The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoThis study aims to determine the risk factors of asphyxia neonatorum in two PONED Public Health Centers of Nosarara and Pantoloan, in Palu City, Central Sulawesi.
MethodsThis study used a case-control study design. Sampling was conducted by a simple random sampling technique. The sample size in this study was 60 samples. The data collected was secondary data from medical records at Nosarara and Patoloan Public Health Centers, Palu City. Multivariate analysis used to determine the main risk of the incidence of neonatal asphyxia.
ResultsThe results showed the Prolong Parturition OR=5.714 (95% CI 1.724–18.944); Prematurity OR=4.333 (95% CI 1.203–15.605); LBW OR=7.000 (95% CI 1.381–35.487).
Conclusionrisk factors for neonatal asphyxia were prolonged labour, prematurity, and LBW. The main factors causing neonatal asphyxia were LBW.
According to WHO (2018), asphyxia is the second leading cause of neonatal deaths worldwide.1 Based on the Health Profile of Central Sulawesi, in the Central Sulawesi Region in 2018, there were 385 cases of Neonatal deaths.2 While the Palu City Health Office in 2016, recorded neonatal deaths in Palu City were 16 cases with the most causes was asphyxia neonatorum which was 50%.3
Asphyxia neonatorum is a condition where newborn experiences gas exchange and oxygen transport disruptions, resulting in a lack of oxygen supply and difficulty in removing carbon dioxide.4 This condition is known as hypoxic-ischemic encephalopathy or HIE. In developed countries, around 0.5–1/1000 full-term infants born alive and experiencing HIE, and 0.3/1000 have significant neurological disabilities.5
A study beyond the organ damage in asphyxia infants showed 34% had no organ damage, 23% had one organ damage, 34% had damage in two organs, and 9% had damage in three organs. Other studies report the frequency of dysfunction of various vital organs, such as the brain, cardiovascular, pulmonary, kidney, gastrointestinal, and blood. The vital organs that are often affected are the kidneys (50%), brain (28%), cardiovascular (25%), and lungs (23%).1,6
Responding to this problem, to reduce MMR or IMR, extra effort is needed and requires commitment support from all parties, starting from the central, regional, health organizations, community, private sector, and NGOs, both national and international. One of the efforts taken in addressing this problem is through handling obstetric and neonatal emergencies/complications at the basic service level (PONED).3,7,8
Following the background that has been discussed, this study aims to determine the risk factors of asphyxia neonatorum in 2 PONED Public Health Centers of Nosarara and Pantoloan, in Palu City, Central Sulawesi.
Materials and methodsThis research was conducted in two of three PONED Public Health Centers in Palu, namely Nosarara Public Health Center and Pantoloan Public Health Center, in Palu City, Central Sulawesi Province, in May 2020. The type of research used was analytical observational with a case-control study design. The dependent variable of this study was asphyxia neonatorum, while the independent variable was a factor suspected to be a risk factor for the incidence of neonatal asphyxia, i.e., maternal age, upper arm circumference, haemoglobin levels, birth weight, gestational age, and time of delivery (parturition). The population of this study was all mothers who gave birth at Nosarara and Pantoloan Public Health Centers in Palu City, Central Sulawesi. A sample of 60 people was selected by simple random sampling with inclusion criteria, such as pregnant women who did labour in Nosarara and Pantoloan Public Health Centers, and have complete data needed by researchers. In the Nosarara Community Health Center, about 30 samples of mothers were given birth, and in the Pantoloan Community Health Center, about 30 samples of mothers were also selected. Data collected based on secondary data that was medical records of patients at Nosarara and Pantoloan Public Health Centers. The data then analyzed with a chi-square statistical test to describe the frequency distribution of each variable, while to assess the main risk factors for the incidence of asphyxia neonatorum, multivariate analysis of logistic regression tests was used.
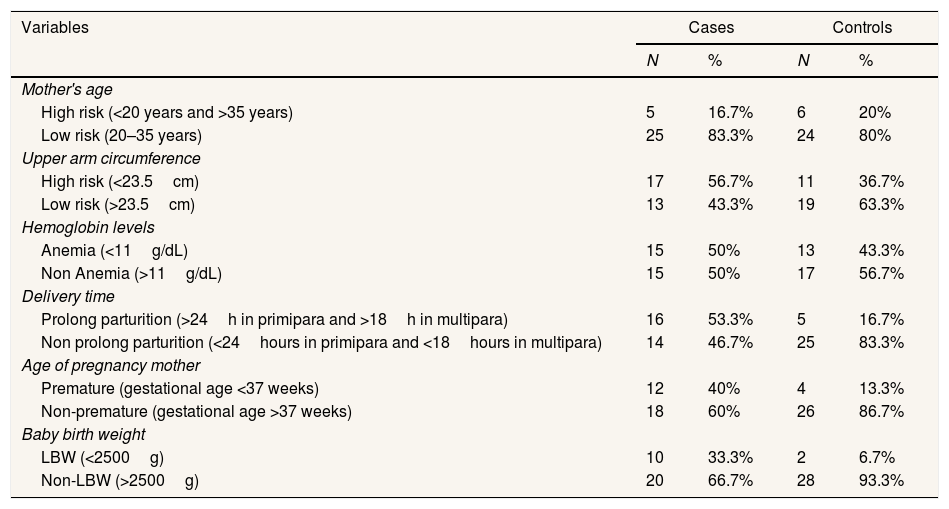
ResultRespondent characteristicsFrequency distribution of mothers giving birth at Public Health Centres of Nosarara and Pantoloan, Palu City, can be seen in Table 1.
Frequency distribution based on cases and controls.
| Variables | Cases | Controls | ||
|---|---|---|---|---|
| N | % | N | % | |
| Mother's age | ||||
| High risk (<20 years and >35 years) | 5 | 16.7% | 6 | 20% |
| Low risk (20–35 years) | 25 | 83.3% | 24 | 80% |
| Upper arm circumference | ||||
| High risk (<23.5cm) | 17 | 56.7% | 11 | 36.7% |
| Low risk (>23.5cm) | 13 | 43.3% | 19 | 63.3% |
| Hemoglobin levels | ||||
| Anemia (<11g/dL) | 15 | 50% | 13 | 43.3% |
| Non Anemia (>11g/dL) | 15 | 50% | 17 | 56.7% |
| Delivery time | ||||
| Prolong parturition (>24h in primipara and >18h in multipara) | 16 | 53.3% | 5 | 16.7% |
| Non prolong parturition (<24hours in primipara and <18hours in multipara) | 14 | 46.7% | 25 | 83.3% |
| Age of pregnancy mother | ||||
| Premature (gestational age <37 weeks) | 12 | 40% | 4 | 13.3% |
| Non-premature (gestational age >37 weeks) | 18 | 60% | 26 | 86.7% |
| Baby birth weight | ||||
| LBW (<2500g) | 10 | 33.3% | 2 | 6.7% |
| Non-LBW (>2500g) | 20 | 66.7% | 28 | 93.3% |
Note: Based on secondary data.
Based on Table 1, the most samples were 25–35 years old mothers (83.3%), that was in the case group. The upper arm circumference was >23.5cm, with 17 samples (56.7%) in the case group. Most haemoglobin levels were >11g/dL in both groups, 15 samples (50%) in each. Most of the time of delivery was 25 samples (83.3%), which was mothers who did not experience prolonged labour in the control group. Most of the gestational ages were 26 samples (86.7%) were mothers who gave birth with gestational age >37 weeks in the control group. The highest number of birth weight of infants was non-LBW infants of 28 samples (93.3%) in the control group.
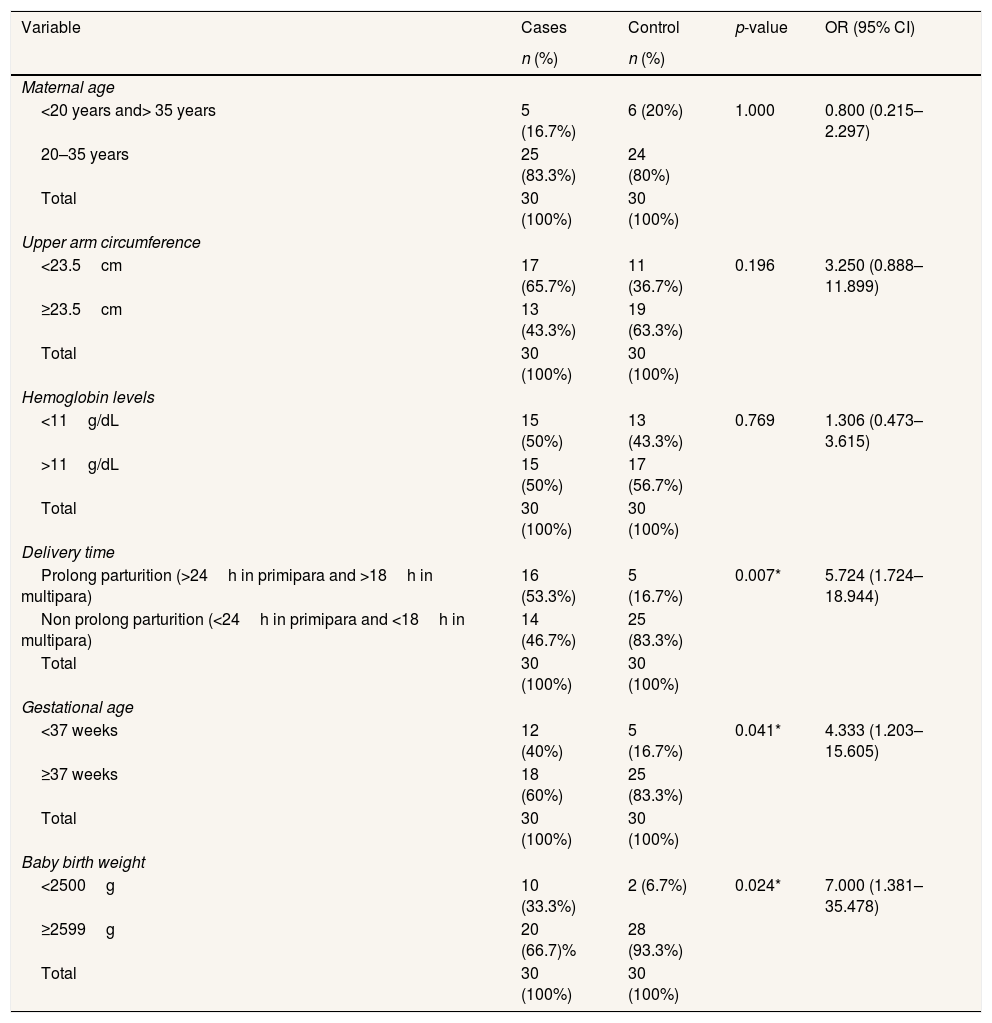
Bivariate analysis of the independent variables against the dependent variablesBivariate analysis was used to determine whether the dependent variable is a risk factor for the occurrence of asphyxia neonatorum, as displayed in Table 2 as follows.
Bivariate analysis of independent variables on the dependent variable.
| Variable | Cases | Control | p-value | OR (95% CI) |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Maternal age | ||||
| <20 years and> 35 years | 5 (16.7%) | 6 (20%) | 1.000 | 0.800 (0.215–2.297) |
| 20–35 years | 25 (83.3%) | 24 (80%) | ||
| Total | 30 (100%) | 30 (100%) | ||
| Upper arm circumference | ||||
| <23.5cm | 17 (65.7%) | 11 (36.7%) | 0.196 | 3.250 (0.888–11.899) |
| ≥23.5cm | 13 (43.3%) | 19 (63.3%) | ||
| Total | 30 (100%) | 30 (100%) | ||
| Hemoglobin levels | ||||
| <11g/dL | 15 (50%) | 13 (43.3%) | 0.769 | 1.306 (0.473–3.615) |
| >11g/dL | 15 (50%) | 17 (56.7%) | ||
| Total | 30 (100%) | 30 (100%) | ||
| Delivery time | ||||
| Prolong parturition (>24h in primipara and >18h in multipara) | 16 (53.3%) | 5 (16.7%) | 0.007* | 5.724 (1.724–18.944) |
| Non prolong parturition (<24h in primipara and <18h in multipara) | 14 (46.7%) | 25 (83.3%) | ||
| Total | 30 (100%) | 30 (100%) | ||
| Gestational age | ||||
| <37 weeks | 12 (40%) | 5 (16.7%) | 0.041* | 4.333 (1.203–15.605) |
| ≥37 weeks | 18 (60%) | 25 (83.3%) | ||
| Total | 30 (100%) | 30 (100%) | ||
| Baby birth weight | ||||
| <2500g | 10 (33.3%) | 2 (6.7%) | 0.024* | 7.000 (1.381–35.478) |
| ≥2599g | 20 (66.7)% | 28 (93.3%) | ||
| Total | 30 (100%) | 30 (100%) | ||
Based on Table 2, it was known that variables that have a p-value <0.05 were variables of delivery time (0.007), gestational age (0.041), and birth weight (0.024) so that they become risk factors for neonatal asphyxia.
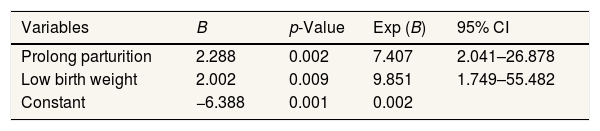
Multivariate analysis between risk factors for neonatal asphyxiaMultivariate analysis was used to determine the main risk factors for asphyxia neonatorum, as displayed in Table 3 as follows.
Table 3 displayed that of the three variables which were risk factors for asphyxia neonatorum, then reprocessed using a logistic regression test, then the outcome of the parturition variable and LBW was the most significant risk factors for neonatal asphyxia, with LBW as a major risk factor for neonatal asphyxia (9.851 times being risky) and prolong parturition contributed at 7.407 times being risky of asphyxia neonatorum.
DiscussionEffects of delivery time, gestational age, and birth weight of infants on the risk of neonatal asphyxia
Based on the results of the chi-square statistical test, the time of delivery in this case of prolonged labour was a risk factor for asphyxia neonatorum with a p-value of 0.007 (p<0.05). Mothers who experienced a prolong parturition were at risk of 5.714 times, giving birth to infants with neonatal asphyxia (95% CI 1.724–18.944). Related research results suggest that the time of delivery, in this case, is the prolonged parturitions, which is critical to discuss neonatal asphyxia.9,10 Mothers who experienced prolonged labour had 3.09 times giving birth to infants with asphyxia neonatorum (95% CI: 1.47–6.54).11 The results of the same study revealed found that mothers with prolonged labour showed the presence of a strong ratio of asphyxia neonatorum with a p-value of 0.012 and a risk of 6.27 times the risk of asphyxia neonatorum to the infants.11,12
Prolong parturition can also occur postpartum haemorrhage, which may cause death in the mother. In the fetus, there will be infections, injuries, and asphyxia, which can increase death in infants.13,14 Prolong parturition may also occur the emphasis on the umbilical cord during labour and when the mother is waiting.15 This can happen when there was prolonged labour or parturition, so the fetus is conceived by the pregnant woman.16,17
Based on the results of the chi-square statistical test, gestational age, in this case, was prematurity, was a risk factor for asphyxia neonatorum with a p-value of 0.041 (p<0.05). Mothers who gave birth to infants <37 weeks’ gestation had a risk of 4.333 times giving birth to infants with neonatal asphyxia (95% CI 1.203–15.605). The results of this study were in line with research conducted, suggesting that prematurity significantly influences the occurrence of asphyxia neonatorum. Mothers who give birth at <37 weeks contributed 3.778 times the risk of neonatal asphyxia in their babies (95% CI: 2.939–5.959).18 Findings revealed that each variable of maternal gestational age obtained a p-value of 0.001 (p<0.05).14,19,20 In premature babies, there is a surfactant deficiency that functions for lung development, so premature babies are very closely related to neonatal asphyxia.2,21
Following the results of the chi-square statistical test, the weight of babies born, in this case, was LBW, was a risk factor for asphyxia neonatorum with a p-value of 0.024 (p<0.05). LBW infants or bodyweight <2500g had seven times the risk of becoming asphyxia neonatorum (95% CI 1.381–35.478). The results of this study were in line with research conducted, which suggests that LBW infants had 5.17 times the risk of developing neonatal asphyxia (95% CI 2.62–10.22).5 This study was also in line with research conducted, Birth Weight of Babies has a significant effect on the incidence of neonatal asphyxia on p-values of 0.001 (p<0.05), with 2.46 times the risk of neonatal asphyxia.22 Similarly, research conducted suggests the same thing with a p-value of <0.001 (p<0.05) with 0.13 times the risk of neonatal asphyxia.23
Respiratory disorders often cause severe illness in Low Birth Weight Babies (LBW).12,24 This is due to a lack of surfactants, growth, and development of lung muscles that are still not perfect. Respiratory muscles are still weak, and the ribs are easily curved, so often associated with severe asphyxia and respiratory distress syndrome.25
Multivariate analysis between risk factors for neonatal asphyxiaThe multivariate analysis used was a multiple logistic regression test with the backward Wald method used to determine the most influential risk factors compared to other variables. In the final multivariate test results (Table 3), it appears that the main factor that most influences on neonatal asphyxia were LBW, which was 9.851 times, then the prolonged parturition was 7.407 times the risk of becoming asphyxia neonatorum.
ConclusionsBased on the results and data analysis, it was concluded that prolong labour, prematurity, and LBW were risk factors for asphyxia neonatorum at Nosarara and Pantoloan Public Health Centres, Palu City, Central Sulawesi Province. The main risk factor for asphyxia neonatorum in both Public Health Centers was LBW, which was 9.851 times. According to the risk factors that cause neonatal asphyxia, the mother who wants to plan a pregnancy or the mother who was undergoing the pregnancy process should pay attention to her health and the fetus. Those can be as nutritious food consumption to avoid the risk of LBW, which increases the risk of neonatal asphyxia. Besides, maintaining physical fitness with exercise under the conditions of pregnancy to prevent the risk of prolonged labour that increases the risk of neonatal asphyxia.
Conflicts of interestThe authors declare no conflict of interest.
The authors would like to thank for Dean and the all vice-dean the Faculty of Public Health at Hasanuddin University for the research funding.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.