The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoThis study aimed to assess the amount of changes in prevalence of stunting after one-year convergence intervention.
MethodsThis was an evaluation study of national program that implemented in Banggai District beginning 2018. There were ten villages (n=532) that included in the program based on severity of stunting prevalence. Data were analyzed using chi-square and independent t-test using SPSS.
ResultAfter a year program, stunting reduced to 38.91% or 2.18% from the baseline (41.09%). The highest reduction was in at 0–5 mo (8.59%) and 6–11 mo (8.46%). There was no difference using height for age z-score in all ages (−1.64±1.19 to −1.59±1.38, p=0.506). However, the reduction was significant at 0–11 months (−1.20±1.23 to 0.78±1.58, p=0.020) but no in other age categories (p>0.05).
ConclusionThe convergence action for one year intervention reduced significantly stunting in 0–11 months of children but not in other age categories of under five children.
Stunting is a serious public health issue experienced by children less than five years. Globally, the stunting prevalence in children was around 21.9% and more than half of them were in Asia.1 It was estimated that 1 out of 4 children under five years experienced growth failure optimally based on the growth standards by WHO.2 In Indonesia, the stunting prevalence was quite high around 30.8%.3 In 2011, the Indonesian government had made a strong commitment to stunting mitigation by joining the global Scaling Up Nutrition (SUN) movement as a global effort from some countries to strengthen the commitment and the action plan of scaling up nutrition,4 then it was strengthened by releasing the national strategy to accelerate stunting reduction and prevention (StraNas Stunting) using a multi-sectoral approach through a convergence program at all levels.5
Since stunting is a complex issue, it does not only need coordination from the health sector (specific) but also from the non-health sector (sensitive).1 Banggai district is one of the 100 districts in the implementation of the stunting convergence program. The stunting prevalence in Banggai is still high.5 The preliminary study conducted in 10 villages in Banggai District showed a higher stunting prevalence of 41.09%.
The effort of accelerating stunting prevention will be more effective if done in a convergent way.6 Globally, the integration of sensitive and specific interventions can reduce stunting prevalence of around 0.7–2.1% per year.1,7 The experience by several countries that had already succeeded in reducing stunting prevalence was based on a strong commitment from the government in arranging policies and the implementation, Sustainable political commitment, multi-sectoral approach, the organizational regulation at all levels, and the improvement of access to good quality health services.8 This study was intended to assess and evaluate the reduction of stunting prevalence after implementing the program of convergence intervention in Banggai district for a year.
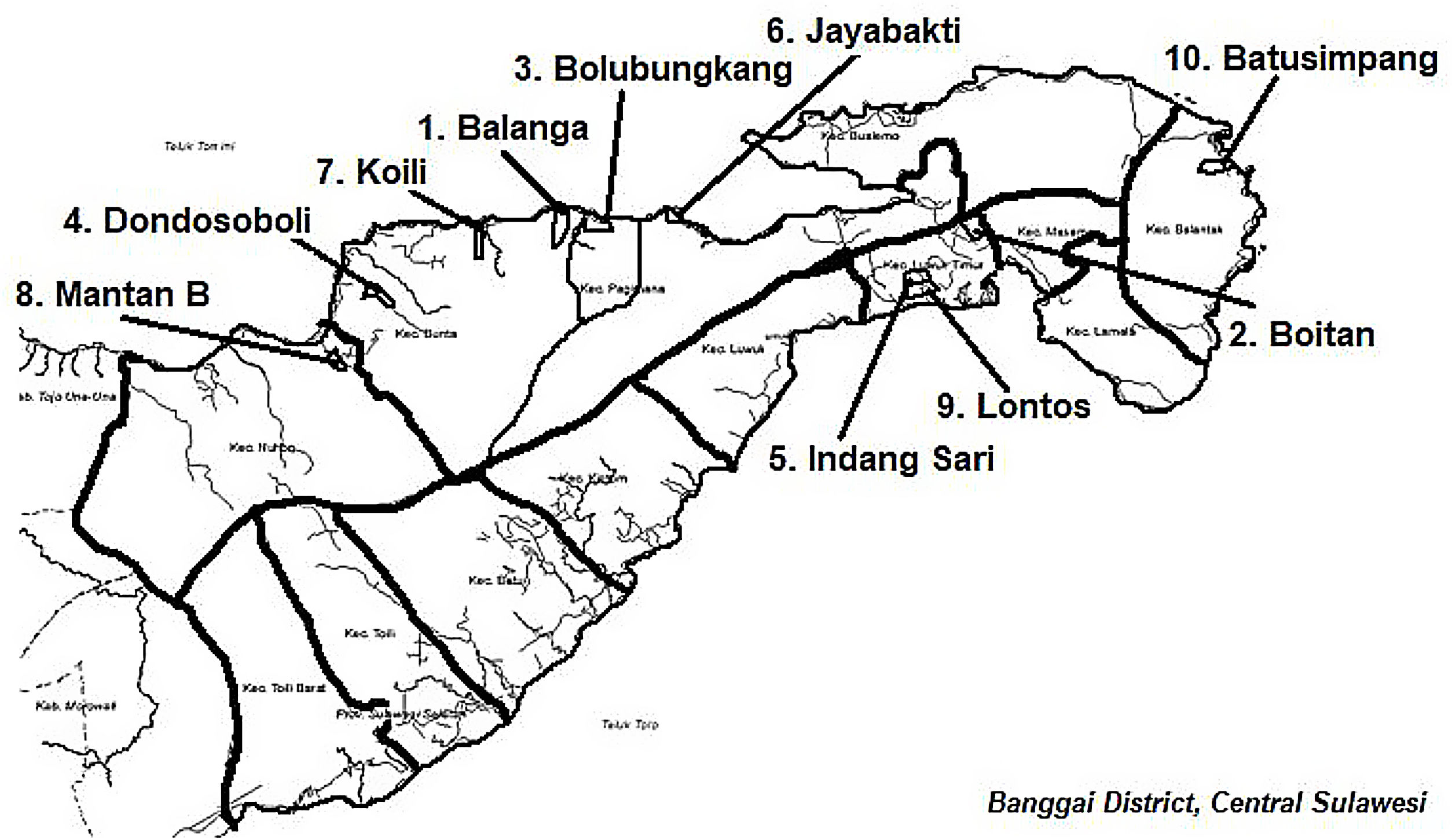
MethodsStudy design and participantThis was an evaluation study of a national program implemented in Banggai District at the beginning of 2018. Banggai district located in Central Sulawesi province, Indonesia, is one of the 100 priority districts/cities in Indonesia that should be intervened to mitigate stunting.9 This study was conducted in 10 selected villages with the highest stunting prevalence. Geographically, the location are scattered in some regions, namely mountains, flatland area, and coastal area, which their location is 40–150km from the district capital (Fig. 1).
Total of 550 under-five children in total were invited to participate at the beginning of the study. At the end of 2019, the anthropometric measurements were performed again to all under-five children the total was 532 under-five children that were measured. Furthermore, the ten villages received nutrition-specific and sensitive interventions in a convergent manner for a year.
Data collectionThe data were collected by trained field officers by following the standardized protocol.10 Anthropometric measurements for children under 2 years were done by using a portable length measuring board, while the measurement for children above 2 years was done using Microtoise as a height measuring instrument with a unit precision of 0.1cm. Based on the result of measuring the Anthropometric index for height-for-age (HAZ).
Data analysisThe WHO Anthro Software for 0–59 mo was used for calculating children's height/length z-score. Further, it was analyzed by using a Chi-square test and independent t-test. Data were analyzed using SPSS.
Ethical statementThis study obtained a clearance letter from the Institutional Ethics Committee of Public Health Faculty, Universitas Hasanuddin, Makassar. The informed consent was taken from each respondent.
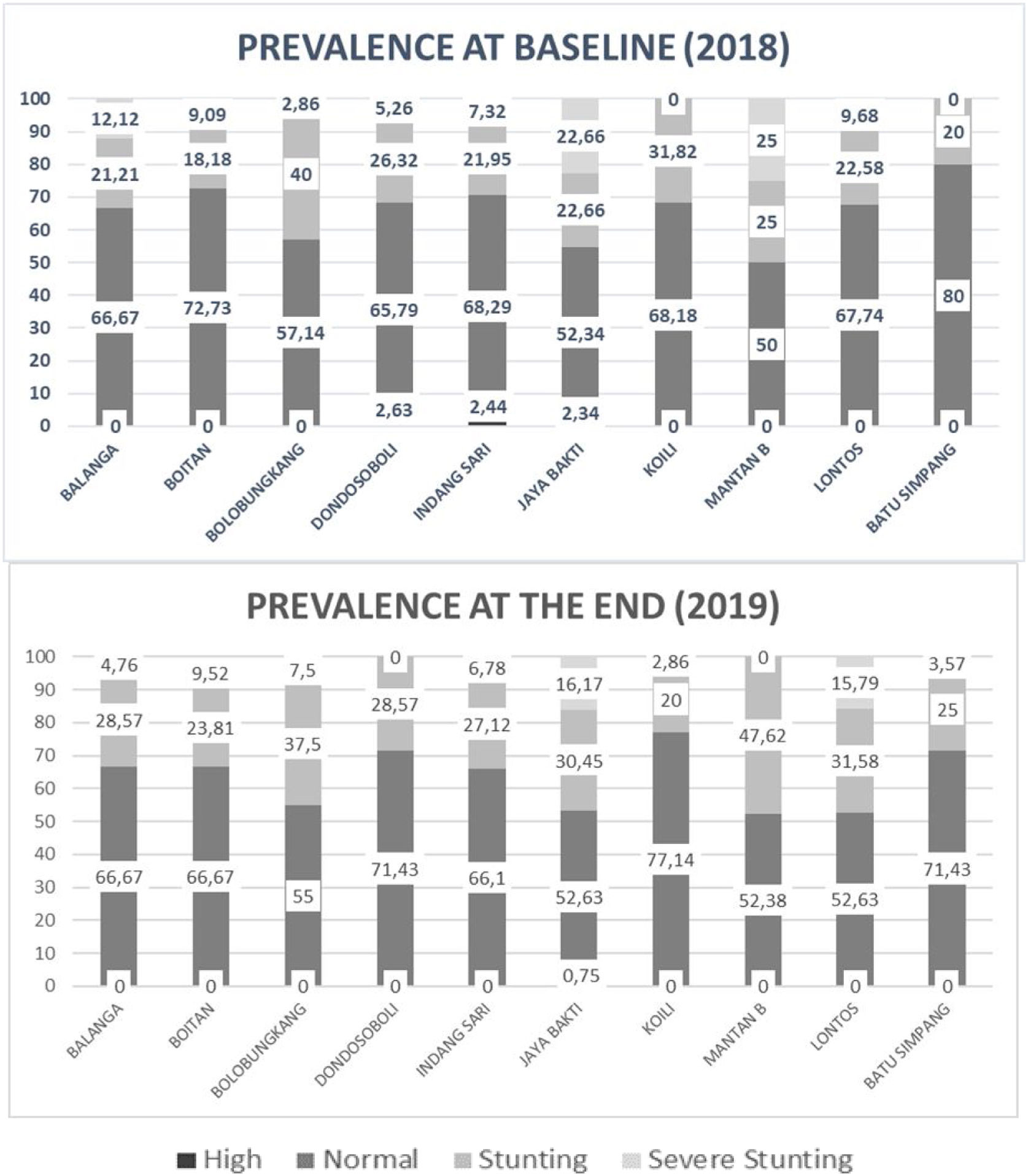
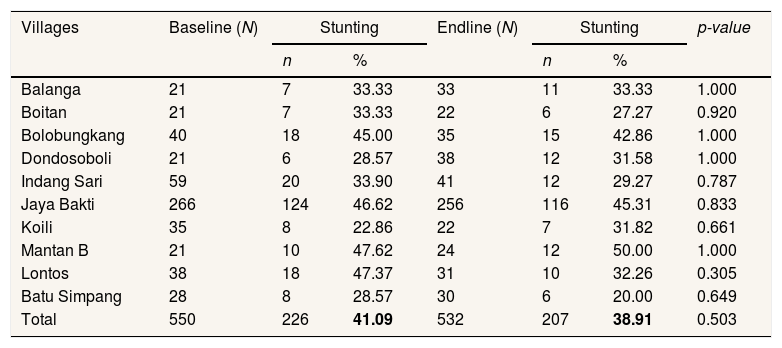
ResultNutritional statusFig. 1 shows an illustration of the prevalence of under-five children's nutritional status. The highest stunting prevalence was Mantan B village followed by Lontos and Jayabakti (47.62%, 47.37%, and 46.62% respectively). The illustration of stunting prevalence in 10 villages both before and after the convergence intervention in Banggai district can be seen in Table 1 (41.1% and 38.9% respectively). Cumulatively, the stunting prevalence was decreasing by around 2.18% for a year of intervention (Fig. 2).
The comparison of stunting prevalence in under-five children in 10 villages at baseline and endline.
| Villages | Baseline (N) | Stunting | Endline (N) | Stunting | p-value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Balanga | 21 | 7 | 33.33 | 33 | 11 | 33.33 | 1.000 |
| Boitan | 21 | 7 | 33.33 | 22 | 6 | 27.27 | 0.920 |
| Bolobungkang | 40 | 18 | 45.00 | 35 | 15 | 42.86 | 1.000 |
| Dondosoboli | 21 | 6 | 28.57 | 38 | 12 | 31.58 | 1.000 |
| Indang Sari | 59 | 20 | 33.90 | 41 | 12 | 29.27 | 0.787 |
| Jaya Bakti | 266 | 124 | 46.62 | 256 | 116 | 45.31 | 0.833 |
| Koili | 35 | 8 | 22.86 | 22 | 7 | 31.82 | 0.661 |
| Mantan B | 21 | 10 | 47.62 | 24 | 12 | 50.00 | 1.000 |
| Lontos | 38 | 18 | 47.37 | 31 | 10 | 32.26 | 0.305 |
| Batu Simpang | 28 | 8 | 28.57 | 30 | 6 | 20.00 | 0.649 |
| Total | 550 | 226 | 41.09 | 532 | 207 | 38.91 | 0.503 |
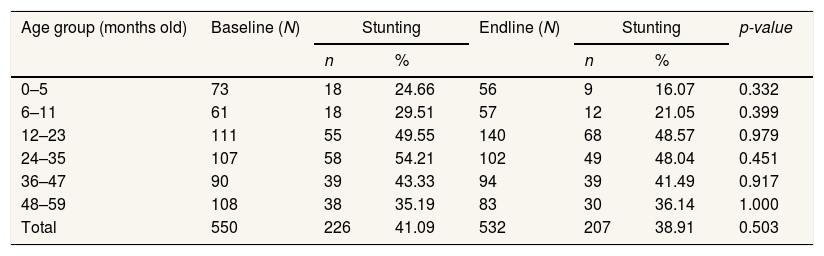
Table 2 shows the comparison of stunting prevalence before and after implementing the intervention program in a convergent manner based on the age group. The reduction of stunting occurred in nearly all age groups, except for the age group of 48–59 mo. The highest reduction was in the age group of 0–5 mo of around 8.6%; this shows that there is a reduction of stunting prevalence in newborn babies.
Stunting prevalence based on age group in under-five children in 10 villages at baseline and endline.
| Age group (months old) | Baseline (N) | Stunting | Endline (N) | Stunting | p-value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| 0–5 | 73 | 18 | 24.66 | 56 | 9 | 16.07 | 0.332 |
| 6–11 | 61 | 18 | 29.51 | 57 | 12 | 21.05 | 0.399 |
| 12–23 | 111 | 55 | 49.55 | 140 | 68 | 48.57 | 0.979 |
| 24–35 | 107 | 58 | 54.21 | 102 | 49 | 48.04 | 0.451 |
| 36–47 | 90 | 39 | 43.33 | 94 | 39 | 41.49 | 0.917 |
| 48–59 | 108 | 38 | 35.19 | 83 | 30 | 36.14 | 1.000 |
| Total | 550 | 226 | 41.09 | 532 | 207 | 38.91 | 0.503 |
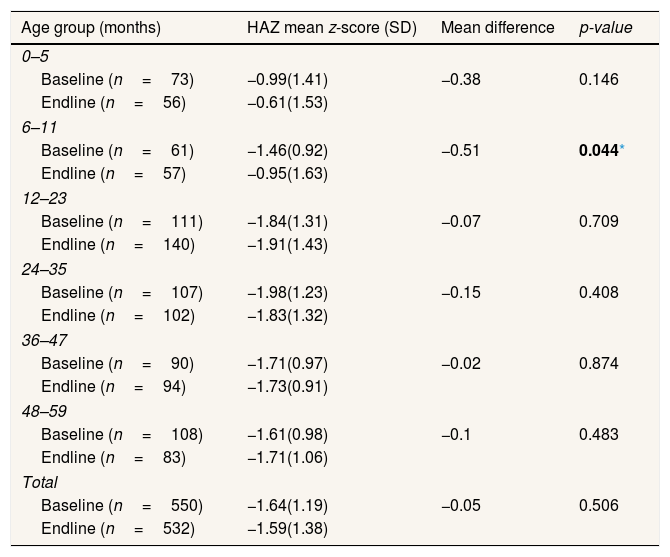
Table 3 shows the mean value and standard deviation from HAZ based on age group using the WHO standards. Generally, the z-score reduction was seen at the endline as they get older. Meanwhile, the highest increase of HAZ was in the age group of 48–59 mo. The lowest HAZ reduction was at the age group of 0–11 mo, whereby the HAZ score declined significantly at 6–11 mo (p<0.05). The HAZ score reduction at 0–11 mo illustrated the success of the intervention program in a convergent manner focused on the first 1000 days of life.
The difference of height-for-age z-score based on age group in under-five children in 10 villages in 2018 and 2019.
| Age group (months) | HAZ mean z-score (SD) | Mean difference | p-value |
|---|---|---|---|
| 0–5 | |||
| Baseline (n=73) | −0.99(1.41) | −0.38 | 0.146 |
| Endline (n=56) | −0.61(1.53) | ||
| 6–11 | |||
| Baseline (n=61) | −1.46(0.92) | −0.51 | 0.044* |
| Endline (n=57) | −0.95(1.63) | ||
| 12–23 | |||
| Baseline (n=111) | −1.84(1.31) | −0.07 | 0.709 |
| Endline (n=140) | −1.91(1.43) | ||
| 24–35 | |||
| Baseline (n=107) | −1.98(1.23) | −0.15 | 0.408 |
| Endline (n=102) | −1.83(1.32) | ||
| 36–47 | |||
| Baseline (n=90) | −1.71(0.97) | −0.02 | 0.874 |
| Endline (n=94) | −1.73(0.91) | ||
| 48–59 | |||
| Baseline (n=108) | −1.61(0.98) | −0.1 | 0.483 |
| Endline (n=83) | −1.71(1.06) | ||
| Total | |||
| Baseline (n=550) | −1.64(1.19) | −0.05 | 0.506 |
| Endline (n=532) | −1.59(1.38) | ||
This study showed the stunting prevalence in under-five children in 10 villages at baseline and endline of 41.1% and 38.9% respectively. There was a decline in stunting prevalence of 2.18% after the convergence intervention program for a year. Based on the age group, the highest reduction of stunting prevalence in children under one year was at 0–5 mo and 6–11 mo, namely 8.6% and 8.5% consecutively, even though, both reductions were not significant. Based on the height-for-age z-score, there was a significant difference between the score at baseline and the endline at the age group of 6–11 mo. In some countries, such as India, 20% of babies experience stunting before the age of 6 months.11,12 Health babies experience a maximum growth velocity since being born to the age of 6 months. The study conducted in Banggai district showed that Stunting prevalence in children under 2 years had more reductions, especially in children at 0–5 mo of 8.6%.
The reduction of stunting prevalence of 2.18% in a year had been appropriated with the success stories by some countries in mitigating malnutrition, such as Cambodia. Within 2000–2010, the stunting prevalence had been successfully reduced by only 1.03%.13 In Maharastra, India showed that stunting prevalence in children under 2 years had been declined 15.3% reduction for a period of 6 years with an average annual rate of reduction of 2.6%.14
The multi-sectoral intervention strategy in sub-Saharan showed that in three years, there was a consistent improvement in household food security and dietary diversity.15 Nearly 15% of mortality in under-five children will be declined if the nutritional intervention, both sensitive and specific, is implemented accurately.16 To prevent the children from having mental and physical health problems in the future, environmental conditions, and socio-demographic, such as population density and poor environmental conditions, should get close attention.14,17 Giving supplements, education on nutrition and the intervention of clean water supply, the improvement of basic sanitation, and washing hands practice will provide benefits for children's growth.18
The effort for stunting prevention in Banggai district had been performed in a convergent way. It can be seen from the involvement of several cross-sector, both government and private sector, including higher educational institutions, especially in planning, budgeting, and the implementation of the stunting reduction program. The commitment from the local government was quite high, whereby several regulations and policies had been issued in supporting the stunting reduction program. Moreover, the First 1000 Days Task Team had been formed to coordinate and integrate the program of the First 1000 Days of Life to be more directed and integrated with the form of an action plan of stunting prevention and mitigation in Banggai district.
One of the innovations made by Banggai district was Preconception Integrated Service Post. It is an approach and strategy by performing assistance toward women at preconception, a group of women of child-bearing age, both those who will be a bride or those who have married, to increase the nutrient intake of prospective mothers and pregnant mothers and reduce the causes of maternal mortality and child mortality as well as prevent stunting. The existence of Preconception Integrated Service Post was also based on antenatal care that was not maximum due to the delay on first ANC visit (K1) among pregnant mothers and the high number of anemic cases in mothers at pre-pregnancy (preconception).19 Consequently, the services for women at preconception become vital and they become a part of Maternal and Child Health Care Services (KIA) in Banggai district. Some services given are including education, anthropometric assessment, pregnancy, blood sample test, and providing multiple micronutrient supplements.
Preconception Integrated Service Post has provided a positive effect on stunting reduction in Banggai district. The result of the study conducted in Banggai district showed a significant reduction in the age group of 6–11 mo (p-value=0.044). This reduction was believed that there was an increase in contact by the officers before the respondents being pregnant, the increase in the number of visits when having K1 assessment, and the increase in mothers’ knowledge. Then, other studies showed the positive effect of MMN supplementation program in the period of preconception and pregnancy on the birth result, whereby the birth weight and birth length of the respondents who received MMN were better (p<0.05) that those who received IFA; the average newborn babies’ length in pregnant mothers in MMN group was longer than IFA group, namely 49.5cm.20
ConclusionReducing Stunting in 10 villages in Banggai district reaches 2.18% in one-year program implementation. The highest stunting reduction is under one year reaching 9%. This shows that a year of intervention can reduce the percentage of stunting in newborn babies and increase a significant improvement in the First 1000 Days of Life program.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.