Despite no evidence in favour, routine workers’ health examinations, mostly pre-employment and periodic, are extensively performed worldwide with important allocation of resources. In Spain they are performed within a theoretical job-specific health surveillance system. Our objective was to ascertain their occupational preventive usefulness from the perspective of occupational health professionals.
MethodsCross sectional study. Online survey addressed to all physicians and nurses members of the Catalan Society of Safety and Occupational Medicine (n=539) in 2011. Univariate and bivariate analyses of prevalence and prevalence differences of answers.
ResultsResponse rate 53% (n=285). According to more than 70% of respondents the health surveillance system isn’t cost-effective, doesn’t meet the goal of early detection of health damage related to work, and doesn’t contribute to improve the occupational risk prevention system. Further deficiencies were identified regarding specificity and scientific basis for health examinations, quality of collective health surveillance and referral of suspected cases to mutual insurance companies for diagnosis and treatment. Bivariate analysis showed a significantly more negative opinion for several items amongst physicians (versus nurses) and amongst professionals working in external prevention services (versus internal services).
ConclusionsThis study raises serious concerns about how health examinations are performed within our workers’ health surveillance system, which should be reviewed to ensure the fulfilment of its occupational preventive objective. Our results might encourage other countries with similar practices to assess them in order to assure their fitness for purpose.
Pese a la ausencia de evidencia a favor, la realización de exámenes de salud rutinarios a los trabajadores, sobre todo previos/iniciales y periódicos, es una práctica extendida en muchos países y conlleva una asignación importante de recursos. En España se realizan dentro de un sistema de vigilancia de la salud laboral teóricamente específico. Nuestro objetivo fue determinar su utilidad preventiva ocupacional desde la perspectiva de los profesionales sanitarios de salud laboral
MétodosEstudio transversal. Encuesta en línea dirigida a profesionales sanitarios miembros de la Sociedad Catalana de Seguridad y Medicina del Trabajo (n=539) en 2011. Análisis univariado y bivariado de prevalencia y prevalencia de diferencias de las respuestas.
ResultadosTasa de respuesta 53% (n=285). Según más del 70% de los participantes, el sistema de vigilancia de la salud no es costo-efectivo, no cumple el objetivo de detección precoz de daños a la salud relacionados con el trabajo, y no contribuye a mejorar el sistema de prevención de riesgos laborales. También se identificaron deficiencias en la especificidad y base científica de los exámenes, en la calidad de la vigilancia colectiva y en la derivación a mutua de casos sospechosos de patología laboral para diagnóstico y tratamiento. El análisis bivariado mostró una opinión significativamente más negativa para varios ítems entre los médicos (versus enfermeras) y los profesionales de servicios de prevención ajenos (versus propios).
ConclusionesEste estudio plantea serias preocupaciones acerca de cómo se realizan los exámenes de salud dentro del sistema de vigilancia de la salud de nuestros trabajadores, que debe ser revisado para asegurar el cumplimiento de su objetivo preventivo laboral. Países con prácticas preventivas similares podrían verse alentados por nuestros resultados para revisarlas.
Health examinations for workers are extensively performed in many countries, either in the context of fitness for work examinations -mainly at pre employment/pre placement-, as part of health surveillance -mostly periodic and often linked to fitness for work certification-, or as general health checks. In 2010, out of a salaried working population of 2.7 million,1 one million workers’ health examinations were performed in the context of health surveillance in Catalonia, involving approximate direct costs of 49–59 million Euros assuming a cost of 50–60€ per health examination charged to employers.2 Indirect costs are difficult to calculate but they include lost working time, adjustments to maintain production schedules, travel time and expenses, and costs of re-testing (mostly in primary care) to rule out false positives. As any form of screening, this practice is not free of unwanted side-effects, like undue anxiety associated with false positives, re-testing, over-diagnosis and medicalization.3,4
According to the International Labour Office, “the central purpose of worker's health surveillance is the primary prevention of occupational and work-related diseases and injuries, and health examinations play a very important role, not only in primary, but also in secondary prevention, through early detection. Medical examinations and tests, however, should not be carried out as a perfunctory routine and due consideration should be given to their value and relevance”.5
Indeed, the preventive usefulness of indiscriminate health examinations is currently highly questioned, both for general population and for working population. The best available evidence shows that general health checks are unlikely to be beneficial for general population, and therefore its use is not supported.6,7 Within the occupational setting, a Cochrane review8 found that there is very low quality evidence that pre-employment examinations that are specific to certain jobs or health problems could reduce occupational disease, injury, or sickness absence, thus recommended restricting pre-employment examinations to job-specific examinations, and warned about the potential harms of rejecting job applicants. Less is published about the occupational preventive usefulness of routine workers’ periodic medical examinations.
In many European countries it is an obligation of all employers to provide occupational health coverage for their employees. The main Spanish health and safety law,9 a transcription of European Framework Directive 89/391/EEC,10 requires companies to offer appropriate health surveillance to their employees, and states that health examinations should be specific and a key instrument for prevention. These examinations are performed by occupational health professionals within prevention services. Companies can either create their own prevention service (internal prevention service) or contract the services from a private company (external prevention service). Prevention services have to interact with the two parallel, publicly financed, healthcare delivery systems in Spain: the National Health System, for non work-related issues, and employers’ mutual insurance companies – that privately manage public funds – for work accidents and occupational diseases.
Given the importance of the issue and the scarcity of publications we decided to undertake this study with a twofold objective: (1) to ascertain the occupational preventive usefulness of medical examinations for workers in our country from the opinion of occupational health professionals, whilst searching for any potential differences by their personal or professional characteristics; and (2) to identify areas for improvement of health surveillance within prevention services.
MethodsDesign and study populationCross sectional design. Taking into account the objectives of the study and the scientific and legal aspects that would subsequently be used to analyse the responses, a self-administered questionnaire was designed, and refined after pilot-testing. Gold Plan SurveyMonkey software was used to develop the on-line version.
Apart from personal and professional data, it included a first section with 10 opinion questions about the overall situation of health examinations and workers’ health surveillance in Catalonia, and a second section with 57 questions on actual practice of health surveillance addressed to a subset of the participants, those who performed health examinations in prevention services. The results of the latter are currently being analysed separately. This report analyses the answers to the first section of the questionnaire.
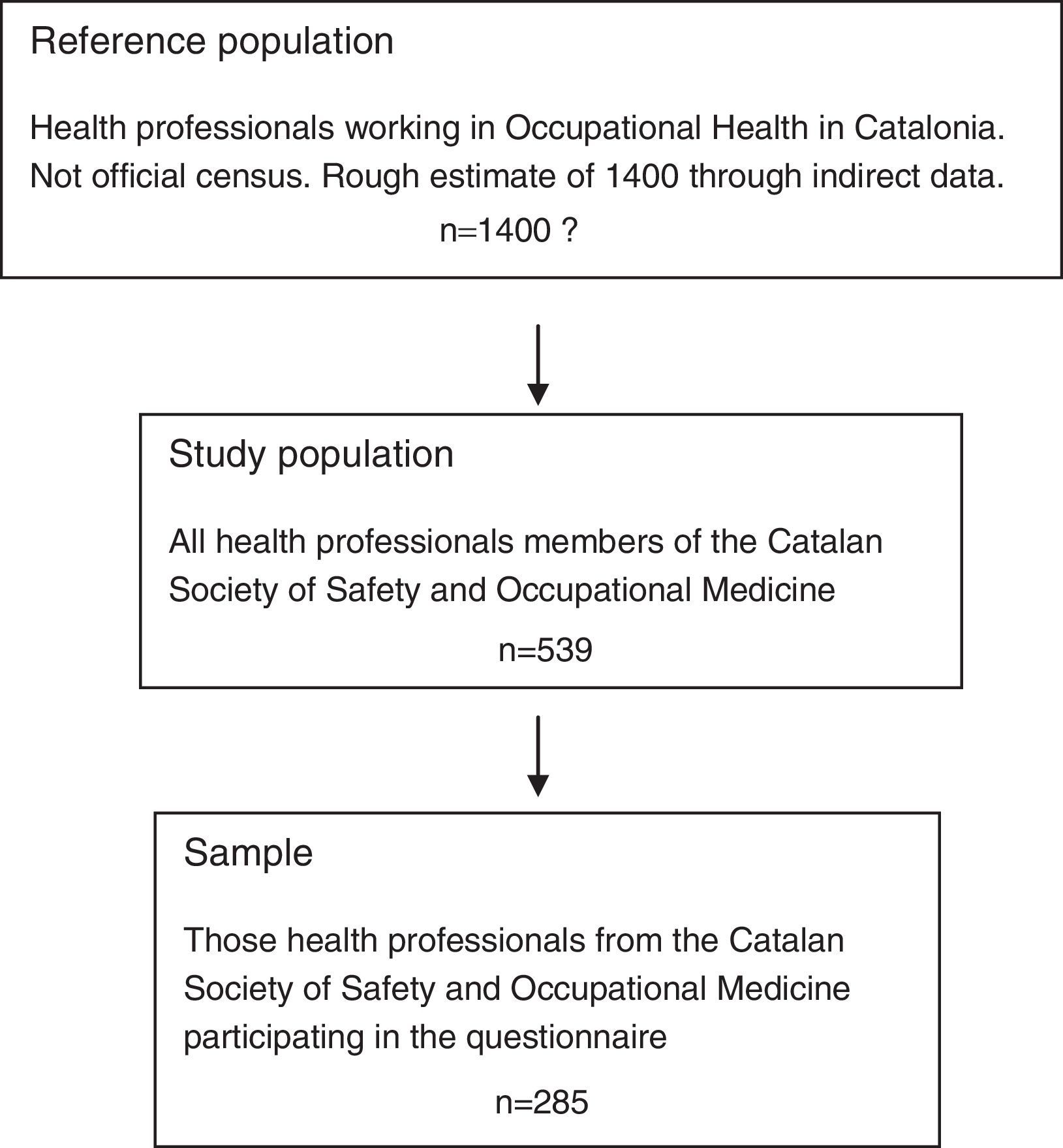
The study population consisted of all health professionals in the Catalan Society of Safety and Occupational Medicine since there is not an official census of health professionals working in Occupational Health in Catalonia (reference population). Our sample consisted of those professionals responding to the questionnaire (Fig. 1). Indirect data were used to estimate the size of the reference population.2 Confidence level absolute values of the estimated ratios were calculated under the assumption of maximum uncertainty (p=q=0.5) and 95% confidence.11
VariablesParticipants’ characteristics (categories are shown in brackets). Age (years); sex (male/female); qualification (physician/nurse); field of activity (prevention service/other fields); type of prevention service if applicable (internal/external); and performance of health examinations by the professional (yes/no).
Areas explored. The questionnaire included questions on the specificity, evidence basis, efficiency, capacity for early diagnosis, and general preventive usefulness of health examinations. Further questions explored professionals’ perception of communication channels between prevention services and both employers’ mutual insurance companies and the National Health System, the degree of referral of suspected occupational and work related diseases by prevention services to mutual insurance companies, the quality of collective health surveillance, and the good use of the skills of occupational health professionals. Likert type scales with 4 or 5 categories plus one “I don’t know” option were used for the answers. Items of the questionnaire and answer options are available in Table I of the online Appendix of this article.
Data gatheringA postal and e-mail invitation to participate in an anonymous, online-only questionnaire was sent to all occupational health professionals in September 2011. Four e-mail reminders encouraged participation along the 6 week data-gathering period.
Data analysisThe distribution of frequencies of answers was calculated for each question. For the bivariate analysis, the questionnaire response categories were dichotomized, grouping the 2 negative options of each answer against all the rest (e.g. “poor or very poor”, “low or very low”). The prevalence of the negative options, the differences of prevalence, and their confidence intervals of 95% were calculated using SPSS 15.0 for Windows.
Ethical considerationsThe study was approved by the Catalan Society of Safety and Occupational Medicine. Their administrative staff sent all postal and e-mail correspondence where participants were informed of the objective of the study which was voluntary and anonymous. The researchers remained blind to the list of potential and actual participants to the survey throughout the whole process.
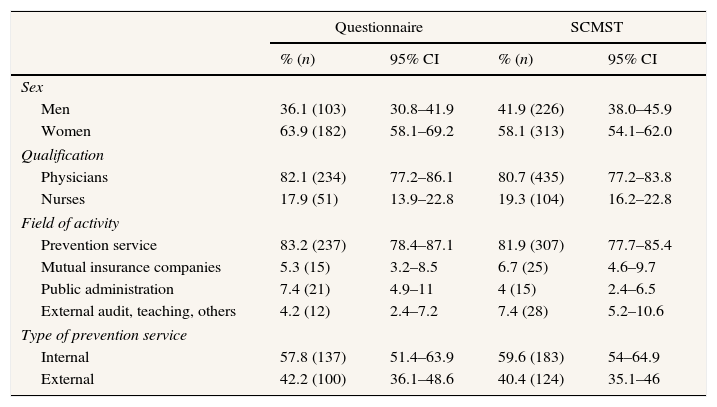
ResultsIn September 2011, the Catalan Society of Safety and Occupational Medicine had 539 health care professional members: 435 physicians and 104 nurses. A total of 321 professionals (59.6%) participated in the survey. Out of the 321 participants, 285 completed the opinion section of the questionnaire, yielding a response rate of 53% for completed questionnaires. The average age of our sample was 47.6 years (CI 46.6–48.6; range 27–69), 63.9% were female (n=182), and 82.1% were physicians (n=234). A total of 83.2% worked in prevention services (n=237), and 57.8% of them in internal prevention services (n=137). The distribution of this sample showed no statistically significant differences with the population of study for the characteristics described above (Table 1). Regarding the reference population, despite the lack of an official census, indirect data allow to estimate this number in roughly 1400. Assuming this estimation, physicians participating in our study would represent approximately 35% of the total physicians working in Occupational Health in Catalonia, while nurses representativeness would be of 7%. The sample would have confidence level absolute precision values of ±5.18% in relation to the reference population, calculated given the number of participants and under the assumption of maximum uncertainty (p=q=0.5) and 95% confidence.
Distribution of respondents to the questionnaire (sample) and SCSMT members (study population).
| Questionnaire | SCMST | |||
|---|---|---|---|---|
| % (n) | 95% CI | % (n) | 95% CI | |
| Sex | ||||
| Men | 36.1 (103) | 30.8–41.9 | 41.9 (226) | 38.0–45.9 |
| Women | 63.9 (182) | 58.1–69.2 | 58.1 (313) | 54.1–62.0 |
| Qualification | ||||
| Physicians | 82.1 (234) | 77.2–86.1 | 80.7 (435) | 77.2–83.8 |
| Nurses | 17.9 (51) | 13.9–22.8 | 19.3 (104) | 16.2–22.8 |
| Field of activity | ||||
| Prevention service | 83.2 (237) | 78.4–87.1 | 81.9 (307) | 77.7–85.4 |
| Mutual insurance companies | 5.3 (15) | 3.2–8.5 | 6.7 (25) | 4.6–9.7 |
| Public administration | 7.4 (21) | 4.9–11 | 4 (15) | 2.4–6.5 |
| External audit, teaching, others | 4.2 (12) | 2.4–7.2 | 7.4 (28) | 5.2–10.6 |
| Type of prevention service | ||||
| Internal | 57.8 (137) | 51.4–63.9 | 59.6 (183) | 54–64.9 |
| External | 42.2 (100) | 36.1–48.6 | 40.4 (124) | 35.1–46 |
| Mean | Difference in means | 95% CI for the difference | ||
|---|---|---|---|---|
| Age | ||||
| Questionnaire | 47.63 | Inf | Sup | |
| SCSMT | 48.24 | 0.611 | −0.764 | 1.987 |
CI: Confidence Interval; SCSMT: Catalan Society of Safety and Occupational Medicine.
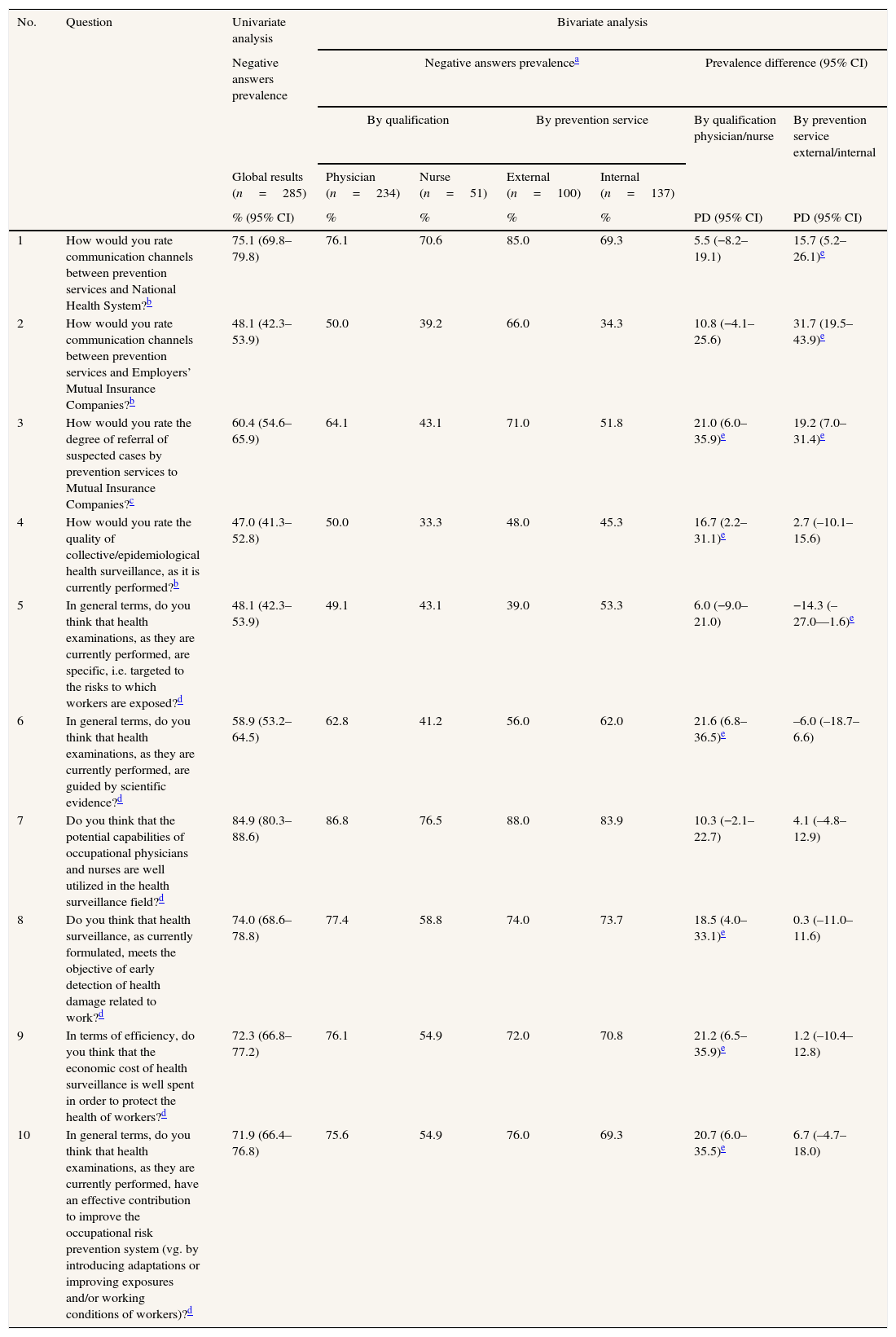
Table 2 shows the prevalence of negative answers which highlight potential areas for improvement in health surveillance and the way health examinations are performed.
Global results of negative answers prevalence (univariate analysis) and prevalence of negative answers and difference of prevalences by qualification and type of prevention services (bivariate analysis).
| No. | Question | Univariate analysis | Bivariate analysis | |||||
|---|---|---|---|---|---|---|---|---|
| Negative answers prevalence | Negative answers prevalencea | Prevalence difference (95% CI) | ||||||
| By qualification | By prevention service | By qualification physician/nurse | By prevention service external/internal | |||||
| Global results (n=285) | Physician (n=234) | Nurse (n=51) | External (n=100) | Internal (n=137) | ||||
| % (95% CI) | % | % | % | % | PD (95% CI) | PD (95% CI) | ||
| 1 | How would you rate communication channels between prevention services and National Health System?b | 75.1 (69.8–79.8) | 76.1 | 70.6 | 85.0 | 69.3 | 5.5 (−8.2–19.1) | 15.7 (5.2–26.1)e |
| 2 | How would you rate communication channels between prevention services and Employers’ Mutual Insurance Companies?b | 48.1 (42.3–53.9) | 50.0 | 39.2 | 66.0 | 34.3 | 10.8 (−4.1–25.6) | 31.7 (19.5–43.9)e |
| 3 | How would you rate the degree of referral of suspected cases by prevention services to Mutual Insurance Companies?c | 60.4 (54.6–65.9) | 64.1 | 43.1 | 71.0 | 51.8 | 21.0 (6.0–35.9)e | 19.2 (7.0–31.4)e |
| 4 | How would you rate the quality of collective/epidemiological health surveillance, as it is currently performed?b | 47.0 (41.3–52.8) | 50.0 | 33.3 | 48.0 | 45.3 | 16.7 (2.2–31.1)e | 2.7 (–10.1–15.6) |
| 5 | In general terms, do you think that health examinations, as they are currently performed, are specific, i.e. targeted to the risks to which workers are exposed?d | 48.1 (42.3–53.9) | 49.1 | 43.1 | 39.0 | 53.3 | 6.0 (−9.0–21.0) | −14.3 (–27.0––1.6)e |
| 6 | In general terms, do you think that health examinations, as they are currently performed, are guided by scientific evidence?d | 58.9 (53.2–64.5) | 62.8 | 41.2 | 56.0 | 62.0 | 21.6 (6.8–36.5)e | –6.0 (–18.7–6.6) |
| 7 | Do you think that the potential capabilities of occupational physicians and nurses are well utilized in the health surveillance field?d | 84.9 (80.3–88.6) | 86.8 | 76.5 | 88.0 | 83.9 | 10.3 (−2.1–22.7) | 4.1 (–4.8–12.9) |
| 8 | Do you think that health surveillance, as currently formulated, meets the objective of early detection of health damage related to work?d | 74.0 (68.6–78.8) | 77.4 | 58.8 | 74.0 | 73.7 | 18.5 (4.0–33.1)e | 0.3 (–11.0–11.6) |
| 9 | In terms of efficiency, do you think that the economic cost of health surveillance is well spent in order to protect the health of workers?d | 72.3 (66.8–77.2) | 76.1 | 54.9 | 72.0 | 70.8 | 21.2 (6.5–35.9)e | 1.2 (–10.4–12.8) |
| 10 | In general terms, do you think that health examinations, as they are currently performed, have an effective contribution to improve the occupational risk prevention system (vg. by introducing adaptations or improving exposures and/or working conditions of workers)?d | 71.9 (66.4–76.8) | 75.6 | 54.9 | 76.0 | 69.3 | 20.7 (6.0–35.5)e | 6.7 (–4.7–18.0) |
CI: Confidence Interval.
According to more than 70% of participants: the coordination of prevention services with the National Health Service is poor (75.1%); the economic cost of health surveillance is not well spent in order to protect the health of workers (72.3%); health surveillance fails in its goal of early detection of health damage related to work (74.0%); and doesn’t improve the occupational risk prevention system (71.9%) -i.e. by introducing adaptations or improving exposures and/or working conditions of workers-.
Roughly half of participants considered that referral of suspected cases (60.4%) and communication with mutual insurance companies is poor (48.1%), negatively rated the quality of collective health surveillance (47.0%), and pointed out that health examinations are not evidence-based (58.9%) or specific (48.1%) -i.e. targeted to the risks to which workers are exposed-.
The potential capabilities of occupational health professionals are underutilized in their roles in health surveillance according to 85% of participants.
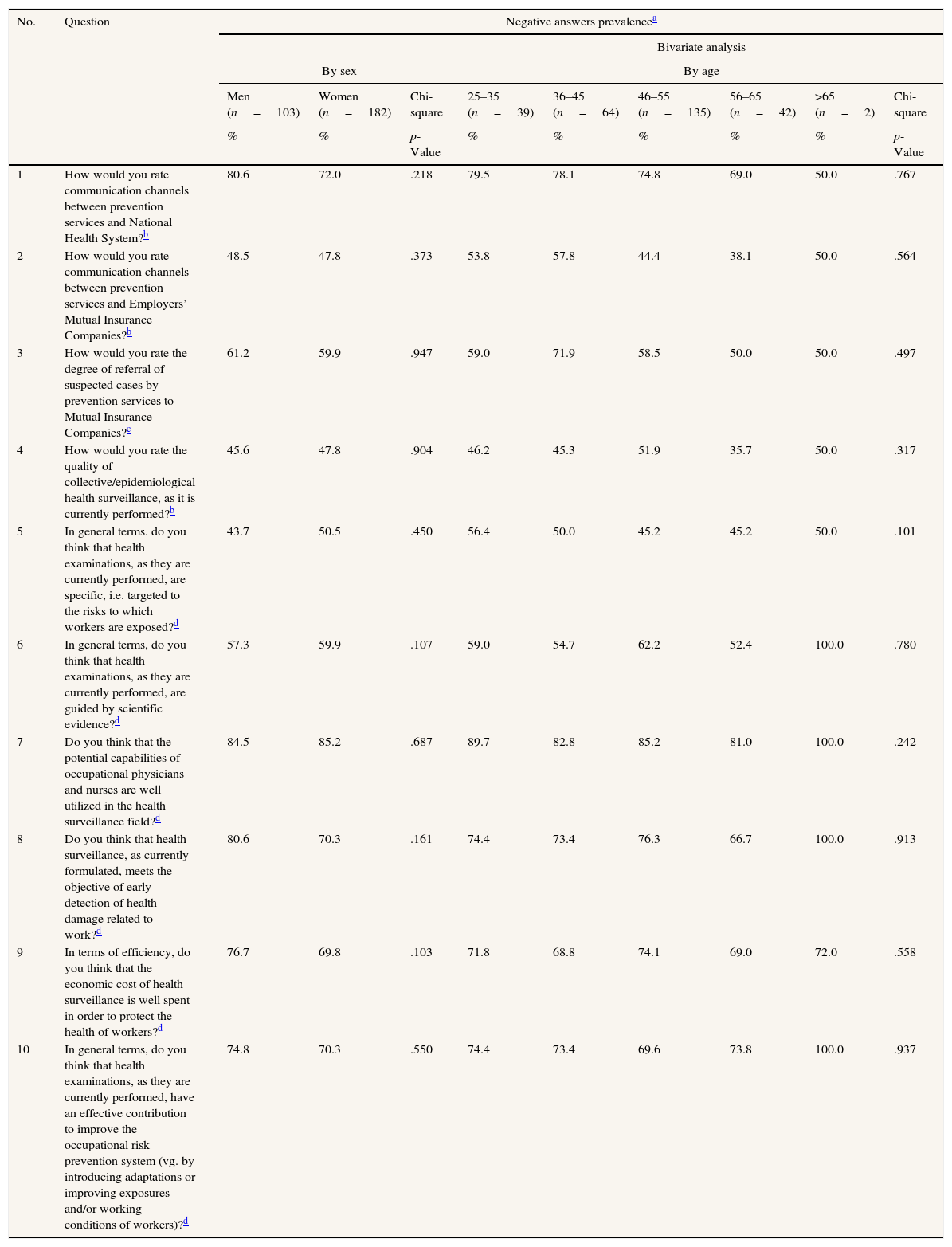
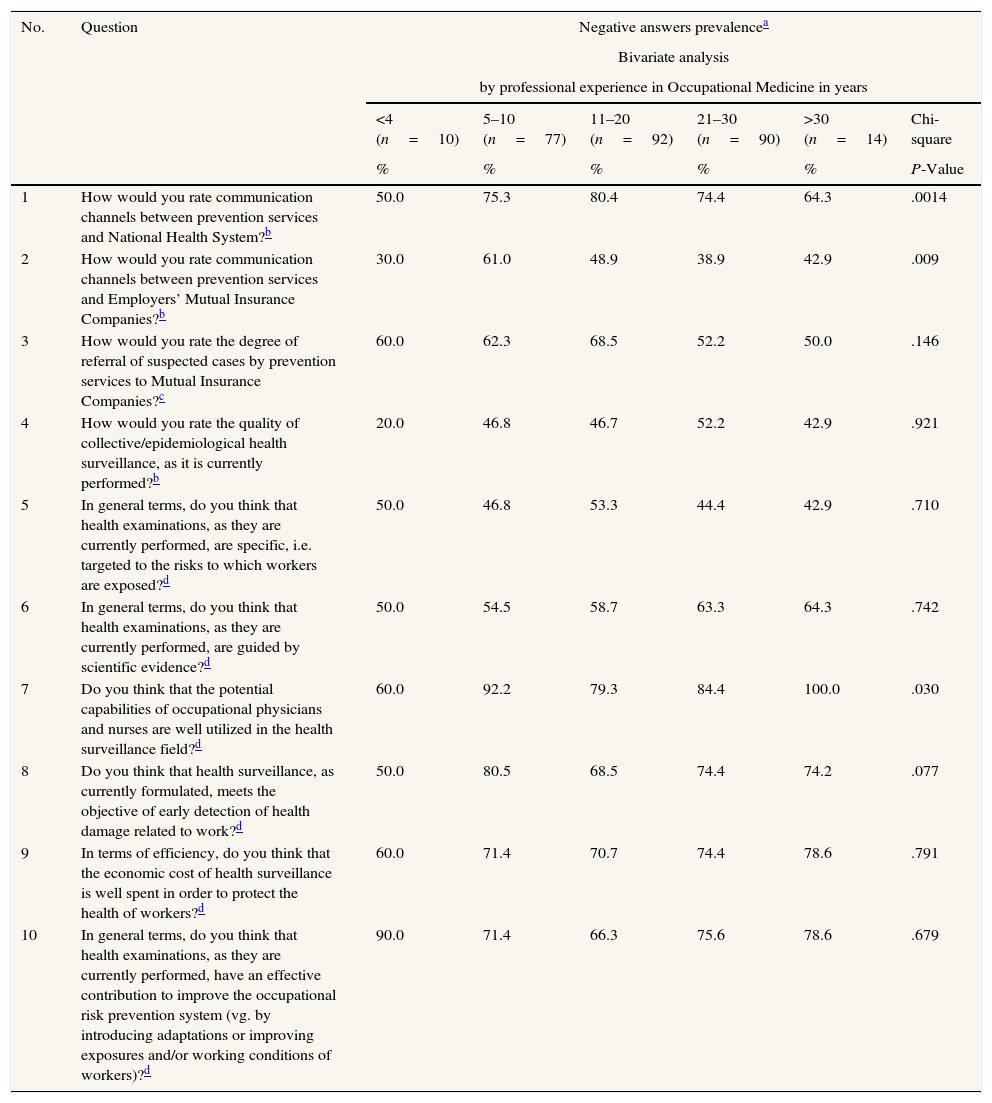
Bivariate analysis didn’t identify statistically significant differences by age, sex (see Table 3), field of activity or between professionals who performed health examinations -presumably with a deeper knowledge- and those who didn’t. Table 4 shows that some statistically significant differences were found for years of professional experience for items 1, 2 and 7. However these differences might be due to the small “n” number in some of the categories.
Bivariate analysis (Chi-square) of negative answers prevalence and p-values by sex and age.
| No. | Question | Negative answers prevalencea | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bivariate analysis | ||||||||||
| By sex | By age | |||||||||
| Men (n=103) | Women (n=182) | Chi-square | 25–35 (n=39) | 36–45 (n=64) | 46–55 (n=135) | 56–65 (n=42) | >65 (n=2) | Chi-square | ||
| % | % | p-Value | % | % | % | % | % | p-Value | ||
| 1 | How would you rate communication channels between prevention services and National Health System?b | 80.6 | 72.0 | .218 | 79.5 | 78.1 | 74.8 | 69.0 | 50.0 | .767 |
| 2 | How would you rate communication channels between prevention services and Employers’ Mutual Insurance Companies?b | 48.5 | 47.8 | .373 | 53.8 | 57.8 | 44.4 | 38.1 | 50.0 | .564 |
| 3 | How would you rate the degree of referral of suspected cases by prevention services to Mutual Insurance Companies?c | 61.2 | 59.9 | .947 | 59.0 | 71.9 | 58.5 | 50.0 | 50.0 | .497 |
| 4 | How would you rate the quality of collective/epidemiological health surveillance, as it is currently performed?b | 45.6 | 47.8 | .904 | 46.2 | 45.3 | 51.9 | 35.7 | 50.0 | .317 |
| 5 | In general terms. do you think that health examinations, as they are currently performed, are specific, i.e. targeted to the risks to which workers are exposed?d | 43.7 | 50.5 | .450 | 56.4 | 50.0 | 45.2 | 45.2 | 50.0 | .101 |
| 6 | In general terms, do you think that health examinations, as they are currently performed, are guided by scientific evidence?d | 57.3 | 59.9 | .107 | 59.0 | 54.7 | 62.2 | 52.4 | 100.0 | .780 |
| 7 | Do you think that the potential capabilities of occupational physicians and nurses are well utilized in the health surveillance field?d | 84.5 | 85.2 | .687 | 89.7 | 82.8 | 85.2 | 81.0 | 100.0 | .242 |
| 8 | Do you think that health surveillance, as currently formulated, meets the objective of early detection of health damage related to work?d | 80.6 | 70.3 | .161 | 74.4 | 73.4 | 76.3 | 66.7 | 100.0 | .913 |
| 9 | In terms of efficiency, do you think that the economic cost of health surveillance is well spent in order to protect the health of workers?d | 76.7 | 69.8 | .103 | 71.8 | 68.8 | 74.1 | 69.0 | 72.0 | .558 |
| 10 | In general terms, do you think that health examinations, as they are currently performed, have an effective contribution to improve the occupational risk prevention system (vg. by introducing adaptations or improving exposures and/or working conditions of workers)?d | 74.8 | 70.3 | .550 | 74.4 | 73.4 | 69.6 | 73.8 | 100.0 | .937 |
Bivariate analysis (Chi-square) of negative answers prevalence and p-values by professional experience in Occupational Medicine in years.
| No. | Question | Negative answers prevalencea | |||||
|---|---|---|---|---|---|---|---|
| Bivariate analysis | |||||||
| by professional experience in Occupational Medicine in years | |||||||
| <4 (n=10) | 5–10 (n=77) | 11–20 (n=92) | 21–30 (n=90) | >30 (n=14) | Chi-square | ||
| % | % | % | % | % | P-Value | ||
| 1 | How would you rate communication channels between prevention services and National Health System?b | 50.0 | 75.3 | 80.4 | 74.4 | 64.3 | .0014 |
| 2 | How would you rate communication channels between prevention services and Employers’ Mutual Insurance Companies?b | 30.0 | 61.0 | 48.9 | 38.9 | 42.9 | .009 |
| 3 | How would you rate the degree of referral of suspected cases by prevention services to Mutual Insurance Companies?c | 60.0 | 62.3 | 68.5 | 52.2 | 50.0 | .146 |
| 4 | How would you rate the quality of collective/epidemiological health surveillance, as it is currently performed?b | 20.0 | 46.8 | 46.7 | 52.2 | 42.9 | .921 |
| 5 | In general terms, do you think that health examinations, as they are currently performed, are specific, i.e. targeted to the risks to which workers are exposed?d | 50.0 | 46.8 | 53.3 | 44.4 | 42.9 | .710 |
| 6 | In general terms, do you think that health examinations, as they are currently performed, are guided by scientific evidence?d | 50.0 | 54.5 | 58.7 | 63.3 | 64.3 | .742 |
| 7 | Do you think that the potential capabilities of occupational physicians and nurses are well utilized in the health surveillance field?d | 60.0 | 92.2 | 79.3 | 84.4 | 100.0 | .030 |
| 8 | Do you think that health surveillance, as currently formulated, meets the objective of early detection of health damage related to work?d | 50.0 | 80.5 | 68.5 | 74.4 | 74.2 | .077 |
| 9 | In terms of efficiency, do you think that the economic cost of health surveillance is well spent in order to protect the health of workers?d | 60.0 | 71.4 | 70.7 | 74.4 | 78.6 | .791 |
| 10 | In general terms, do you think that health examinations, as they are currently performed, have an effective contribution to improve the occupational risk prevention system (vg. by introducing adaptations or improving exposures and/or working conditions of workers)?d | 90.0 | 71.4 | 66.3 | 75.6 | 78.6 | .679 |
Statistically significant differences were found, however, by qualification and type of prevention service as shown in Table 2. In summary, professionals in external prevention services had a significantly more negative opinion about the referral of suspected cases and about the communication channels between prevention services and both employers’ mutual insurance companies and the National Health System. They showed a more positive opinion exclusively regarding specificity of health examinations. Physicians’ perception was significantly more negative than that of nurses’ regarding referral rates to mutual insurance companies, quality of collective surveillance, evidence basis, early detection, cost-effectiveness and overall preventive usefulness of health examinations.
DiscussionA high percentage of the occupational health care professionals participating in our study described health examinations as unspecific, inefficient, not evidence-based and not contributing to early diagnosis or effective prevention, which seriously questions the quality and preventive usefulness of health surveillance as it is currently performed.
A significantly more negative opinion was found for several items amongst physicians (versus nurses) and amongst professionals working in external prevention services (versus internal services). The more negative opinion of physicians could be explained by different knowledge areas and professional expectations in some cases. And the more negative opinion of professionals from external prevention services, might be explained by the fact that they are located away from the workplaces, their contact with workers is often reduced to medical examinations, and feedback on their decisions or recommendations is scarce, reducing health surveillance, in many cases, to the routine, automated performance of high numbers of health examinations. These health examinations are aimed at predominantly healthy individuals, and generally have a scarce occupational content. This might explain why 85% of participants felt that the highly trained Catalan occupational physicians and nurses are overqualified for the range of activities they currently perform.
A high proportion of professionals reported low referral rates of suspected cases to mutual insurance companies, whose responsibility is, precisely, the diagnosis, treatment and official reporting of occupational and work related diseases and injuries. One possible explanation might be that the professional independence of occupational physicians might have been jeopardized through organisational conditions and unwritten guidelines within the company (internal prevention services), or the influence of open market rules (external prevention services), given that the regulatory framework in Spain determines economic compensation and corporate responsibilities for companies in case of recognition of occupational injury or disease. It has to be noted that in occupational health there are interactions between many partners, sometimes with conflicting interests. And although the code of ethics of the International Commission of Occupational Health12 states in its basic principles that “occupational health professionals are experts who must enjoy full professional independence in the execution of their functions”, it cannot be guaranteed that this is always the case.13
Although motivational issues might have influenced participation in the study, we don’t have evidence to support this. Indeed, those who join a scientific society are likely to be more engaged and have a higher level of commitment with their profession and therefore their opinion might be more critical, but they are likely to have a higher insight too. On the other hand, the results from a 2007 survey to occupational health care professionals in Catalonia,14 suggest that the professional situation and working conditions of those who are not members of the Catalan Society of Safety and Occupational Medicine are frequently worse, and, presumably, their opinion would be too. Thus, in case of having incurred in a selection bias by the choice of our population, our study would probably underestimate the real situation in Catalonia.
The members of the Catalan Society of Safety and Occupational Medicine were chosen as the study population, conditioned by the fact that it was the only identifiable, and on the grounds that they are a representative group of physicians and nurses working in occupational health in Catalonia, given the lack of an official census. The lack of statistically significant differences for personal and professional characteristics between our sample and the Catalan Society of Safety and Occupational Medicine as a whole, together with the satisfactory response rate, points to the adequate representativeness of our sample, suggesting that our results truly reflect the opinion of the Society. We are confident that the results of our study validly describe the real situation in Catalonia, and, if we accept the rough estimate of 1400 professionals as reference population, our data would have external validity for Catalonia.
Moreover, our results are probably valid for Spain as a whole too, given that health and safety laws and the labour inspectorate are common, and companies and prevention services share similar practices and procedures, especially in the case of external prevention services, most of which are large nation-wide companies.
This is the first study of its kind carried out in Spain in a subject where literature is very scarce. In a Belgian survey an on-line questionnaire was sent to 510 occupational physicians15 which resulted in 222 complete replies. In an “open comment box” many complained of being constricted by a legal framework leading to excessive periodic examinations at the expense of other forms of prevention, and those physicians in favour of periodic examinations, reckoned that their content should be improved. A French qualitative study of occupational health doctors and workers16 also concluded that occupational health practice often falls into an institutional framework that prioritizes medical examinations over the improvement of environmental and organisational conditions, worker health protection and promotion of workplace adaptations when needed.
Despite the subjectivity of our data, we understand that occupational health professionals are very well placed to judge the current situation of health surveillance and health examinations. Our work gives visibility to a widespread negative opinion amongst these professionals, and the unequivocal nature of the results clearly deserves attention from Catalan and Spanish institutions with competencies in health and safety. If these views are confirmed by assessing the actual practice, changes should be introduced to improve health surveillance in our country. These changes might include a regulatory reform, but more urgently, multilateral agreements among labour and health authorities, social partners including employers’ and employees’ representatives, and, regarding Occupational Medicine, representatives from academia and the profession.
In conclusion, the situation described by occupational physicians and nurses raises serious concerns about the efficiency and preventive usefulness of workers’ health examinations performed in a theoretical job-specific health surveillance system in Catalonia. Potential areas for improvement have been identified regarding issues such as coordination between prevention services and the health care system, early detection of health damage related to work and referral of suspected cases for diagnosis and treatment, as well as the specificity and scientific basis for health examinations. Occupational health professionals alongside health and safety stakeholders should promote the development of a truly efficient, evidence based health surveillance that fulfils its preventive objective, allocating resources accordingly. Other countries with similar practices might be encouraged by our results to assess them in order to assure their fitness for purpose.
Health examinations for workers are extensively performed in many countries, which has implications on allocation of limited resources. There are few studies on the quality, effectiveness and occupational preventive usefulness of routine workers’ medical examinations.
What does this study add to the literature?Our study, the first of its kind in Spain, seriously questions the quality and occupational preventive usefulness of workers’ health examinations performed in a theoretical job-specific health surveillance system in Catalonia.
Professionals, health and safety stakeholders and policy makers at national, regional and company level should take actions to assess it and improve it accordingly. Further research is needed to develop guidelines for a truly efficient, evidence based health surveillance that fulfils its preventive objective.
Clara Bermúdez-Tamayo.
Author's contributionsM.C. Rodríguez-Jareño was the main author, conceived the idea for the study and designed the first draft of the questionnaire. She was the main contributor to the analysis and interpretation of results and writing of the paper. J. de Montserrat and E. Molinero contributed with improvements in the design of the study, the design and content of the pilot questionnaire and its final version, and helped to analyse the information and interpreted and gave possible explanations to the results. A. Vallès helped with the design of the study and of the questionnaire and supervised methodological aspects, especially in relation to statistical analysis, together with E. Molinero. M. Aymerich was in charge of the general supervision of the study, and contributed to methodological aspects and analysis of the results. All authors contributed to the analysis and interpretation of results and the writing of the paper. All authors approved the final version of the manuscript.
FundingThis paper has been partially funded by a Fundación Prevent grant R+D in Occupational Risk Prevention.
Conflicts of interestNone.
We would like to thank the professionals of the Catalan Society of Safety and Occupational Medicine who have participated in this survey, and the board of the Society for their support.