial also found that ginger is as effective as novafen in relieving menstrual pain.
Besides orally consumed, the topical use of ginger is also has a significant effect in reducing menstrual pain intensity. Topically, ginger can be used by compressing ginger extract on the site of pain. Ginger compresses were more effective than compresses of warm water to reduce the pain concluded in a study performed by Ati Karomika et al. Pre experimental study on one group pretest–posttest design by Harmawati also found significant menstrual pain difference before and after ginger compresses were given.30 Another pretest–posttest experimental study also found the effect of ginger compresses to decrease menstrual pain in MTs Hurul Huda.
In the above studies, ginger is as effective with other herbs and pharmacological agents in relieving menstrual pain, both consumed or topically used. In our study, ginger oil used is in preparation for oil. The distillation method used to produce ginger oil is the extracting technique using the vapor of boiled water.18 A study found the use of ginger oil was more effective to relieve pain than raw ginger.31
The main mechanism of menstrual pain in primary dysmenorrhea is myometrium hypercontractility and vasoconstriction triggered by the accumulation of prostaglandin, chemokines, cytokines, growth factors, and oxytocin.32 prostaglandin is inflammation substance which is synthesized from cyclooxygenase (COX).5 Non-steroid anti-inflammatory drugs (NSAID) prevent inflammation by inhibiting enzymes COX-1 and COX-2 that produce prostaglandin. It can explain how NSAID is used as the first-line treatment of menstrual pain. Gingerols and gingerdiones are two components of ginger that has an anti-inflammatory and anticarcinogenic role. They are COX inhibitor which inhibits leukotriene and prostaglandin synthesis.13 These COX inhibitor role of ginger components explain how ginger has effectiveness as NSAID drugs in relieving menstrual pain.
This study did not control other variables, which are risk factors of menstrual pain, such as dietary intake, daily activity, and psychological status, that can bias data collected. Another bias that can be occurred because the sample dropped out was more in group A. Limitation in this study is the absence of washout time in group A after the intervention that can affect comparison with group B in posttest 2. Subjectively evaluation of a facial expression in pain visual analog is another difficulty in this study. The strength of our study is intervention held starting before period comes to see prevention effect.
ConclusionThere was an effect of ginger oil in decreasing menstrual pain in primary dysmenorrhea of senior high school students when it used topically before the period comes. It can be an herbal treatment option for young women in relieving their menstrual pain. As this study did not evaluate the effect of long uses of ginger oil, we recommended the next research to examine it.
FundingThe material used in this study was 50 bottles of patent ginger oil, with commercial name varash, sponsored by PT Saddan Nusantara.
Conflict of interestThe author declares no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.