To identify the characteristics, motivations and employment implications among graduates of Masters programmes in health-economics (MPHE).
MethodThe most renowned MPHE in Spain were contacted to assist in this research study. Participants submitted an online survey comprising 30 items designed specifically for the purpose. Our sample consisted of 439 graduates. Different statistical analysis, including a logistic model, were performed to describe the sample.
ResultsThe main motivation for undertaking an MPHE is academic, and to acquire new or enhance previous knowledge. The general profile of graduates is that of a woman aged 37.8 and a health professional. Those looking for a job in Health Economics generally found employment in the first (54.9%) or second year (29.7%). MPHE were very highly assessed. The most useful subject was health management (46.3%).
ConclusionsUndertaking an MPHE is a good investment because most of the graduates believed that their training enabled them to find a job. The graduates showed a high degree of confidence in the usefulness of the training. MPHE are highly evaluated irrespective of consequent employment. The subjects in which the curriculum vitae of the health professionals were weaker, such as those concerning management, were evaluated the highest as they were assumed to enhance promotion opportunities.
Identificar las características, las motivaciones y las implicaciones laborales que aparecen entre los egresados de programas de máster en economía de la salud (PMES).
MétodoSe solicitó colaboración a los másteres más relevantes de España para esta investigación. Los participantes completaron un cuestionario on line de 30 ítems específicamente diseñado para este propósito. La muestra estuvo formada por 439 egresados. Se realizaron diferentes análisis estadísticos, incluyendo modelos logísticos.
ResultadosLa principal motivación para hacer un PMES es la académica. Las personas lo hacen con el fin de adquirir nueva formación o mejorar conocimientos previos. El perfil general de egresado es el de una mujer de 37,8 años, profesional sanitaria. Las personas que buscaban trabajo en economía de la salud lo encontraron principalmente en el primer (54,9%) o segundo (29,7%) año. La valoración de los PMES es muy elevada. La materia más útil fue gestión sanitaria (46,3%).
ConclusionesHacer un PMES es una buena inversión porque la mayoría de los egresados consideran que obtuvieron un empleo gracias a su formación. Los graduados muestran un alto grado de confianza en la utilidad de la formación. Los PMES son altamente valorados independientemente de las consecuencias laborales. Las materias en las que los curricula vitae de los sanitarios son más débiles, como las relativas a gestión, son las mejor valoradas, ya que suponen mejores oportunidades de promoción.
Traditionally, since the seminal contribution of Gary S. Becker (1964),1 the period of time dedicated to training is considered an investment, but in this case in human capital. In a classic sense, human capital corresponds to any stock of knowledge or other characteristics of the workers that contributes to their productivity.2 Even with this point of view, human capital is not only referred to as the school quality, it also includes personal attitudes towards work, and their capacity to adapt to different conditions.
For candidates it can be expected that increasing their training is one of the motivations for the people who apply for a masters programme in health economics (MPHE). It is a clear competitive advantage, for the people, the firms, and even the countries that increase their GDP.3 It has been proposed that human capital has a higher social return than investment in physical capital.4
Masters programme are a way to introduce a differentiation between candidates,5,6 and consequently people opt to do a MPHE in order to get into the job market. Ruiz-Adame7,8 in this sense found recently positive results in a similar study, but with graduates of masters programme in gerontology.
A (little) review of the development of health economicsAfter the Second World War, for the World Health Organization9 health became a necessary, and an indispensable condition for production making the management of health a priority for governments.10,11 Human capital12 and health care,13 the two historically large branches of the field, have yielded a large number of topics of interest in the most recent studies: social determinants of health, health systems and their institutional assessment, the supply and demand of health services, pharmacoeconomic, health technology assessment, and the analysis of incentives and behaviour of the agents that participate in the production of health.
The supply of specific training in this field began in the United Kingdom in 1983 (first edition of the MPHE at the University of York), and in the United States of America in 1989 in pharmacoeconomics.14 In the 20th century the necessity for specialists in this area became of great importance,15 and there has been an increasing demand for training by health agents in order to make decisions based on efficiency criteria.16 These criteria are of great importance when facing healthcare challenges.17
In Spain, health economics came into the spotlight during the 80's. In this period the assessment and management of hospital financing was applied to regional health systems.18 The master's programme at the Andalusian School of Public Health in Granada began in 1984, and the master's programme at the Pompeu Fabra University in Barcelona in 2004.
What we add to the knowledgeThe aim of this research has been to identify the characteristics, motivations and working implications that appear among the graduates in MPHE in Spain, so that we can ascertain which areas are the main focus for the graduates in the field of health economics.
With regard to other similar works previously published, as far as we know there is no other study such as the one that we have performed. The closest reference in Spain is the study by Trapero Bertrán and Oliva Moreno,19 who take the survey of Morrisey and Cawley20 as their starting point. They did a survey in 2009 of 285 members of the Spanish Association of Health Economics, two thirds of them defined themselves as health economists or health professionals who usually work on health economics issues. The results obtained by the authors in this study point to health economics in Spain as being a multidisciplinary activity that is not at all limited to the Schools of Economics and Management. Other interesting papers, although where the Spanish population is not represented, are those performed in the United States of America by Feldman and Morrisey,21 and more recently the study of Morrisey and Cawley.20 They analysed the main sociolabour characteristics of the health economist with a sample of 359 health economists.
In the United Kingdom, Kaambwa and Frew22 performed an online questionnaire in 2008 of 135 self-defined health economists who belonged to the Health Economists’ Study Group and the International Health Economics Association. The authors stated that the health economists’ motivation came from their previous experience during their undergraduate years, the availability of funding for master programmes, a special personal interest in the field, the necessity to enhance their personal careers, and the encouragement of their peers.
All the previous studies have focused on analysing the demographic, working, educational, salary and scientific production characteristics of people that are self-defined health economists or specialists in health economics and/or health management, independent of their previous educational background, and most of these studies were performed mainly in countries other than Spain.
Our study is based on a theoretical framework of human capital theory, which assumes educational training is an investment for individuals and organizations. We are adding to previous knowledge by way of looking at some variables that explain the motivations and how curriculum development contribute to professional outcomes, and additionally we add knowledge to the international research with data from a country where very little was studied previously. We consider these findings useful for policy makers and for a broad range of health and social disciplines in many countries.
The MPHE in Spain are traditionally a similar length of time as those of other countries, regardless of this very little has been studied about the profile of the people who work in health economics in Spain, and nothing, as far as we know, has been studied about the people who have done a specific training programme, such as a MPHE. As its main feature, this study has performed research in a geographical area, Spain, which focuses on the people who have done a training programme in health economics. The study has been done from the graduate perspective, with a broad sample and with the participation of the main MPHE. The study highlights new data on the graduate profile, their evaluation of these educational programmes, the impact the programme had on working conditions after graduation, and how the economic crisis of 2008 has affected the financing of this kind of training.
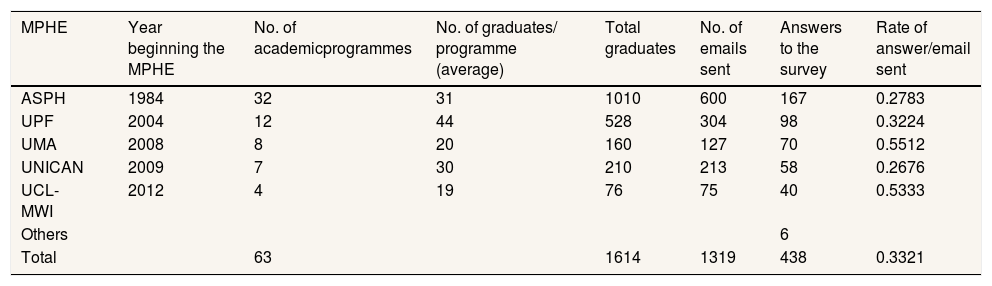
MethodsThe paper authors contacted the directors of the most renowned MPHE to request assistance in this research. Participants were mailed a letter explaining the purpose of the study by each university. The participants were anonymous and the researchers were completely blind to the personal data of participants, who voluntarily submitted an online survey comprised of 30 items designed specifically for the purpose. The master programmes and rate of answers can be seen on Table 1. The sample consisted of 439 graduates of MPHE.
Masters programmes in health economics that participated in the research. Rate of answer/email sent.
| MPHE | Year beginning the MPHE | No. of academicprogrammes | No. of graduates/ programme (average) | Total graduates | No. of emails sent | Answers to the survey | Rate of answer/email sent |
|---|---|---|---|---|---|---|---|
| ASPH | 1984 | 32 | 31 | 1010 | 600 | 167 | 0.2783 |
| UPF | 2004 | 12 | 44 | 528 | 304 | 98 | 0.3224 |
| UMA | 2008 | 8 | 20 | 160 | 127 | 70 | 0.5512 |
| UNICAN | 2009 | 7 | 30 | 210 | 213 | 58 | 0.2676 |
| UCL-MWI | 2012 | 4 | 19 | 76 | 75 | 40 | 0.5333 |
| Others | 6 | ||||||
| Total | 63 | 1614 | 1319 | 438 | 0.3321 |
ASPH: Andalusian School of Public Health; MPHE: masters programmes in health economics; MWI: Max Webber Institute; UCL: University of Castilla-La Mancha; UMA: University of Málaga; UNICAN: University of Cantabria; UPF: University Pompeu Fabra.
The items of the survey were organised in four big blocks: a) demographic questions; b) previous educational situation, working situation, and motivation for doing the MPHE; c) evaluation of the consequences of doing the MPHE in the labour market (only for those who found a job in health economics after the MPHE); and d) evaluation of the MPHE. We also included a last item in which participants could give an opinion or make an open comment.
AnalysisData was analysed using the SPSS-22 statistics software. Firstly, a descriptive analysis was performed to characterise the sample participants based on frequency measures for qualitative variables and central tendency measures (mean and standard deviations) for quantitative variables. Secondly, contingency tables were built to look for correlations using the chi-square test between qualitative variables under the usual parameters. Finally, binomial logistic models were undertaken to study the probability of occurrence of certain values. For the logistic models, we had previously proved the three underlying assumptions in the model: linearity, the independence of errors, and non multi-collinearity. The model of logistic regression guaranties linearity. For the second we performed the Durbin-Watson test (in all cases the data was between 1 and 3, and close to 2). For the third assumption we verified it through the inflate variance factor (in all cases the data was under 10, and close to 1).
ResultsThe graduates were from all over Spain and the years of finishing ranged from 1986 to 2016. The average year of finishing the MPHE was 2009 (standard deviation [SD]: 6.8). The general profile of the sample is that of a woman (55.5%) who was 37.8 (SD: 8.7) years old when she did the MPHE and currently is 44.5 (SD: 8.6) years old. Graduates came, on the whole, from health degrees (74.7%). The two most common educational backgrounds were in Medicine (37.0%) and in Pharmacy (19.2%). From the social sciences the most frequent previous training was in Economics (14.8%). Only 35.6% responded that they had ever had any kind of previous training in health economics.
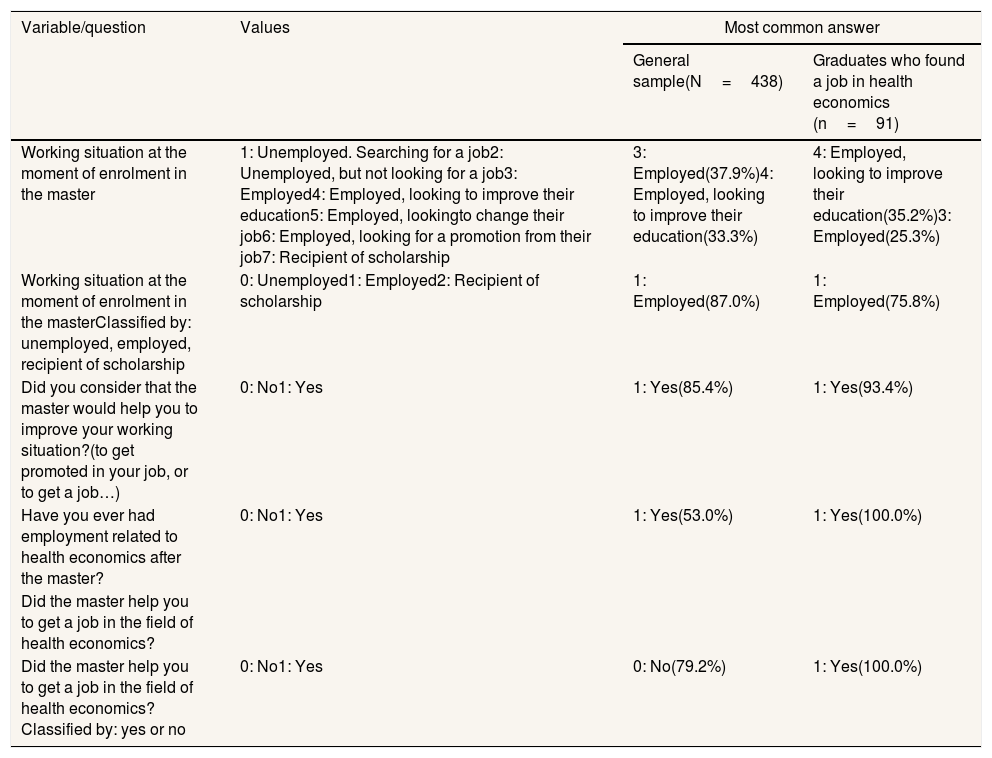
The principal motivation (44.1%) for doing the MPHE was to acquire new knowledge or to enhance previous knowledge (17.8%). Only 20.1% demonstrated that they did the MPHE for employment reasons: 12.8% to improve their employment opportunities and 7.3% to get promoted from their current position. Most of the sample (87.0%) were employed when they applied for the MPHE. The proportion increased (94.7%) when we asked for their current situation.
When we only analyse the profile of the people who have found a job in health economics after the masters (n=91, 20.7% of the sample) the profile is very similar to the general profile: a woman (57.1%), but slightly younger, of 34.3 (SD: 7.9) years old when she did the MPHE, and is currently 43.6 (SD: 10.3) years old. The average year of finishing the MPHE is 2007 (SD: 7.6). The graduates also mainly came from health specialities (74.7%). The two most common educational backgrounds were Medicine (35.2%) and Pharmacy (16.5%). From the social sciences the most frequent previous training was in Economics (15.4%). The prime motivation for doing the MPHE was also mainly academic (Table 2), by an even higher proportion (56.1%); 38.5% answered that they did it to acquire new knowledge or to enhance previous knowledge (17.6%).
Working situation and expectation of graduates. General group vs. graduates who found a job in health economics after the master in health economics.
| Variable/question | Values | Most common answer | |
|---|---|---|---|
| General sample(N=438) | Graduates who found a job in health economics (n=91) | ||
| Working situation at the moment of enrolment in the master | 1: Unemployed. Searching for a job2: Unemployed, but not looking for a job3: Employed4: Employed, looking to improve their education5: Employed, lookingto change their job6: Employed, looking for a promotion from their job7: Recipient of scholarship | 3: Employed(37.9%)4: Employed, looking to improve their education(33.3%) | 4: Employed, looking to improve their education(35.2%)3: Employed(25.3%) |
| Working situation at the moment of enrolment in the masterClassified by: unemployed, employed, recipient of scholarship | 0: Unemployed1: Employed2: Recipient of scholarship | 1: Employed(87.0%) | 1: Employed(75.8%) |
| Did you consider that the master would help you to improve your working situation?(to get promoted in your job, or to get a job…) | 0: No1: Yes | 1: Yes(85.4%) | 1: Yes(93.4%) |
| Have you ever had employment related to health economics after the master? | 0: No1: Yes | 1: Yes(53.0%) | 1: Yes(100.0%) |
| Did the master help you to get a job in the field of health economics? | |||
| Did the master help you to get a job in the field of health economics?Classified by: yes or no | 0: No1: Yes | 0: No(79.2%) | 1: Yes(100.0%) |
1: No. I have never looked for a job in this field.
2: No. I have not got a job in this field.
3: No. I was already working in this field.
4: Yes.
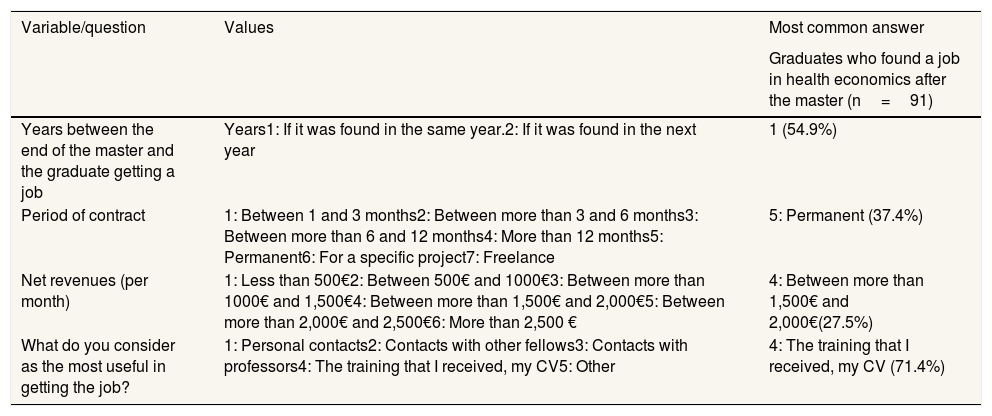
As seen on Table 3, the people who found a job did it mainly in the first (54.9%) or in the second (29.7%) year after finishing the MPHE. The employment was for long-term and stable positions. The most common type of contract was permanent employment (37.4%) and for more than 12 months (23.1%). The wages were most frequently between 1,500 € and 2,000 € (27.5%), but the second most frequent wages were higher than these figures, in this case they were between 2,000 € and 2,500 € (25.3%). The reason the people found a job in health economics after the MPHE was attributed, in a very high proportion (71.4%) to their personal training and their curriculum vitae. Only a low proportion attributed the fact that they had found a job to personal contacts (9.9%) or to contact with fellows (9.9%).
Characteristics of the job found by the graduates in the field of health economics (for those who found a job after the master in health economics).
| Variable/question | Values | Most common answer |
|---|---|---|
| Graduates who found a job in health economics after the master (n=91) | ||
| Years between the end of the master and the graduate getting a job | Years1: If it was found in the same year.2: If it was found in the next year | 1 (54.9%) |
| Period of contract | 1: Between 1 and 3 months2: Between more than 3 and 6 months3: Between more than 6 and 12 months4: More than 12 months5: Permanent6: For a specific project7: Freelance | 5: Permanent (37.4%) |
| Net revenues (per month) | 1: Less than 500€2: Between 500€ and 1000€3: Between more than 1000€ and 1,500€4: Between more than 1,500€ and 2,000€5: Between more than 2,000€ and 2,500€6: More than 2,500 € | 4: Between more than 1,500€ and 2,000€(27.5%) |
| What do you consider as the most useful in getting the job? | 1: Personal contacts2: Contacts with other fellows3: Contacts with professors4: The training that I received, my CV5: Other | 4: The training that I received, my CV (71.4%) |
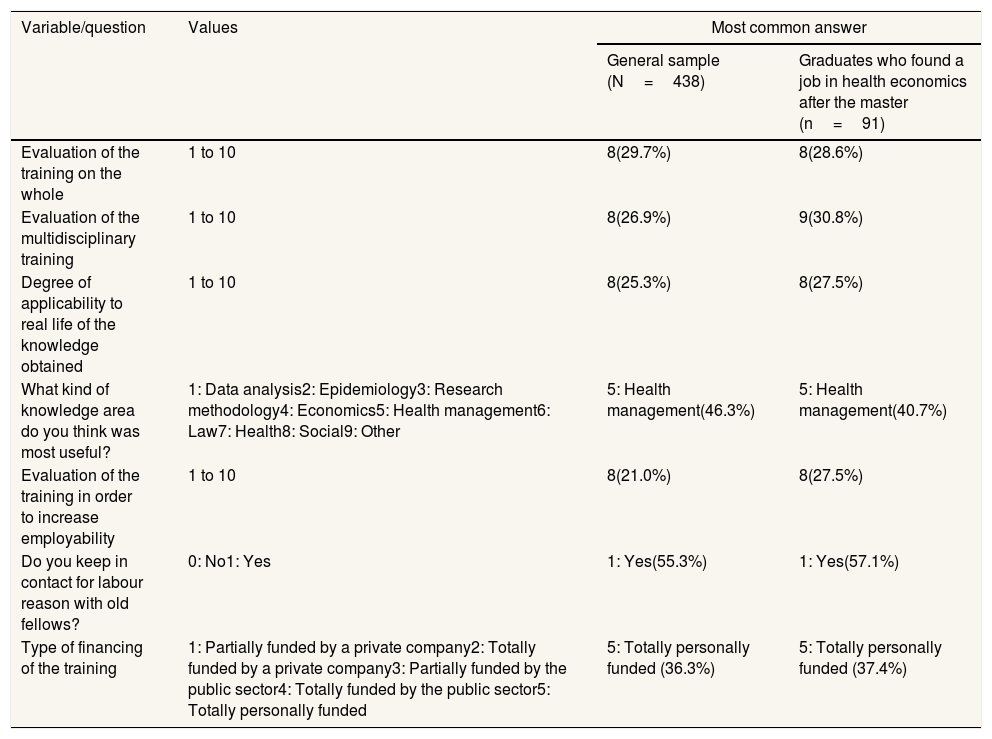
The evaluation of the MPHE was high as can be seen on Table 4. The area of knowledge that was considered as the most useful was health management (46.3%), followed by methodology of research (13.0%) and data analysis (12.6%). Either way, the MPHE seems to have a social aspect that remains after the end of the training; 55.3% of the graduates say that they maintain professional contacts and 62.3% also have social contacts with their classmate.
Evaluation of the master in health economics by the graduates. General group vs. graduates who found a job in health economics after the master.
| Variable/question | Values | Most common answer | |
|---|---|---|---|
| General sample (N=438) | Graduates who found a job in health economics after the master (n=91) | ||
| Evaluation of the training on the whole | 1 to 10 | 8(29.7%) | 8(28.6%) |
| Evaluation of the multidisciplinary training | 1 to 10 | 8(26.9%) | 9(30.8%) |
| Degree of applicability to real life of the knowledge obtained | 1 to 10 | 8(25.3%) | 8(27.5%) |
| What kind of knowledge area do you think was most useful? | 1: Data analysis2: Epidemiology3: Research methodology4: Economics5: Health management6: Law7: Health8: Social9: Other | 5: Health management(46.3%) | 5: Health management(40.7%) |
| Evaluation of the training in order to increase employability | 1 to 10 | 8(21.0%) | 8(27.5%) |
| Do you keep in contact for labour reason with old fellows? | 0: No1: Yes | 1: Yes(55.3%) | 1: Yes(57.1%) |
| Type of financing of the training | 1: Partially funded by a private company2: Totally funded by a private company3: Partially funded by the public sector4: Totally funded by the public sector5: Totally personally funded | 5: Totally personally funded (36.3%) | 5: Totally personally funded (37.4%) |
Lower punctuation means lower satisfaction.
Concerning the utility of doing these training programmes and the potential repercussion on the labour market, we analysed the relationship between doing the MPHE and finding a job after it. Contingency tables were performed. Correlations were found using the chi-square test. We use confidence levels of 1% and 5%. Although the two main handicaps to getting a job in health economics are: Being a woman (p=0.002, significant at 5%), and doing the MPHE after 2008 (p=0.000, significant at 1%). Education in a health degree still facilitated access to the job market in health economics (p=0.043, significant at 5%).
There is a significant relationship (p=0.000, significant at 1%) between those who gave a positive answer to the question as to whether previous to the MPHE they considered that doing it would help them in getting a job after graduation and obtaining one.
The main motivation, as previously stated was academic, and there is a positive correlation between this variable and getting a job (p=0.008, significant at 5%). But we did not find any significant association between getting a job and the time needed to get one, or the type of contract, or the revenue obtained for that job.
We studied the effect of the economic crisis of 2008 on the financing of education. The two main relevant factors seem to be doing MPHE previous or after the economic crisis of 2008 and the type of education (in the health field or the social field). We analysed the effect using a binomial hierarchical logistic model to predict if the dependent variable, the financing of training (totally or partially public vs private), could be forecast by these two variables.
The block 0 (empty model) shows that there is 50.2% probability of matching the results of the dependent variable, if we assume that every person finances the MPHE privately. For block one, the statistical efficiency test of ROA shows that there is a significant improvement (p<0.050) with the prediction of the probability of occurrence of the categories of the dependent variable for the variable crisis (chi-squared: 42.16; df: 1; p<0.001). The values of the R2 of Naglekerke are 0.122. We repeated the process and included the variable type of education. The statistical efficiency test of ROA shows that there is again a significant improvement (p<0.050) with the prediction of the probability of occurrence of the categories of the dependent variable for the variable type of education (chi-squared: 4.73; df: 1; p<0.005). The values of the R2 of Naglekerke increase to 0.135. Block 2 shows that there is 63.9% probability of matching the results of the dependent variable when we know the values of the variables crisis and type of education. The significant results that we have found are that those who did the MPHE after the crisis (B: 1.497; Exp(B): 4.469; Sig: 0.000) and those who had previous health education (B: 0.504; Exp(B): 1.655; Sig: 0.030) are more likely to privately fund their MPHE.
DiscussionMPHE in Spain have existed for a similar amount of time as the most prestigious MPHE in other countries but very little is known about the people who graduate from these specific training programmes. This is the first study in that sense.
From our data, health economics in Spain is a field of special interest for health professionals that are currently working and want specialised training in the field of economics and management. Surprisingly, very few economists are interested in this area of knowledge, this may be because very few have studied this subject during their university years.
The large proportion of working professionals could explain the high average age at the moment of applying for the MPHE. This is an investment that people do not make to get a job (only 12,8% declared doing the MPHE for that reason) but to improve the way they do their jobs.
Human capital theory says that individuals use their experience and education to signal their skills. This kind of investment gives a competitive advantage, consequently it should also be useful when getting a job in this area if you are not previously working in the field. This is what we have found. The majority of people who apply for a MPHE are already in work, but the people who are not and are looking for a job in health economics find one in the first or in the second year after finishing the MPHE. It is therefore a good investment because most of the graduates believe that they got the job thanks to their training.
Graduates show a high degree of confidence in the utility of training. We analysed the kind of financing and, most of the financing (50.2%) was in general private (partially or totally), this figure increased (59.9%) after the economic crisis of 2008. People, especially in the health sector, gamble on investing in training when the general economic situation is bad. This is in line with human capital theory which states that training helps to differentiate between candidates and allows better access to jobs positions.
On the other hand, the contents of the MPHE are highly evaluated independent of the job consequences. The subjects in which the curriculum vitae of the health professionals are weaker, such as those concerning management, are the best valued as they are assumed to enhance promotion opportunities. We think it could be as a consequence of a change in the orientation of the professional career from a clinical position to an executive role. The other two most valued subjects, methodology and data analysis, are linked to those profiles of people who use the MPHE training as a step towards getting into (or to enhancing) an academic career.
We have seen that the general profile of graduates is that of a female (55.5%), but there is still a statistically significant increased gender inequality in getting into the job market, that is greater for those who finished their training after the 2008 economic crisis. In the Spanish job market, the participation of women is lower than men, the employment rate for women is 42.15% and 53.20% for men23 and in this case, it seems that the difference also exists, though it is statistically significant that it is less of a differentiation than the general population. The proportion of women who found a job after the MPHE (48.7%) is closer to the statistic for men who found one (51.3%). Despite the gender handicap, doing a MPHE is a good investment for women who want to get into this field.
Finally, it should be into account that it is difficult to compare our results with other studies mainly because the previous studies that were performed in United States of America, United Kingdom or even in Spain are based on the characteristics of people who were self-declared health economists, independent of their basic education.
From our point of view, future research should deep in the gender differences. It would also be interesting to know more about the private job market in health economics.
Human capital theory states that education is a personal investment that it is a competitive advantage for the people and for the employers. Some studies performed in other countries have confirmed this statement. The closest study done in Spain about health economists was performed with a smaller sample and with people that did not have a specific training but they defined themselves as health economists. There are no descriptions of the profile of the graduates of the masters programs.
What does this study add to the literature?We have done the biggest study performed in Spain about the profile of the graduates, their motivations, labour consequences and valuation of the masters programs in health economics. We have found relationships between gender and labour consequences of this training, and we have identified which subjects are the best valued for the students.
David Cantarero.
Authorship contributionsMain author was responsible of the data collection. All authors have participated in the design of the methodology of the study. Ruiz-Adame was responsible of the data analyses and the writing of the manuscript. All authors have done a supervision and review of the manuscript.
AcknowledgementsThe authors wish to thank the directors of the masters programmes at the universities of Cantabria, Castilla-La Mancha, Málaga, Pompeu Fabra, and the Andalusian School of Public Health for their contribution. And specially to the Chair in Health Economics and Rational Use of Medicine University of Málaga-Janssen for its economic support. We also want to thank Katherine Burton for her writing and style advice.
FundingWe have received a grant of the Chair in Health Economics and Rational Use of Medicine University of Málaga-Janssen to pay the fee for publishing this paper.
Conflicts of interestNone.