To estimate the prevalence of hepatitis B virus (HBV) infection and vaccine-induced immunity in the region of Madrid, and to analyze their evolution over time.
MethodsAn observational, analytical, cross-sectional study was carried out in the population aged 16–80 years between 2008 and 2009. This was the last of four seroprevalence surveys in the region of Madrid. The prevalence of HBV infection and vaccine-induced immunity was estimated using multivariate logistic models and were compared with the prevalences in the 1989, 1993 and 1999 surveys.
ResultsIn the population aged 16–80 years, the prevalence of HBV infection was 11.0% (95% CI: 9.8–12.3) and that of chronic infection was 0.7% (95% CI: 0.5–1.1). The prevalence of vaccine-induced immunity in the population aged 16–20 years was 73.0% (95% CI: 70.0–76.0). Compared with previous surveys, there was a decrease in the prevalence of HBV infection.
ConclusionsBased on the prevalence of chronic infection (<1%), Madrid is a region with low HBV endemicity. Preventive strategies against HBV should especially target the immigrant population.
Estimar la prevalencia de infección por hepatitis B(HB) e inmunidad vacunal en la Comunidad de Madrid y analizar su evolución en el tiempo.
MétodosEstudio observacional analítico transversal en población de 16-80 años, en 2008-2009. Ésta es la última de cuatro encuestas de seroprevalencia. La prevalencia de infección por HB e inmunidad vacunal fue estimada usando modelos logísticos multivariantes y se compararon con las encuestas de 1989, 1993 y 1999.
ResultadosEn población de 16-80 años, la prevalencia de infección por HB fue 11,0% (IC-95%:9,8-12,3) y 0,7% (IC-95%:0,5-1,1) de infección crónica. La prevalencia de inmunidad vacunal en población de 16-20 años fue 73,0% (IC-95%:70,0-76,0). En comparación con anteriores encuestas la prevalencia de infección disminuyó.
ConclusionesMadrid es una región de baja endemicidad de HB, de acuerdo a la prevalencia de infección crónica (<1%). Las estrategias de prevención de la HB deben dirigirse especialmente a la población inmigrante.
Europe is a low to intermediate endemicity region for Hepatitis B (HB).1 The Spanish Seroprevalence Survey, carried out in 1996, reported prevalence rates for HB virus exposure and chronic infection of 4.5% and 0.8%, respectively, for the population aged 2–39 years.2
The Region of Madrid began vaccinating risk groups in the 1980s. In 1994 the HB vaccine was included in the vaccination schedule for infants (0–1–6 months). In 1996, a mixed vaccination programme was established that included vaccination at 11 years of age (discontinued in 2005) and vaccination for infants.
In the region of Madrid, seroprevalence surveys are conducted as part of the Epidemiological Surveillance Network3 since 1988. The aim of our study was to estimate the prevalence of HB infection and vaccine-induced immunity in the region of Madrid, and to analyze its evolution over time.
MethodsThis is an observational, analytical, cross-sectional study on the residents or the region of Madrid aged 16–80 years that attended blood extraction centres between January and June 2008 and between October and December 2009. The sampling plan was bi-stage, cluster (by socioeconomic class) and stratified (by proportion of immigrants) design, which resulted in the selection of 78 basic areas of health that represents the 247 of Region of Madrid. Immigrant population was sample at a higher frequency than the rest to provide more precise estimates in this group. Similar sampling has been used in other seroprevalence surveys.4
Patients with diseases or conditions that could interfere with the immune response were excluded. Socio-demographic factors, history of hepatitis, vaccination status and exposure to bloodborne risk were collected by trained interviewers. Eligible individuals gave informed consent to be part of this study, and the study was approved by the ethical committee of the Ramón y Cajal University Hospital.
HB profiles analyzed were as follows: past resolved infection (positive anti-HBc and positive anti-HBs); chronic HB infection (positive anti-HBc, negative anti-HBs and positive HBsAg); isolated infection (only positive anti-HBc) and finally, vaccine-induced immunity (positive anti-HBs and negative anti-HBc).
Anti-HBc antibodies were detected by competitive enzyme-linked immunosorbent assay (ELISA) (sensitivity: 99.0%, specificity between 99.6% and 99.7%) and anti-HBs antibodies were detected using one-step sandwich ELISA (Enzygnost® Siemens-GmbH, Germany) (sensitivity: 99.1%, specificity: 99.8%). Anti-HBc positive and anti-HBs negative samples were then processed to detect HBsAg using two-step ELISA (Enzygnost® Siemens-GmbH, Germany) (sensitivity: 100%, specificity: 99.8%) and HBsAg positivity was confirmed by repeating the test.
Prevalence for the four immune profiles was estimated overall and according to sociodemographic characteristics. Possible risk factors for HB infection (positive anti-HBc) and chronic HB infection such as age, sex, country of origin, education level and socioeconomic class were analyzed using univariate and multivariate logistic regression models. Prevalence estimations and regressions models were weighted to account for oversampling immigrant population.
Prevalence data from previous surveys (1988, 1993 and 1999) were used to study the HB infection evolution over time. The sampling method used in past surveys was the same as the one used in the present one.5,6 A multivariate logistic regression model adjusted for sex and age was used to compare prevalence in this survey with that in the 1999 survey.
ResultsA total of 3695 subjects participated in the study, for a response rate of 69.4%. The response rate was higher among women (73.0%), and among 40 years old or younger subjects (72.6%). In 9 cases, blood samples were not suitable.
Prevalence of HB infection in the population aged 16–80 years was 11.0% (95% confidence interval (CI): 9.8–12.3). Immigrants with HB infection were from Latin America (41.1%), Africa (29.2%), Eastern Europe (22.3%), Southeast Asia (5.6%), the Middle East (1.3%) and Western Europe (0.6%).
Of the subjects with HB infection, 80.0% (95% CI: 74.9–84.3) had past resolved infection (anti-HBc positive and anti-HBs positive), 6.3% (95% CI: 4.1–9.4) were chronically infected, and 13.7% (95% CI: 10.1–18.4) had isolated anti-HBc.
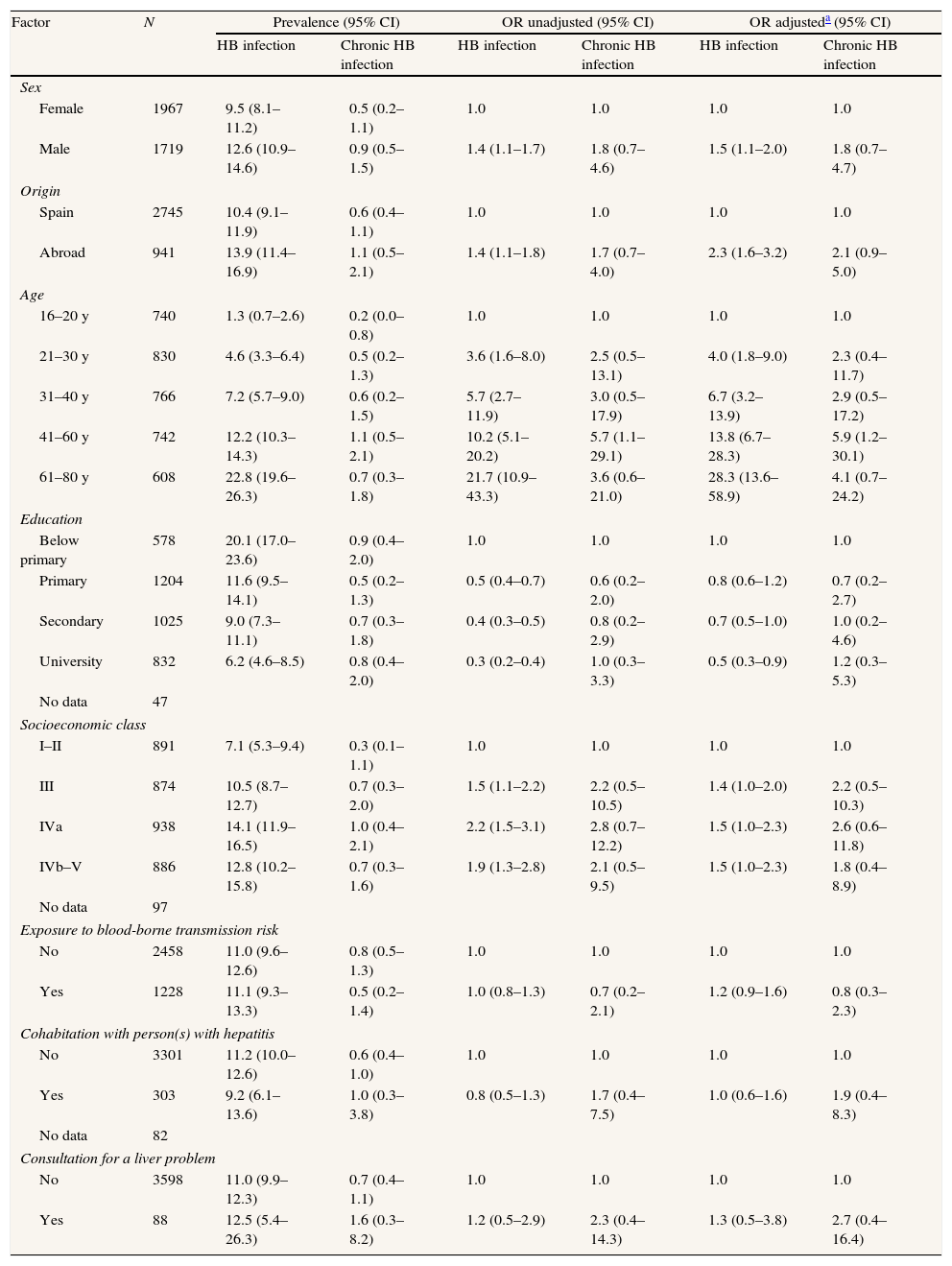
Chronic HB prevalence in the population aged 16–80 years was 0.7% (95% CI: 0.5–1.1). The proportion of carriers who reported a history of HBV was 46.4% (95% CI: 24.4–70.0). Prevalence and OR by socio-demographic factors are presented in Table 1.
Prevalence of HB Infection and possible risk factors. Fourth Seroprevalence Survey of the region of Madrid, 2008–2009.
| Factor | N | Prevalence (95% CI) | OR unadjusted (95% CI) | OR adjusteda (95% CI) | |||
| HB infection | Chronic HB infection | HB infection | Chronic HB infection | HB infection | Chronic HB infection | ||
| Sex | |||||||
| Female | 1967 | 9.5 (8.1–11.2) | 0.5 (0.2–1.1) | 1.0 | 1.0 | 1.0 | 1.0 |
| Male | 1719 | 12.6 (10.9–14.6) | 0.9 (0.5–1.5) | 1.4 (1.1–1.7) | 1.8 (0.7–4.6) | 1.5 (1.1–2.0) | 1.8 (0.7–4.7) |
| Origin | |||||||
| Spain | 2745 | 10.4 (9.1–11.9) | 0.6 (0.4–1.1) | 1.0 | 1.0 | 1.0 | 1.0 |
| Abroad | 941 | 13.9 (11.4–16.9) | 1.1 (0.5–2.1) | 1.4 (1.1–1.8) | 1.7 (0.7–4.0) | 2.3 (1.6–3.2) | 2.1 (0.9–5.0) |
| Age | |||||||
| 16–20 y | 740 | 1.3 (0.7–2.6) | 0.2 (0.0–0.8) | 1.0 | 1.0 | 1.0 | 1.0 |
| 21–30 y | 830 | 4.6 (3.3–6.4) | 0.5 (0.2–1.3) | 3.6 (1.6–8.0) | 2.5 (0.5–13.1) | 4.0 (1.8–9.0) | 2.3 (0.4–11.7) |
| 31–40 y | 766 | 7.2 (5.7–9.0) | 0.6 (0.2–1.5) | 5.7 (2.7–11.9) | 3.0 (0.5–17.9) | 6.7 (3.2–13.9) | 2.9 (0.5–17.2) |
| 41–60 y | 742 | 12.2 (10.3–14.3) | 1.1 (0.5–2.1) | 10.2 (5.1–20.2) | 5.7 (1.1–29.1) | 13.8 (6.7–28.3) | 5.9 (1.2–30.1) |
| 61–80 y | 608 | 22.8 (19.6–26.3) | 0.7 (0.3–1.8) | 21.7 (10.9–43.3) | 3.6 (0.6–21.0) | 28.3 (13.6–58.9) | 4.1 (0.7–24.2) |
| Education | |||||||
| Below primary | 578 | 20.1 (17.0–23.6) | 0.9 (0.4–2.0) | 1.0 | 1.0 | 1.0 | 1.0 |
| Primary | 1204 | 11.6 (9.5–14.1) | 0.5 (0.2–1.3) | 0.5 (0.4–0.7) | 0.6 (0.2–2.0) | 0.8 (0.6–1.2) | 0.7 (0.2–2.7) |
| Secondary | 1025 | 9.0 (7.3–11.1) | 0.7 (0.3–1.8) | 0.4 (0.3–0.5) | 0.8 (0.2–2.9) | 0.7 (0.5–1.0) | 1.0 (0.2–4.6) |
| University | 832 | 6.2 (4.6–8.5) | 0.8 (0.4–2.0) | 0.3 (0.2–0.4) | 1.0 (0.3–3.3) | 0.5 (0.3–0.9) | 1.2 (0.3–5.3) |
| No data | 47 | ||||||
| Socioeconomic class | |||||||
| I–II | 891 | 7.1 (5.3–9.4) | 0.3 (0.1–1.1) | 1.0 | 1.0 | 1.0 | 1.0 |
| III | 874 | 10.5 (8.7–12.7) | 0.7 (0.3–2.0) | 1.5 (1.1–2.2) | 2.2 (0.5–10.5) | 1.4 (1.0–2.0) | 2.2 (0.5–10.3) |
| IVa | 938 | 14.1 (11.9–16.5) | 1.0 (0.4–2.1) | 2.2 (1.5–3.1) | 2.8 (0.7–12.2) | 1.5 (1.0–2.3) | 2.6 (0.6–11.8) |
| IVb–V | 886 | 12.8 (10.2–15.8) | 0.7 (0.3–1.6) | 1.9 (1.3–2.8) | 2.1 (0.5–9.5) | 1.5 (1.0–2.3) | 1.8 (0.4–8.9) |
| No data | 97 | ||||||
| Exposure to blood-borne transmission risk | |||||||
| No | 2458 | 11.0 (9.6–12.6) | 0.8 (0.5–1.3) | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1228 | 11.1 (9.3–13.3) | 0.5 (0.2–1.4) | 1.0 (0.8–1.3) | 0.7 (0.2–2.1) | 1.2 (0.9–1.6) | 0.8 (0.3–2.3) |
| Cohabitation with person(s) with hepatitis | |||||||
| No | 3301 | 11.2 (10.0–12.6) | 0.6 (0.4–1.0) | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 303 | 9.2 (6.1–13.6) | 1.0 (0.3–3.8) | 0.8 (0.5–1.3) | 1.7 (0.4–7.5) | 1.0 (0.6–1.6) | 1.9 (0.4–8.3) |
| No data | 82 | ||||||
| Consultation for a liver problem | |||||||
| No | 3598 | 11.0 (9.9–12.3) | 0.7 (0.4–1.1) | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 88 | 12.5 (5.4–26.3) | 1.6 (0.3–8.2) | 1.2 (0.5–2.9) | 2.3 (0.4–14.3) | 1.3 (0.5–3.8) | 2.7 (0.4–16.4) |
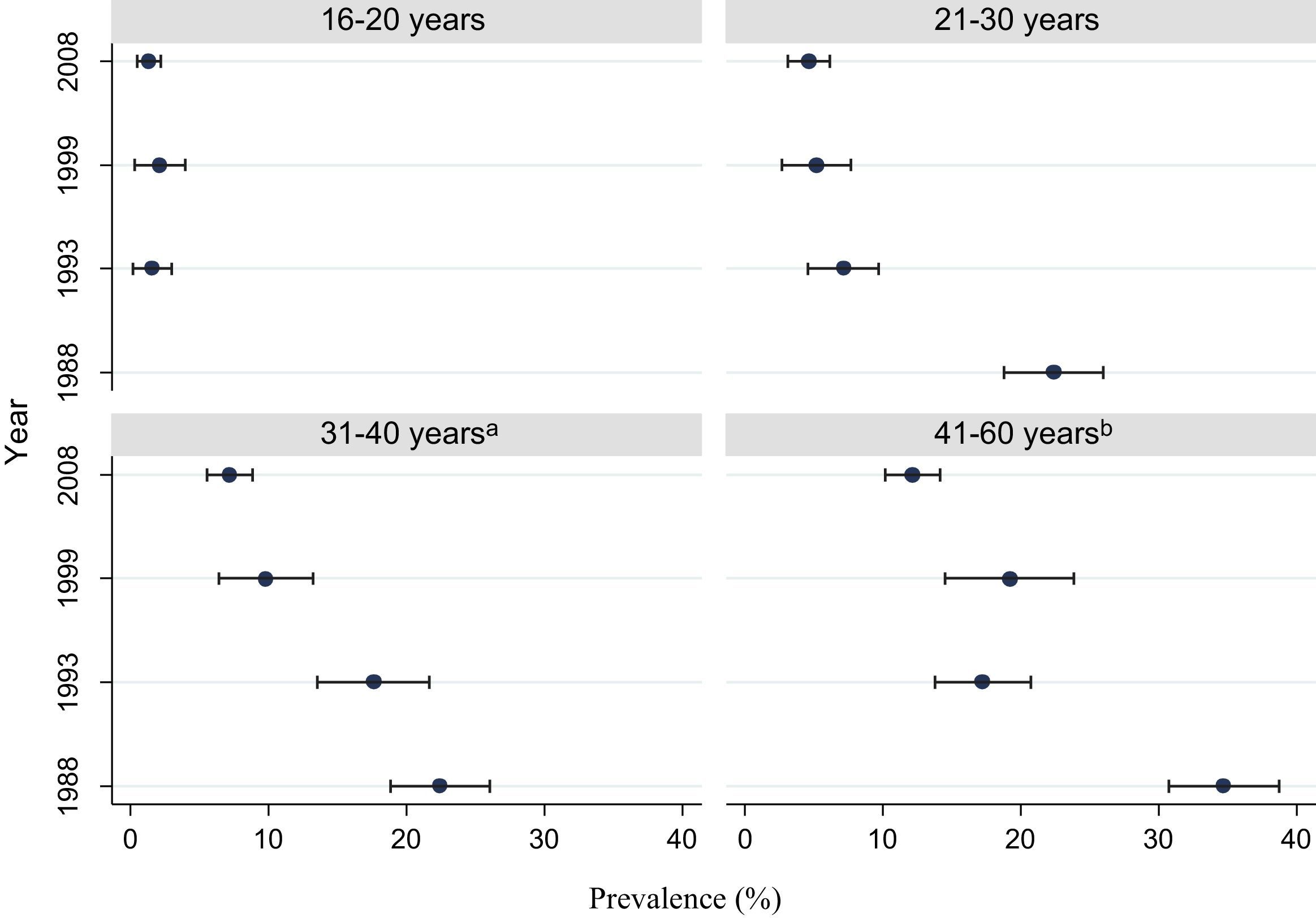
Fig. 1 shows the HB prevalence for all the seroprevalence surveys. A decreasing trend in prevalence of HB infection in 2008 compared with 1999 is observed (OR: 0.7; 95% CI: 0.5–0.9), especially in population between 41 and 60 years of age (OR: 0.6; 95% CI: 0.4–0.8). No significant differences were detected in relation to previous surveys, although estimated prevalence rates for the groups aged 16–20 years and 21–30 years were lower than that in the 1999 survey.
The prevalence of vaccine-induced immunity to HBV in the population aged 16–80 years was 26.3% (95% CI: 24.7–28.0). Prevalence for the group aged 16–20 years, consisting of cohorts recommended for vaccination at 11 years of age, was 73.0% (95% CI: 70.0–76.0). This figure was significantly lower for the immigrant population compared to the Spanish-born population (OR: 0.2; 95% CI: 0.2–0.4) and for men compared to women (OR: 0.6; 95% CI: 0.4–0.8).
DiscussionHB prevalence in the population aged 16–80 years in the region of Madrid is 11.0%. Prevalence has decreased compared to previous surveys, possibly due to the effectiveness of control measures for at-risk groups (safe sex practices, use of individual syringes, vaccination).
In this study, seroprevalence of infection is 2.5 times higher in people coming from immigrant than in native population. These data are consistent with the ones reported in other areas of the region.1,6 It is advisable to consider targeting disease prevention programmes in immigrant populations coming from high-endemicity regions as a cost effective measure.1,7,8
Chronic HB infection prevalence in the region of Madrid is low (<2%) and is below both the 1996 rate reported for Spain overall and the rates reported for other regions of Spain.2,9–12 Since chronic HB infection prevalence remains below 1% even considering that the population aged under 16 years is excluded from the analysis, Spain can be classified as a low-endemicity country.
Immunization is another factor influencing the HB prevalence profile for the region of Madrid. HB vaccination at 11 years of age was introduced in 1996 with a coverage of vaccination at ranged from 59.7% to 68.8%.13 However, this coverage figure is probably underestimated, given that vaccine-induced immunity prevalence for this group is 73.0% and due to loss of the ability to detect antibodies identified in individuals who retain good immune response.14 Significant reductions in infection can be expected in the coming years as the routine immunization target cohorts reach the age of highest transmission risk.
Although the main reason for non-participation in the study was lack of interest or time (78%), a healthy volunteer bias may be underestimating the prevalence of the disease.
The lower vaccine-induced immunity and higher prevalence of infection in the immigrant population make a priority to focus the HB preventive strategies to these high risk groups.
According to the last Spanish Seroprevalence Survey, the prevalence for Hepatitis B exposure and chronic infection was 4.5% and 0.8%, respectively.
What does this study add to the literature?In the Region of Madrid, Hepatitis B prevalence has shown a decreasing trend in the last 20 years and vaccine-induced immunity is lower in the immigrant population.
Implication for health policy/practice/research/medical education:In order to reduce the prevalence of Hepatitis B in the Region of Madrid, understanding of risk factors associated is mandatory.
This study was funded in part by the pharmaceutical company Gileas, which has provided the financial resources needed for the detection of the serological markers.
Authors contributionA brief description of the role and collaboration of each author are listed below: AM Pedraza conducted the statistical analysis and drafted the report. L García-Comas and M Ordobás-Gavín conceived and designed the study and oversaw the data management. JC-Sanz Moreno and B-Ramos Blázquez performed the laboratory analysis. Astray Mochales provided support to the bibliographic review. All authors interpreted the data and reviewed and approved the final version of the report.Editor in charge Pere Godoy.
Conflict of interestThe authors declare that they do not have a conflict of interest regarding the publication of this manuscript.