To analyse changes in health professionals’ and immigrant users’ perceptions of the quality of care provided to the immigrant population during the crisis.
MethodsA qualitative descriptive-interpretative and exploratory study was conducted in two areas of Catalonia. Semi-structured individual interviews were used with a theoretical sample of medical (n=24) and administrative (n=10) professionals in primary care (PC) and secondary care (SC), and immigrant users (n=20). Thematic analysis was conducted and the results were triangulated.
ResultsProblems related to technical and interpersonal quality emerged from the discourse of both professionals and immigrants. These problems were attributed to cutbacks during the economic crisis. Regarding technical quality, respondents reported an increase in erroneous or non-specific diagnoses, inappropriate use of diagnostic tests and non-specific treatments, due to reduction in consultation times as a result of cuts in human resources. With regard to interpersonal quality, professionals reported less empathy, and users also reported worse communication, due to changes in professionals’ working conditions and users’ attitudes. Finally, a reduction in the resolution capacity of the health services emerged: professionals described unnecessary repeated PC visits and limited responses in SC, while young immigrants reported an insufficient response to their health problems.
ConclusionThe results indicate a deterioration in perceived technical and interpersonal quality during the economic crisis, due to cutbacks mainly in human resources. These changes affect the whole population, but especially immigrants.
Analizar los cambios en la calidad percibida de la atención a la población inmigrante durante la crisis económica, desde la perspectiva de profesionales e inmigrantes.
MétodosEstudio cualitativo descriptivo-interpretativo y exploratorio en dos áreas de Cataluña, mediante entrevistas individuales semiestructuradas a una muestra teórica de médico/as (n=24) y administrativas (n=10) de atención primaria (AP) y secundaria (AS), e inmigrantes (n=20). Se realizó un análisis temático de contenido y se triangularon los resultados.
ResultadosDel discurso de profesionales e inmigrantes emergen problemas en la calidad técnica e interpersonal, que relacionan con la reducción de recursos durante la crisis. Respecto a la calidad técnica, los/las informantes describen un aumento de diagnósticos erróneos o inespecíficos, un uso inadecuado de pruebas y tratamientos inespecíficos, debido a la disminución del tiempo de consulta por la reducción de recursos humanos. Respecto a la calidad interpersonal, los/las profesionales señalaron menor empatía, mientras que los/las inmigrantes, además, una peor comunicación, que atribuyeron al cambio en las condiciones laborales de los/las profesionales y en la actitud de los/las inmigrantes. Finalmente, emergió la disminución de la capacidad resolutiva de los servicios: según los/las profesionales, por la repetición de consultas innecesarias en AP y limitadas en AS; según los/las inmigrantes jóvenes, por respuestas limitadas a sus problemas de salud.
ConclusionesLos resultados apuntan a un empeoramiento de la calidad técnica e interpersonal durante la crisis, por reducción de recursos, principalmente humanos, que afectan al conjunto de la población, pero en especial a las personas inmigrantes.
Since the start of the economic crisis in 2008, Spain has adopted various austerity policies aimed at the health system in response to pressures from multilateral financial institutions. Firstly, drastic cuts were made to public healthcare spending at national level (16.6% less in 2015 than in 2010),1 as well as at regional level, including Catalonia2 and healthcare coverage was restricted for certain benefits and population groups.3 Secondly, measures were introduced upon human resources (reductions in staff and salaries) and material resources (reducing investments and drug prices).4,5 These policies do not affect the whole population in the same way; vulnerable groups, due to their poorer living and working conditions, are at greater risk of exclusion from social and healthcare services,6,7 It is therefore to be expected that any changes in quality of care will be more marked for those groups and, among them, immigrants.8
Quality of care is defined as the degree to which health services increase the chance of achieving the desired outcome and are consistent with current scientific knowledge.9 Donabedian established three components to evaluate healthcare quality: structure, or the attributes of the settings in which care occurs; process, or the interaction between users and health services, including technical quality (knowledge and clinical criteria used to resolve health problems) and interpersonal quality (interpersonal exchange between health personnel and patients); and outcome of the care, or changes in health status as a result of the care received.10 This paper focuses on the interaction between users and providers, from the main actors’ viewpoint.
Although widely debated, the effects of the crisis on quality of health care have scarcely been analysed.11–14 In the international context, no studies were found. In the national context, some qualitative studies on the effect of the austerity measures on the national health system highlighted reductions in available resources that might affect the technical quality of care.15 Moreover available indicators show an increase in waiting times for consultation or tests16 and a rise in users who perceive the waiting lists as a problem,17 although levels of satisfaction remained steady.17 However, these databases do not easily permit differentiation according to nationality/origin.
Before the crisis, international evidence had highlighted inequalities in the technical quality of care given to immigrants, such as more diagnostic errors18 and shorter anamneses19 when a language barrier was present; worse monitoring of chronic patients,20 less diagnostic testing or more inappropriate hospital admissions.21 Some studies also described differences in interpersonal quality, with less empathetic treatment, insensitivity to cultural differences or worse communication.19,22–24 At national level, available evidence revealed less diagnostic testing in foreign patients.25
In summary, the evidence available on changes in quality of health care during the crisis is very limited; it does not focus on immigrant population, and incorporates only partially the actors’ viewpoint. This article, which presents partial results of a wider study,26,27 aims to analyse changes in the perceived quality of health care provided to the immigrant population during the economic crisis from the perspective of health professionals and users.
MethodsStudy designA qualitative descriptive-interpretative and exploratory study was conducted to analyse the phenomenon of study —changes in perceived quality of care provided to immigrants during the economic crisis— from the main social actors’ perspective. The study population was made up of health professionals and users of Moroccan and Bolivian origin in two counties of Catalonia: Baix Empordà and Barcelona, semi-rural and urban areas with a high proportion of immigrants (19.1% and 14.2% respectively). These countries of origin were chosen because they are amongst the largest groups 20.8% and 3.4% respectively, (first and sixth -but first of Latin America- groups of the foreign population in Catalonia28) and differ in relevant characteristics such as language, culture, etc. Fieldwork took place from November 2014 to September 2015.
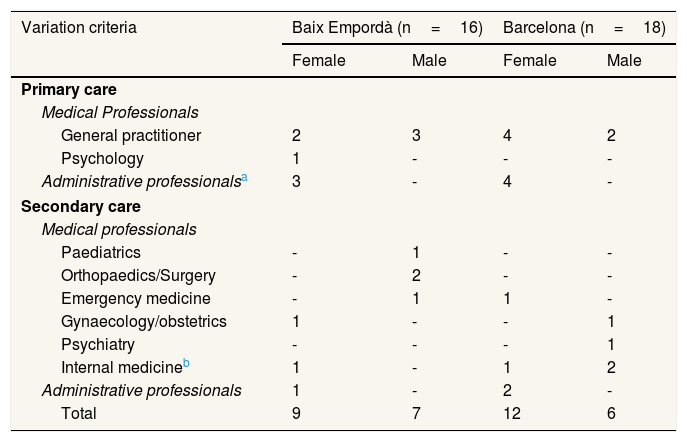
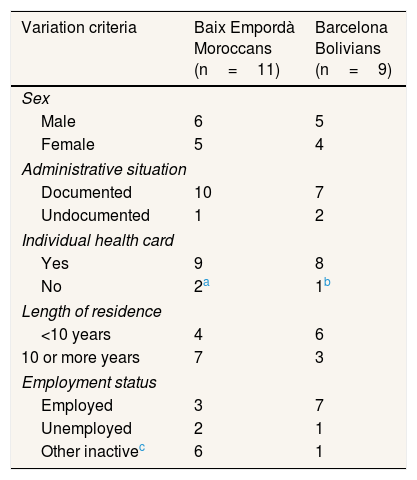
SamplingA theoretical sample was selected through a two-stage process. In the first stage, the contexts, primary care centres with the greatest proportion of immigrants and their referral hospitals were selected. In the second stage, informants were selected according to the following criteria in order to ensure variety in discourses: a) health professionals: medical and administrative personnel, from primary and secondary care, with different job profiles and more than 10 years’ work experience in the national health system, and b) users from Morocco or Bolivia with and without an individual healthcare card (IHC) and with at least 5 years’ residence in Spain. Reaching immigrants without IHCs proved more difficult than anticipated. In order to increase the recruitment chances, different strategies were applied: expansion of the study areas in Barcelona; collaboration with hospitals’ mediators; contacting NGOs and immigrants’ associations; direct recruitment by the first author in local stores, bars and consulates; posting announcements in public places; and snowballing. Due to the limited success, being without IHC was converted into a variation criterion. The final sample was determined by saturation (Tables 1 and 2). A member of the research team in most facilities (and a collaborator for SC in Barcelona) applying the defined criteria would select professionals and contact them for participation. Most users were identified by NGOs (when not directly by the first author). The first author then contacted those who agreed on participating to ensure that they complied with the criteria and to agree on the time and day for the interview.
Composition of final sample of health professionals by care level and study area.
| Variation criteria | Baix Empordà (n=16) | Barcelona (n=18) | ||
|---|---|---|---|---|
| Female | Male | Female | Male | |
| Primary care | ||||
| Medical Professionals | ||||
| General practitioner | 2 | 3 | 4 | 2 |
| Psychology | 1 | - | - | - |
| Administrative professionalsa | 3 | - | 4 | - |
| Secondary care | ||||
| Medical professionals | ||||
| Paediatrics | - | 1 | - | - |
| Orthopaedics/Surgery | - | 2 | - | - |
| Emergency medicine | - | 1 | 1 | - |
| Gynaecology/obstetrics | 1 | - | - | 1 |
| Psychiatry | - | - | - | 1 |
| Internal medicineb | 1 | - | 1 | 2 |
| Administrative professionals | 1 | - | 2 | - |
| Total | 9 | 7 | 12 | 6 |
Includes nephrology, endocrinology & nutrition, gastroenterology.
The selected centres in the semi-rural municipalities were Palafrugell, Palamós, La Bisbal d’Empordà, and Torroella de Montgrí, and in the urban areas: Raval, Sant Pere, Santa Caterina i la Ribera, Camp de l’Arpa del Clot, Clot, Bèsos i el Maresme, and Trinitat Nova.
Composition of final sample of immigrant users by sociodemographic characteristics and study area.
| Variation criteria | Baix Empordà Moroccans (n=11) | Barcelona Bolivians (n=9) |
|---|---|---|
| Sex | ||
| Male | 6 | 5 |
| Female | 5 | 4 |
| Administrative situation | ||
| Documented | 10 | 7 |
| Undocumented | 1 | 2 |
| Individual health card | ||
| Yes | 9 | 8 |
| No | 2a | 1b |
| Length of residence | ||
| <10 years | 4 | 6 |
| 10 or more years | 7 | 3 |
| Employment status | ||
| Employed | 3 | 7 |
| Unemployed | 2 | 1 |
| Other inactivec | 6 | 1 |
Individual, semi-structured interviews were carried out using a topic guide. The explored topics included perceived quality of health care provided to immigrants in general and of its technical and interpersonal components, resolution capacity; changes perceived during the crisis, and the attributed causes and mechanisms. Topics were addressed with open-ended and probing questions and were discussed as they came up during the interview. Interviews were conducted in places convenient to informants: with health personnel, in the health facilities, and with users their homes or community centres. They lasted between 40-80minutes, were audio-recorded and transcribed verbatim. An Arabic interpreter was needed in four interviews.
Data analysis and quality of informationThematic analysis was carried out using the Atlas-ti software. Data was segmented by areas and type of informants. Categories of analysis were generated through a process of mixing those from the topic guide with those emerging from the data. Themes were identified, coded, re-coded and classified in order to identify common patterns by looking at regularities, convergences and divergences in data in a process of constant comparison, going back and forth between the data and the conceptual framework. Quality was ensured through triangulation, by comparing different areas and groups of informants. Three analysts with different backgrounds and a good knowledge of the context participated in the analysis.
To identify the informants producing the discourse, a set of abbreviations is used: a) type of informant: medical professional (MP), administrative professional (AP), immigrant users (U); b) area: Barcelona (B), Baix Empordà (BE); and c) healthcare level: primary care (PC) or secondary care (SC); followed by a serial number.
Ethical considerationsThis study was approved by the Ethical Committee for Clinical Research of the Municipal Health Institute of Barcelona (2014/5708/I) and the Jordi Gol and Gurina Foundation (P14/159). Written consent was obtained from every participant prior to interview. Confidentiality and anonymity were guaranteed.
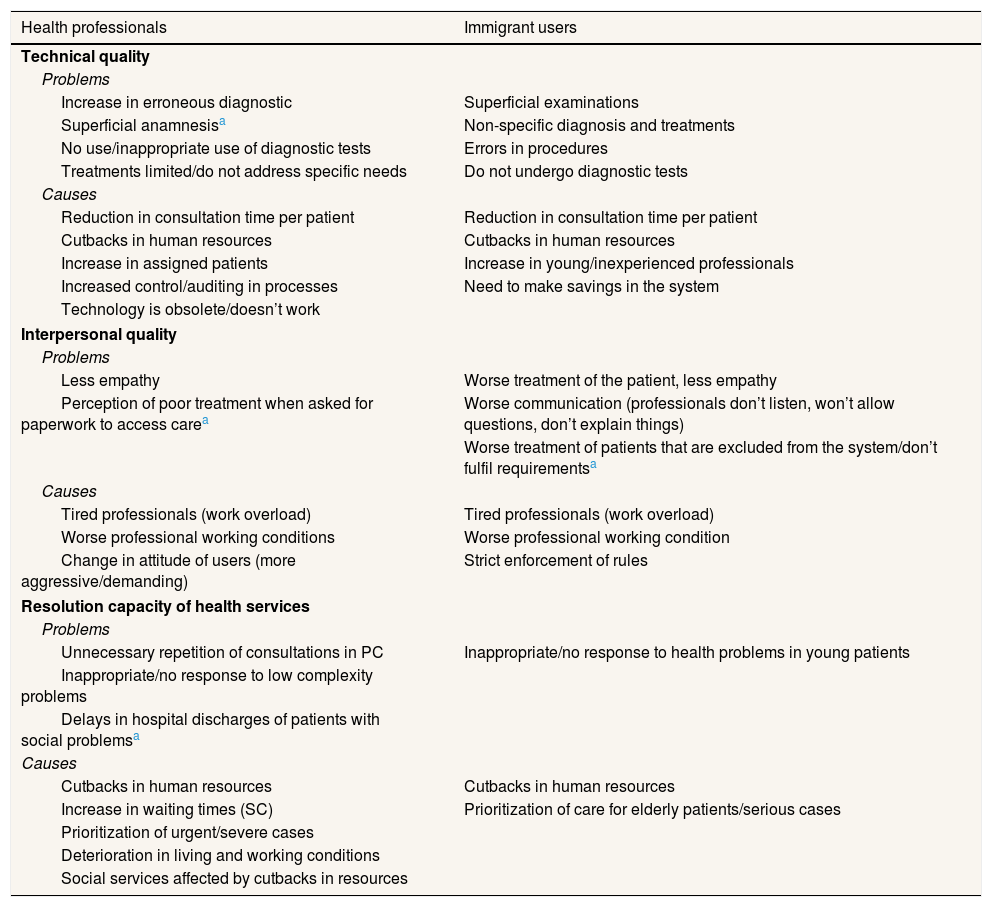
ResultsProblems emerged from the discourse of both professionals and users related to technical quality (increase in erroneous diagnoses, inappropriate tests) and interpersonal quality (worse treatment and communication) of the care provided, which they attributed to cutbacks in resources, mainly human, leading to reductions in consultation time, and changes in professionals’ working conditions during the crisis. Although they clearly affect the whole population, informants point out that some of these problems especially affect immigrants due to their particular characteristics (language-cultural barriers, limited entitlements, worse living conditions) (Table 3).
Changes in the quality of health care perceived by professionals and immigrant users during the economic crisis.
| Health professionals | Immigrant users |
|---|---|
| Technical quality | |
| Problems | |
| Increase in erroneous diagnostic | Superficial examinations |
| Superficial anamnesisa | Non-specific diagnosis and treatments |
| No use/inappropriate use of diagnostic tests | Errors in procedures |
| Treatments limited/do not address specific needs | Do not undergo diagnostic tests |
| Causes | |
| Reduction in consultation time per patient | Reduction in consultation time per patient |
| Cutbacks in human resources | Cutbacks in human resources |
| Increase in assigned patients | Increase in young/inexperienced professionals |
| Increased control/auditing in processes | Need to make savings in the system |
| Technology is obsolete/doesn’t work | |
| Interpersonal quality | |
| Problems | |
| Less empathy | Worse treatment of the patient, less empathy |
| Perception of poor treatment when asked for paperwork to access carea | Worse communication (professionals don’t listen, won’t allow questions, don’t explain things) |
| Worse treatment of patients that are excluded from the system/don’t fulfil requirementsa | |
| Causes | |
| Tired professionals (work overload) | Tired professionals (work overload) |
| Worse professional working conditions | Worse professional working condition |
| Change in attitude of users (more aggressive/demanding) | Strict enforcement of rules |
| Resolution capacity of health services | |
| Problems | |
| Unnecessary repetition of consultations in PC | Inappropriate/no response to health problems in young patients |
| Inappropriate/no response to low complexity problems | |
| Delays in hospital discharges of patients with social problemsa | |
| Causes | |
| Cutbacks in human resources | Cutbacks in human resources |
| Increase in waiting times (SC) | Prioritization of care for elderly patients/serious cases |
| Prioritization of urgent/severe cases | |
| Deterioration in living and working conditions | |
| Social services affected by cutbacks in resources | |
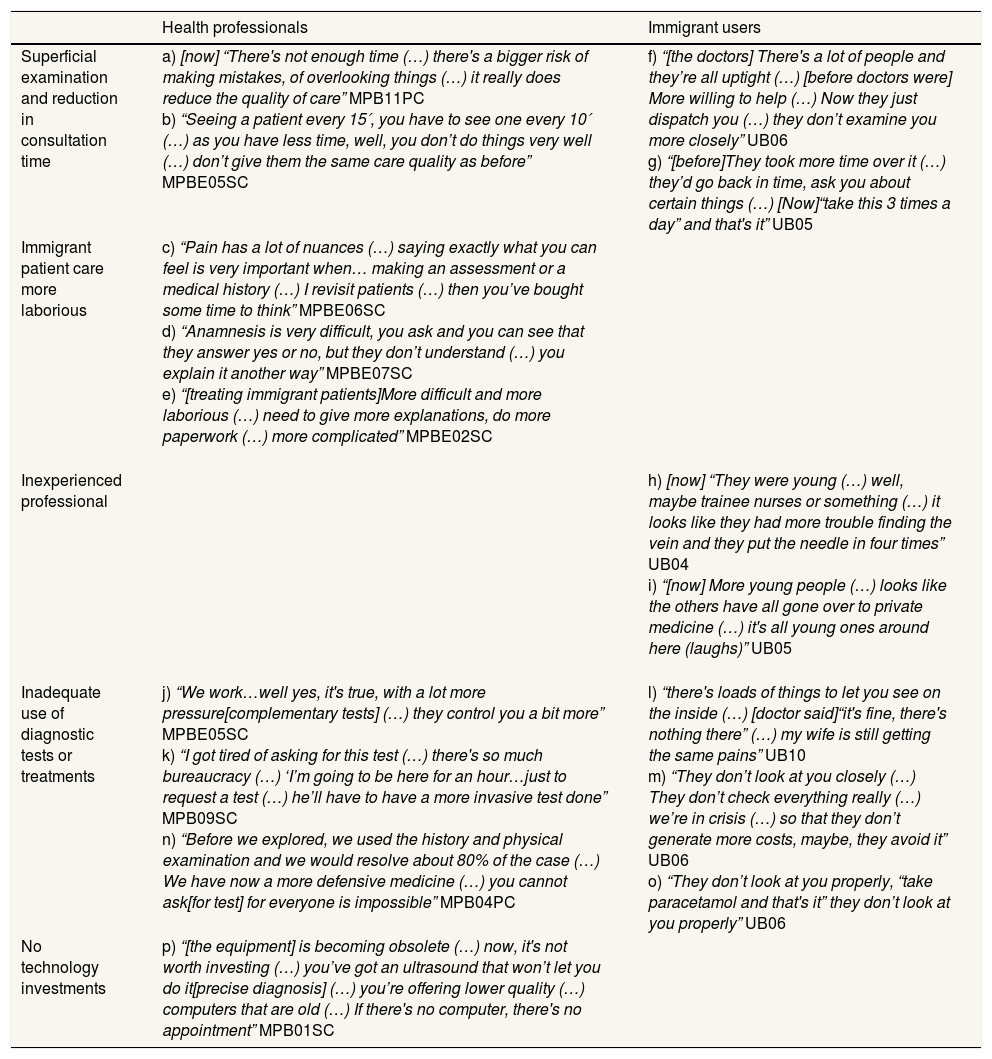
A deterioration in the diagnostic process emerged: while medical professionals refer to a potential increase in diagnostic errors and superficial anamneses, immigrants report superficial examinations and non-specific diagnoses and treatments. Both groups attribute these to a reduction in the time available per patient, which professionals considered insufficient and forces them to work quickly (“I can’t work as well as I’d like to [APBE02PC]”) (Table 4 a, b). Moreover, they highlight difficulties in producing a good anamnesis, especially for patients with a language barrier or cultural differences when reporting pain/discomfort. According to some professionals it makes caring for a patient a more “laborious” process (Table 4 c-e) and aggravates the pressure they are under as it prolongs consultation and waiting times. Immigrant users described superficial physical examinations and non-specific diagnoses and treatments: “[…need] to examine her more closely (…) I want to know what the problem is” (UB05) (Table 4 f, g). Both professionals and users attribute the reduction in consultation times to staff cutbacks leading to an increase in assigned patients. Some immigrant users in Barcelona attribute mistakes in procedures to the employment of young and inexperienced professionals (Table 4h, i).
Examples of verbatim of professionals and immigrant users on changes in the technical quality of health care during the economic crisis.
| Health professionals | Immigrant users | |
|---|---|---|
| Superficial examination and reduction in consultation time | a) [now] “There's not enough time (…) there's a bigger risk of making mistakes, of overlooking things (…) it really does reduce the quality of care” MPB11PC b) “Seeing a patient every 15′, you have to see one every 10′ (…) as you have less time, well, you don’t do things very well (…) don’t give them the same care quality as before” MPBE05SC | f) “[the doctors] There's a lot of people and they’re all uptight (…) [before doctors were] More willing to help (…) Now they just dispatch you (…) they don’t examine you more closely” UB06 g) “[before]They took more time over it (…) they’d go back in time, ask you about certain things (…) [Now]“take this 3 times a day” and that's it” UB05 |
| Immigrant patient care more laborious | c) “Pain has a lot of nuances (…) saying exactly what you can feel is very important when… making an assessment or a medical history (…) I revisit patients (…) then you’ve bought some time to think” MPBE06SC d) “Anamnesis is very difficult, you ask and you can see that they answer yes or no, but they don’t understand (…) you explain it another way” MPBE07SC e) “[treating immigrant patients]More difficult and more laborious (…) need to give more explanations, do more paperwork (…) more complicated” MPBE02SC | |
| Inexperienced professional | h) [now] “They were young (…) well, maybe trainee nurses or something (…) it looks like they had more trouble finding the vein and they put the needle in four times” UB04 i) “[now] More young people (…) looks like the others have all gone over to private medicine (…) it's all young ones around here (laughs)” UB05 | |
| Inadequate use of diagnostic tests or treatments | j) “We work…well yes, it's true, with a lot more pressure[complementary tests] (…) they control you a bit more” MPBE05SC k) “I got tired of asking for this test (…) there's so much bureaucracy (…) ‘I’m going to be here for an hour…just to request a test (…) he’ll have to have a more invasive test done” MPB09SC n) “Before we explored, we used the history and physical examination and we would resolve about 80% of the case (…) We have now a more defensive medicine (…) you cannot ask[for test] for everyone is impossible” MPB04PC | l) “there's loads of things to let you see on the inside (…) [doctor said]“it's fine, there's nothing there” (…) my wife is still getting the same pains” UB10 m) “They don’t look at you closely (…) They don’t check everything really (…) we’re in crisis (…) so that they don’t generate more costs, maybe, they avoid it” UB06 o) “They don’t look at you properly, “take paracetamol and that's it” they don’t look at you properly” UB06 |
| No technology investments | p) “[the equipment] is becoming obsolete (…) now, it's not worth investing (…) you’ve got an ultrasound that won’t let you do it[precise diagnosis] (…) you’re offering lower quality (…) computers that are old (…) If there's no computer, there's no appointment” MPB01SC |
Secondly, professionals and users report the inadequate use of diagnostic tests and limitations to treatments. Some professionals point out that they are unable to request all the necessary tests or they substitute them for more invasive procedures in order to avoid the additional bureaucracy involved in getting the most suitable tests performed (Table 4 j, k). According to immigrants, the professionals “avoid” requesting diagnostic tests due to cutbacks in spending during the crisis (Table 4 l, m): “They avoid doing tests (…) We’re in times of crisis (…) they don’t generate more costs” (UB06). However, a PC doctor considered that restricting tests had allowed them to go back to being a complement to physical examination and anamnesis (Table 4 n). Professionals also point out restrictions on treatments (those considered non-first choice), hence they are not always able to adapt them to the patient's individual needs, and they attribute this to increased controls on spending since the economic crisis: “They control you more. Resources have been severely limited (…) what isn’t in the [clinical] guidelines as the first choice (…) you have to justify” (MPBE07PC). Users report the prescription of non-specific treatments (analgesics), with no alternatives offered when the health problem is not resolved (Table 4 o).
Some SC doctors in Barcelona highlight difficulties in making more precise diagnoses because the technology used is obsolete or does not work properly, which they attribute to a lack of investment due to budget restrictions (Table 4 p).
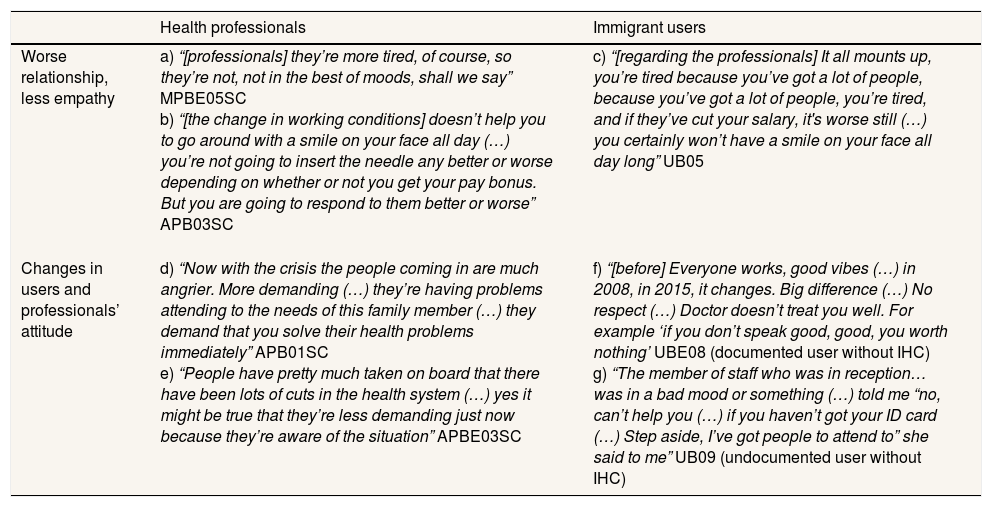
Changes perceived in interpersonal qualityProfessionals and users generally perceived that the relationship between professional-patient has deteriorated in recent years. Medical professionals indicate that less empathetic responses on their part are more common (Table 5 a, b), whilst immigrants, in addition to perceiving they are treated worse, report worse communication because medical staff do not allow them to ask questions or provide explanations “they don’t listen like they used to” (UB09) (Table 5 c). Both groups attribute this to tiredness due to the increasing work overload and worse working conditions of professionals, but also to a change in the attitude of both professionals and users (Table 5 d, e). According to medical professionals, although some users are more understanding because of the crisis, others are more demanding and insist on immediate solutions. According to administrative professionals, this leads mostly immigrant users to perceive they are being treated poorly when they are asked to present paperwork in order to access care: “We’re not out to screw the patient over (…) I can’t [give them access]” (APB06PC). Nevertheless, some users perceive that they are treated as if they were “worth nothing” (UBE08) and they attribute this to their situation of exclusion from the system (Table 5 f, g).
Examples of verbatim of professionals and immigrant users on changes in interpersonal quality of care during the economic crisis.
| Health professionals | Immigrant users | |
|---|---|---|
| Worse relationship, less empathy | a) “[professionals] they’re more tired, of course, so they’re not, not in the best of moods, shall we say” MPBE05SC b) “[the change in working conditions] doesn’t help you to go around with a smile on your face all day (…) you’re not going to insert the needle any better or worse depending on whether or not you get your pay bonus. But you are going to respond to them better or worse” APB03SC | c) “[regarding the professionals] It all mounts up, you’re tired because you’ve got a lot of people, because you’ve got a lot of people, you’re tired, and if they’ve cut your salary, it's worse still (…) you certainly won’t have a smile on your face all day long” UB05 |
| Changes in users and professionals’ attitude | d) “Now with the crisis the people coming in are much angrier. More demanding (…) they’re having problems attending to the needs of this family member (…) they demand that you solve their health problems immediately” APB01SC e) “People have pretty much taken on board that there have been lots of cuts in the health system (…) yes it might be true that they’re less demanding just now because they’re aware of the situation” APBE03SC | f) “[before] Everyone works, good vibes (…) in 2008, in 2015, it changes. Big difference (…) No respect (…) Doctor doesn’t treat you well. For example ‘if you don’t speak good, good, you worth nothing’ UBE08 (documented user without IHC) g) “The member of staff who was in reception… was in a bad mood or something (…) told me “no, can’t help you (…) if you haven’t got your ID card (…) Step aside, I’ve got people to attend to” she said to me” UB09 (undocumented user without IHC) |
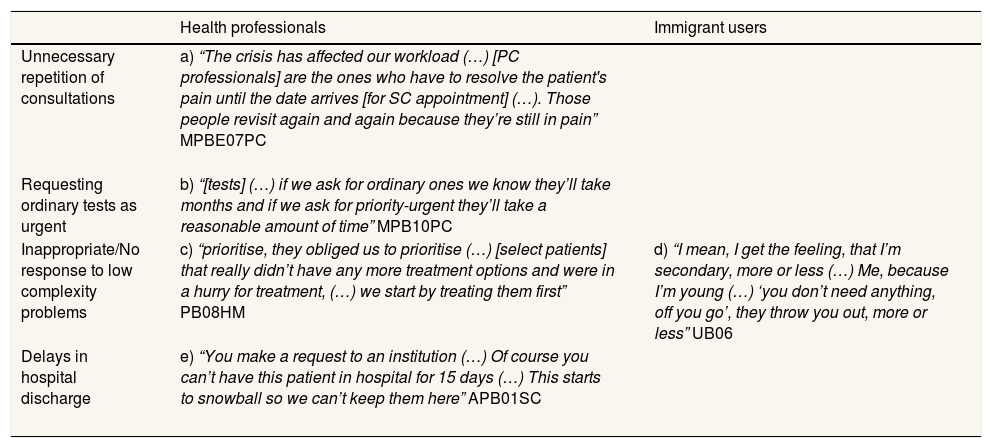
In the discourse of medical professionals and immigrant users, a reduction in the resolution capacity of the health services emerges marginally, in both care levels but especially in primary care. PC doctors report the repetition of consultations for patients waiting to receive SC (surgery or diagnostic tests) which, in addition to not resolving the problem, reduces accessibility to PC (Table 6 a) and leads some medical professionals to mark requests for ordinary tests as priority/urgent (Table 6 b). In SC, medical professionals highlight inappropriate responses or a failure to respond to problems of low complexity because they prioritise the most severe/urgent cases (Table 6 c). “Our main (…) priority is severity (…) low complexity problems (…) you don’t give them any answers” (MPB06SC). Likewise, some young immigrants perceive that their problems are relegated in the face of more complex cases and that they are treated as “secondary” (UB06) (Table 6 d).
Examples of verbatim of professionals and immigrant users on changes in the resolution capacity of the health services.
| Health professionals | Immigrant users | |
|---|---|---|
| Unnecessary repetition of consultations | a) “The crisis has affected our workload (…) [PC professionals] are the ones who have to resolve the patient's pain until the date arrives [for SC appointment] (…). Those people revisit again and again because they’re still in pain” MPBE07PC | |
| Requesting ordinary tests as urgent | b) “[tests] (…) if we ask for ordinary ones we know they’ll take months and if we ask for priority-urgent they’ll take a reasonable amount of time” MPB10PC | |
| Inappropriate/No response to low complexity problems | c) “prioritise, they obliged us to prioritise (…) [select patients] that really didn’t have any more treatment options and were in a hurry for treatment, (…) we start by treating them first” PB08HM | d) “I mean, I get the feeling, that I’m secondary, more or less (…) Me, because I’m young (…) ‘you don’t need anything, off you go’, they throw you out, more or less” UB06 |
| Delays in hospital discharge | e) “You make a request to an institution (…) Of course you can’t have this patient in hospital for 15 days (…) This starts to snowball so we can’t keep them here” APB01SC |
Lastly, some social workers in Barcelona point out delays in the discharge from hospital of patients who are clinically stable but have social problems (mostly immigrants), since this hinders the appropriate use of hospital beds (Table 6 e).
DiscussionThe results of the study allow us to identify changes in quality of care related to austerity measures during the economic crisis, as perceived by professionals and immigrant users. These changes have scarcely been studied so far, either for the general population or for immigrants in particular. The results pinpoint problems of both technical quality (erroneous diagnoses; inappropriate diagnostic tests/treatments) and interpersonal quality (worse treatment and communication) in addition to a reduction in the resolution capacity of the health services (unnecessary consultations). The problems described are attributed to cutbacks in resources, mainly of personnel, in the context of the crisis. Although these changes affect the whole population, they are more evident in immigrant users due to certain specific characteristics. Changes in access to the services, one component of quality, have been analysed elsewhere.27
Less consultation time and restrictions of diagnostic testsThe results point to a deterioration in technical quality related to the reduction in consultation times, also described in previous studies15,29 and restrictions on diagnostic tests and treatments, attributed to cutbacks in resources, especially health personnel. This suggests that diagnostic errors may have increased during the crisis, due to superficial anamnesis and examinations and an inappropriate use of tests. Further research is required on medical errors to contrast these results.
These problems appear to affect immigrant users more acutely. Some are consistent with problems described in immigrant care prior to the crisis, in this30 and other contexts,19 but seem to have become more acute. Allowing enough time is particularly relevant for immigrant patients when making a diagnosis, because of the communication difficulties that often arise due to linguistic/cultural barriers and which may be further complicated by the reduction in mediation staff.
Furthermore, the inappropriate use of tests and treatments due to restrictions, although it affects the whole population, could translate into an increase in the inequities described in previous studies showing that immigrants undergo less diagnostic testing and experience longer waiting times for appointments in SC.25,31
Worse treatment and communication for immigrant patientsProfessionals and users coincide in reporting that treatment to patients had got worse and they attributed this to a deterioration in the working conditions of professionals and a change in the attitude of patients. This result is in contrast with available indicators according to which the personal treatment received from professionals remained highly rated in Catalonia and Spain (1995-2015),17 although this difference may be because the data is not disaggregated by the origin of the user.
Professionals attribute this not only to the work overload but also to a more demanding attitude of patients because of the economic crisis, although in previous studies professionals associated this attitude (more aggressive or demanding) with certain groups of immigrants,32 so this may be reflecting the professionals prejudice rather than the actual situation of crisis. Users report worse treatment from administrative staff towards the most vulnerable (particularly, those without IHC) which may indicate variability in their responses. Receiving an inadequate treatment is especially relevant because it can have a dissuasive effect on immigrants’ use of the health services.27
Reduction in the resolution capacity of the health servicesAlthough our study does not allow us to evaluate the effectiveness of interventions, the results appear to indicate a reduction in the resolution capacity of the health services, in both care levels but especially in PC, due to cutbacks in human resources and a consequent increase in waiting times for SC. These results are consistent with the increase in average waiting times for basic specialties,16 or worsening of some quality indicators such as avoidable hospital admissions for congestive heart failure (CHF) in adults that increased by 1.8% over the period 2008-2013.33
Delays in hospital discharges for socially vulnerable patients, apart from contributing to a reduction in the effectiveness of the services, is evidence that the health system is containing problems that should be addressed by other sectors, such as social services, which have also been affected by policies adopted in the context of the crisis.
Increased workload and deteriorating working conditions of professionalsThe deterioration in working conditions of the health professionals due to increasing workloads emerges as a reason for the drop in technical and interpersonal quality of care. During the crisis, policies were designed that affected the pay of NHS staff (RDL 08/2010; RDL 20/2012; Ley 2/2012), although their implementation has varied among the autonomous region. The data is difficult to access, but available studies indicate a generalized reduction in variable bonus payments over the period 2009-2014 and they have disappeared altogether in some regions.34 Moreover, health professionals without a permanent position work on average 5.73 contracts per year, of a duration of less than six months or part time.35 Furthermore, the presence of young, inexperienced professionals, which users relate to a loss of care quality, could be an indication of a lack of staff to oversee training due to retired professionals not being replaced.
LimitationsAs reaching migrants without IHCs was more difficult than expected, identified changes in perceived quality of care might be worse than our results suggested. Results are based on main actor's opinions, hence further studies are needed to deepen the analysis and establish the size of the problem.
ConclusionsThis study allowed to identify changes perceived in the quality of care provided to the immigrant population during the economic crisis. Professionals and users identify changes in both technical and interpersonal quality, mainly related to structural changes and specifically to cutbacks in human resources. Although these changes affect the whole population, they are especially relevant to vulnerable population, especially immigrants due to some specific characteristics.
However, further analysis is needed to identify the magnitude of the changes described. Nevertheless, these results should be seen as a warning sign of the potential effects of austerity measures on quality of care. Public policies aimed at improving the efficiency of the health system, such as those introduced during the crisis, should ensure that while unnecessary components are suppressed, all necessary are kept to ensure the proper functioning of the system, avoiding putting at risk equitable access to quality care.
Before the crisis, national and international evidence highlighted inequalities both in technical and interpersonal quality given to immigrants. During the crisis, the available evidence is scarce. No international studies were found and national databases showed that some indicators have worsened though they do not allow disaggregation by origin.
What does this study add to the literature?This study identifies changes in quality of care related to austerity measures during the crisis, perceived by professionals and immigrant users. These changes have scarcely been studied so far. Results pinpoint problems in technical and interpersonal quality and a reduction in the health services effectiveness.
María del Mar García-Calvente.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsM.L. Vázquez and I. Vargas were responsible for the overall design and supervision of the project. V. Porthé contributed to the final version of the research tools, conducted the field work and analysis of data and produced, together with M.L. Vázquez and I. Vargas the first version of the paper. All authors contributed to the interpretation of data and provided feedback on preliminary versions of the paper. They approved the final version for its publication.
FundingThe research leading to these results has received funding from the Instituto de Salud Carlos III and the European Regional Development Fund (FEDER) (PI13/00261). The funding sources had no involvement in study design, nor in the collection, analysis and interpretation of the data, nor in writing the article and the decision to submit it for publication.
Conflict of interestsNone.
The authors thanks to the rest of the MEISI I project researchers and its institutions: M. Ballesta, Servicio de Epidemiología de la Región de Murcia; L. Colomes, SAGESSA; J. Llopart, Badalona Serveis Assistencials; J.L. Heras, Hospital Universitario Ramón y Cajal, Madrid; Belén Sanz, Escuela Nacional de Sanidad, Instituto de Salud Carlos III, CIBERESP, Madrid; and Isabel Plaza, Institut Català de la Salut, Barcelona. They are especially grateful to people that participated in the study and generously shared their time: F. Cots Reguant, Parc de Salut Mar; Y. El Haddouchi y P. Veth, Serveis de Salut Integrats Baix Empordà; and also NGOs and immigrants’ associations. We thank K. Bartlett for the English version of this article.