To analyze women's advancement compared with that of men and to determine whether advancement in hierarchical status differs from advancement in the professional recognition achieved by women from 1996 to 2008.
MethodsA retrospective study was carried in Hospital Clínic in Barcelona. We analyzed data on temporary and permanent positions, hierarchy, promotions, specialty, age, and sex among the participants.
ResultsThe female-to male ratio among trainee medical specialists was higher than 1 throughout the study period. After completion of specialist training, the proportion of women with temporary contracts more than doubled that of men. Less than 50% of women achieved permanent positions compared with 70% of men. For permanent non-hierarchical and hierarchical positions, the female-to-male ratio gradually decreased from 0.5 to below 0.2. Although more than 50% of trainee specialists were women, the number of female consultants remained 25% lower than that of men. In 2008, the final year of the study, the percentage of women who had achieved the grade of senior consultant was one-third that of men (29.5% of men vs 10.9% of women; p<0.0001).
ConclusionsThe significant differences in medical positions held by men and women illustrate the ‘leaky pipeline phenomenon’, consisting of a disproportionately low number of women achieving leading medical positions. The full potential of the increasing number of women physicians will not be reached without continuing efforts to improve the hospital medicine environment.
Analizar el avance de las mujeres en comparación con los hombres en la medicina y analizar si el avance jerárquico difiere del avance en su reconocimiento profesional en el periodo 1996-2008.
MétodosEstudio retrospectivo en el Hospital Clínic de Barcelona mediante el análisis de datos relativos a posición temporal y permanente, jerarquía, carrera profesional, especialidad, edad y sexo de los médicos.
ResultadosLa proporción de mujeres y hombres entre residentes fue superior a 1 durante el período de estudio. Finalizada la residencia, la proporción de mujeres dobla la proporción de hombres entre posiciones médicas temporales. Menos del 50% de las mujeres en comparación con el 70% de los hombres logra posiciones médicas permanentes. La proporción de mujeres y hombres entre posiciones permanentes no jerarquizadas y jerarquizadas desciende gradualmente desde 0.5 hasta llegar a menos de 0.2. A pesar de que más del 50% de residentes son mujeres, ellas alcanzan el grado de consultor 25% menos que sus colegas masculinos. En 2008, el último año del estudio, un tercio de las mujeres (10,9%) en comparación con los hombres (29,5%) alcanzó el grado de consultor senior (p<0.0001).
ConclusionesDiferencias significativas en posiciones médicas entre hombres y mujeres configuran el fenómeno conocido como “tuberías con fugas”’, que consiste en un número desproporcionado de mujeres que llegan a posiciones médicas principales. El potencial de la feminización médica no se alcanzará sin esfuerzos de mejora ambiental continua en la medicina hospitalaria.
The presence of women in the practice of medicine goes back to the ancient times. Some women were canonized in the 10th and 11th centuries for their care during the European plagues. From the 13th century to the 18th century, healing women were considered as witches and forbidden access to the medical education of the time. This ban lasted until the first half of the 19th century, thereby justifying the inferiority of women. It was not until the end of the 19th century that women were able to have access to training in medicine. In Spain women did not have access to higher education until the 20th century, and full incorporation into the medicine began in the 1970s with their incorporation into the world of work.
Over the past four decades, the number of women physicians has increased from less than 10% of the medical students and less than 15% of practicing physicians to being the majority of new graduates in medicine and more than 40% of practicing physicians in Western countries1. The proportion of women among Spanish collegiate physicians as a whole has risen to 93.4% in contrast with men who have barely increased 12.6% from 1994 to 20112. Women physicians represent more than 70% of the practitioners in primary health care and more than 40% in the Catalan hospital setting3.
Although the feminization of medicine in the developed world has risen dramatically, women are under-represented in the advanced echelons, with a remarkable lack of female leaders reaching the rank of full professor4,5. Studies on the representation of women among higher medical staff positions undertaken in the United States emphasize the potential conflict that may ensue from being both a physician and a mother which appears to be less a cause of dissatisfaction than the opportunity for advancement and practice control in their careers6,7. In the United Kingdom, since the early 1990s, the probability that fewer women than men doctors reached the category of consultant appears to be associated with a previous part-time contract with the British National Health Service8. In Spain, the advance of women physicians in their careers is unknown due to reluctance to provide such data.
We obtained data from the Hospital Clínic of Barcelona (HCB) and analyzed the proportion of women and men holding temporary, permanent and managerial medical positions, as well as the gender ratios for each of the promotion grades over the past ten years. The structure and medical organization of the HCB has been reported previously9.
This article evaluates the advance of women in comparison with men in medicine and determines whether the advance between the hierarchical status and the professional recognition achieved by women differs. We analyzed the disparity between women and men physicians along the formal hierarchal promotion process and the recognition of professional career promotion in the 21st century.
MethodsA retrospective longitudinal descriptive study was designed. Data related to the medical workforce were obtained from the Human Resources Department of the HCB. All physicians working at the hospital in October 1996 were included, using information based on gender, age, medical specialty and professional status. Calculation of the sample size was not done since the sample size was the total number of physicians.
VariablesThe two main variables studied were the hierarchical status and the grade of professional career. The following variables were studied: permanent, temporary and training medical positions and data related to medical executive management hierarchy and professional career (PC) promotion within the permanent positions.
Regarding the category of executive management hierarchy, data on the section or unit chief, department and institute chairs; grade attained on PC promotion: specialist, senior specialist, consultant and senior consultant; specialty, sex and age from 1996 to 2008 were collected.
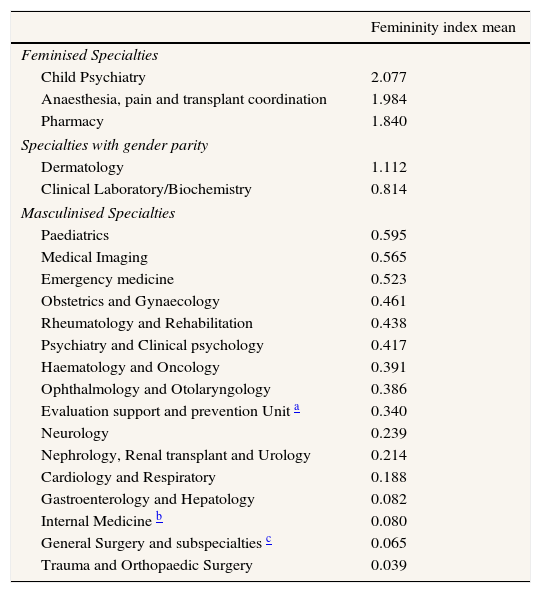
Feminization was evaluated as femininity index. This is a measure of frequent use and simple interpretation and defined as the percentage representing women with respect to the total of the variable. The ratio between the number of women and men in permanent medical positions, and in hierarchal positions and PC promotion within the permanent positions was calculated. According the femininity index in each specialty, we classified the specialties into three groups: i) feminised specialties, if the relationship was more than 1; ii) parity specialties, if the relationship was 1; iii) and masculinised specialties, if the relationship was less than 1.
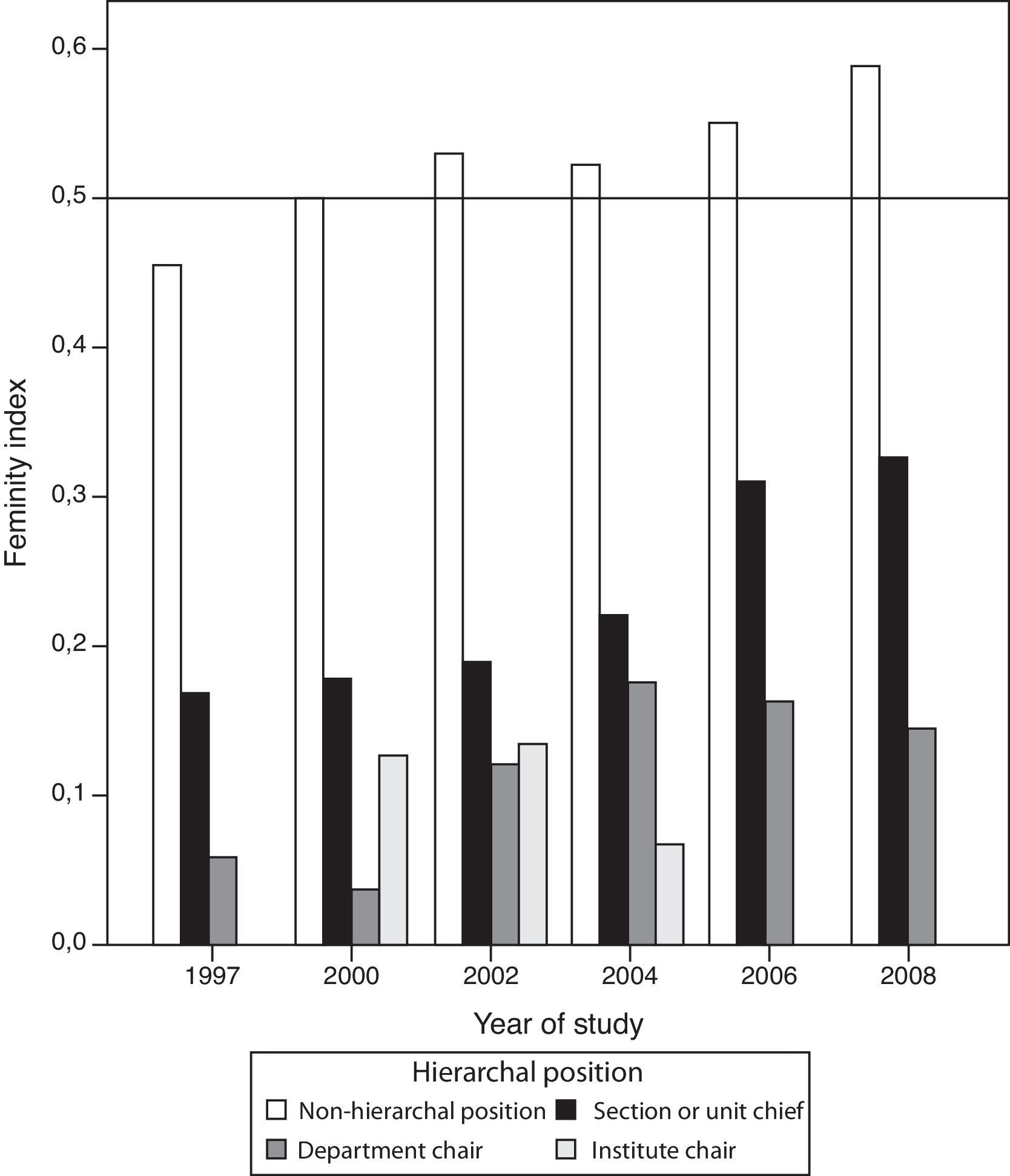
Statistical analysisThe demographic characteristics of the medical workforce by year of study were expressed as absolute frequencies. The femininity index related to positions of hierarchy was plotted using a bar graph. The Chi-square and the Fisher exact tests were used to compare differences in the proportion of the type of employment status–permanent and temporary - and hierarchal positions held by men and women. The association between age, hierarchal position and sex was analysed with the ANOVA test.
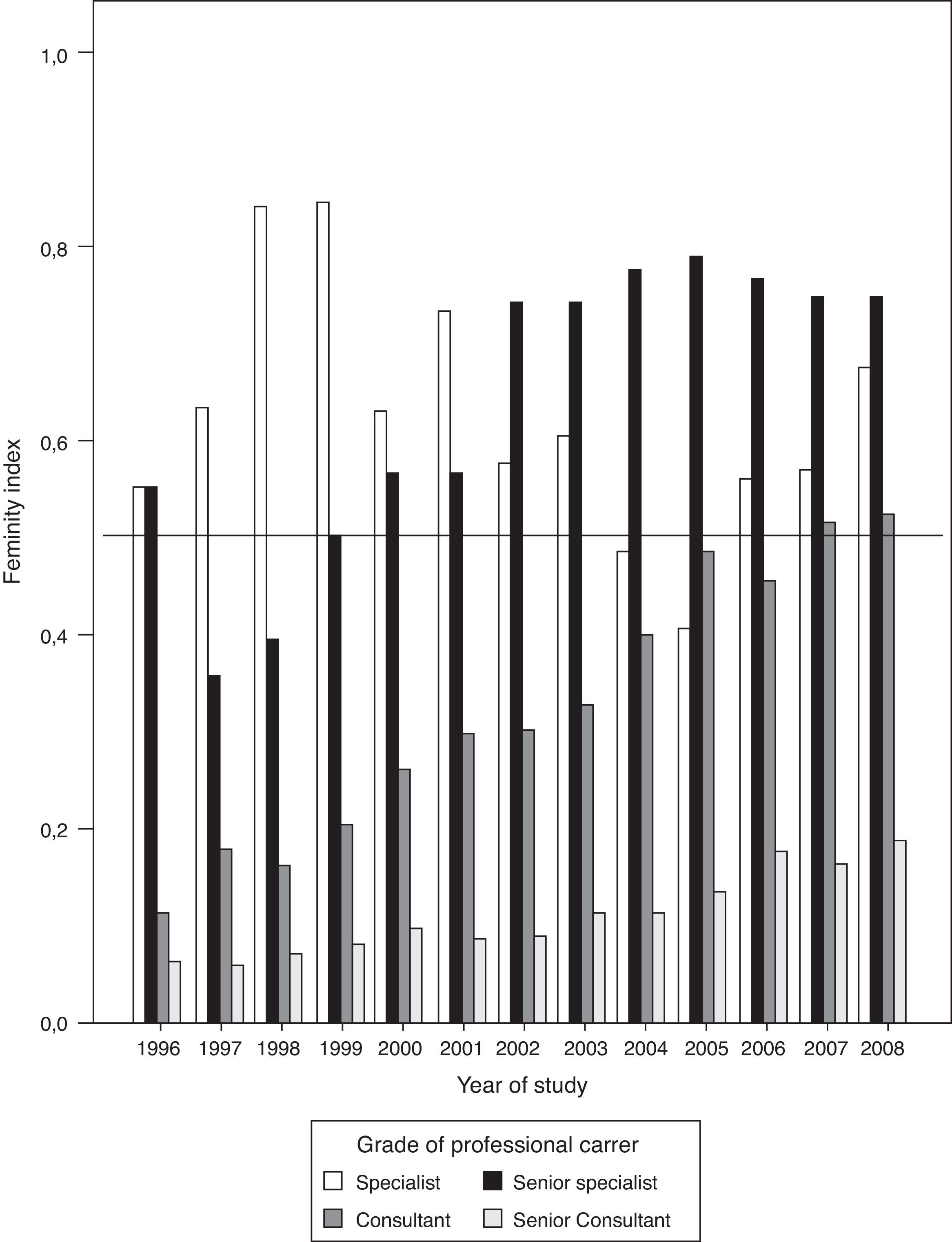
The ratio of the number of female versus male physicians, femininity index, and relation to the grade of PC was represented by a bar graph. A Chi-square test was used to determine trends related to hierarchal positions and grade of PC over the study period. A time series analysis was not used because the number of years studied - or periods - was small. A Chi-square was used for linear trend in order to study the increase in the number of women physicians for each degree of promotion during the study period.
ResultsThe study was made up of 695 physicians, 216 women and 479 men. Professionals beginning work from 1996 and 2008 were also included, raising the number of physicians studied to 1135, 492 women and 643 men at the end of the study period in 2008.
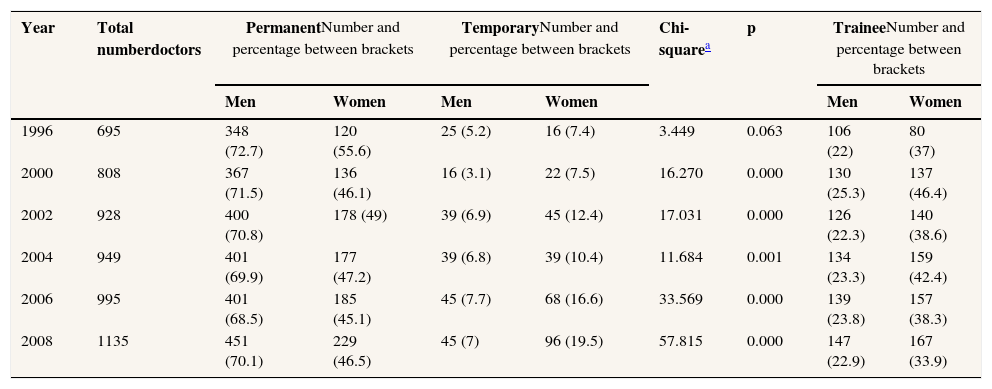
The number of women physicians holding a training medical specialist position at the HCB has been greater than 50% since 2000. Thus, the ratio of the femininity index among the trainees was from 1.05 in 2000 to 1.14 in 2008. After completion of their specialist training women held significantly more than double the temporary medical positions than men, with less than 50% of women compared to 70% of men physicians achieving permanent positions (p<0.001) (Table 1).
Demographic characteristics of the medical workforce at the Hospital Clínic from 1996 to 2008.
| Year | Total numberdoctors | PermanentNumber and percentage between brackets | TemporaryNumber and percentage between brackets | Chi-squarea | p | TraineeNumber and percentage between brackets | |||
|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | ||||
| 1996 | 695 | 348 (72.7) | 120 (55.6) | 25 (5.2) | 16 (7.4) | 3.449 | 0.063 | 106 (22) | 80 (37) |
| 2000 | 808 | 367 (71.5) | 136 (46.1) | 16 (3.1) | 22 (7.5) | 16.270 | 0.000 | 130 (25.3) | 137 (46.4) |
| 2002 | 928 | 400 (70.8) | 178 (49) | 39 (6.9) | 45 (12.4) | 17.031 | 0.000 | 126 (22.3) | 140 (38.6) |
| 2004 | 949 | 401 (69.9) | 177 (47.2) | 39 (6.8) | 39 (10.4) | 11.684 | 0.001 | 134 (23.3) | 159 (42.4) |
| 2006 | 995 | 401 (68.5) | 185 (45.1) | 45 (7.7) | 68 (16.6) | 33.569 | 0.000 | 139 (23.8) | 157 (38.3) |
| 2008 | 1135 | 451 (70.1) | 229 (46.5) | 45 (7) | 96 (19.5) | 57.815 | 0.000 | 147 (22.9) | 167 (33.9) |
Child psychiatry and anaesthesia were feminised specialties. Dermatology and laboratory (clinical chemistry, microbiology, pathological anatomy, genetics and immunology) specialties appeared to show gender parity. In nine specialties, the mean ratio of the femininity index was less than 0.59 to 0.34, and finally, 7 specialties were strongly masculinised, with 24% (neurology) to 3% (trauma and orthopaedic surgery) of these specialties being comprised of women (Table 2).
Femininity index - ratio between the number of women and men - in permanent medical positions in the specialties throughout the study period.
| Femininity index mean | |
|---|---|
| Feminised Specialties | |
| Child Psychiatry | 2.077 |
| Anaesthesia, pain and transplant coordination | 1.984 |
| Pharmacy | 1.840 |
| Specialties with gender parity | |
| Dermatology | 1.112 |
| Clinical Laboratory/Biochemistry | 0.814 |
| Masculinised Specialties | |
| Paediatrics | 0.595 |
| Medical Imaging | 0.565 |
| Emergency medicine | 0.523 |
| Obstetrics and Gynaecology | 0.461 |
| Rheumatology and Rehabilitation | 0.438 |
| Psychiatry and Clinical psychology | 0.417 |
| Haematology and Oncology | 0.391 |
| Ophthalmology and Otolaryngology | 0.386 |
| Evaluation support and prevention Unit a | 0.340 |
| Neurology | 0.239 |
| Nephrology, Renal transplant and Urology | 0.214 |
| Cardiology and Respiratory | 0.188 |
| Gastroenterology and Hepatology | 0.082 |
| Internal Medicine b | 0.080 |
| General Surgery and subspecialties c | 0.065 |
| Trauma and Orthopaedic Surgery | 0.039 |
The ratios between the numbers of women versus men among permanent medical positions were around 0.5 (0.45-0.60) for non-hierarchal positions and markedly decreased below 0.2 for hierarchal positions throughout the study. According to data from 2006, this ratio slightly rose to 0.3 for section or unit heads, the lowest hierarchal position, but no trend to an increase was observed in any hierarchal position (p>0.05) (Fig. 1).
Among the doctors with hierarchal positions (section or unit chief, department and institute chairs), the proportion of women was 8.1%, 5.8%, 7.3%, 9%, 10.2% and 8.3% versus the proportion of men which was 24.4%, 20.5%, 21.4%, 22.5%, 23.3% and 20.08% in 1998, 2000, 2002, 2004, 2006 and 2008, respectively (p<0.001).
The difference in age of institute and department chairs was 13.13±0.82 years (mean±standard deviation) while that for section or unit heads was 8.33±0.66 years, being greater than the remaining non hierarchal permanent medical positions (F=266.53, p<0.001) with no significant differences related to hierarchal positions between the two genders.
Professional career promotionPromotion for women in comparison with men physicians under the PC system followed a different pathway throughout the study. Male physicians developed homogeneous progression through the 4 successive grades of PC with almost half of those applying for any grade of promotion achieving success, while significantly fewer women doctors attained the grade of consultant: 49.5% versus 37.4% (p=0.01), respectively. The ratios between women versus men among permanent medical positions did not show equity for almost any of the grades of PC promotion. There was no significant change in the number of women specialists (Chi-square=0.64, p=0.423). On the other hand, the number of women in senior specialist (Chi-square=34.19, p<0.001), consultant (Chi-square=52.29, p<0.001) and senior consultant (Chi-square=12.79, p<0.001) positions increased significantly throughout the study period (Fig. 2). However, in 2008, the last year of the study, one-third of women (10.9%) compared to men (29.5%) (Chi-square =32.68, p<0.0001) reached the grade of senior consultant. Otherwise, more than 65% of the consultants (p<0.0001) and more than 85% of senior consultants (p<0.0001) continued to be men.
DiscussionThis study shows significant differences between women and men holding permanent medical positions. These differences progressively increase in relation to the grade of advancement over hierarchal promotion as well as over PC promotion. Therefore, when male physicians apply for promotion, female physicians have not yet obtained a permanent position, delaying the time for promotion compared to that of male physicians with similar years of professional experience. These differences in permanent medical positions held by men and women are the basis of the ‘leaky pipeline phenomenon’, indicating a disproportionate low number of women achieving leading medical positions and advancement in PC promotion. Although the grade of PC promotion for women physicians slightly increased throughout the study, the results show that professional promotion is harder for women than for men in medicine, and add weight to earlier suggestions derived in a previous one-year study performed in two Catalan hospitals9. The difference between women and men physicians in relation to PC promotion agrees with the growing gender gap in the starting salaries of physicians after adjustments for hours worked in internal medicine, paediatrics, family practice and emergency medicine10,11.
Some authors have pointed out that a gender role contributes to the trends in the popularity of specialties for women. Academic achievement and the duration of medical studies could influence specialty preference12. Being female and having a parent in general practice was found to be positively associated with a preference for a career in general practice and paediatrics. Among first-year students and in those with no clerkship experience, female gender was positively associated with a preference for psychiatry. In fact, the three specialties - primary care in family medicine, paediatrics, and psychiatry–are all related to higher importance on the perspective-taking scale of the empathy measure that is a female belief within the culture. Among students with clerkship experience and final-year students the duration of study was positively associated with a preference for a career in internal medicine. Surgical specialties continue to be chosen three times more frequently by men than by women doctors.
Personality factors had many indirect influences upon sex. A questionnaire conducted among 2867 British medical students was assessed by path analysis factors which could be grouped as four types of motivations - helping people, respect, science and indispensability- indicated the attraction of different aspects of medical practice13. Helping people was particularly related to agreeableness and interest in general practice, paediatrics, geriatric medicine, and with none of the specialities. Respect was related to a surface approach to learning, and science being more open to experience and related to pathology. Indispensability was related to higher strategic learning scores, lower fantasy and stress scores and interest in surgery and acute medical specialties. Therefore, feminization of the medical profession suggests the need for measures to stimulate the interest of female medical students in the surgical field in order to optimize human resources in the current health care systems.
The rapid increase of the number of female medical students in Spain over the past three decades is now being reflected by the growing proportions of women in all medical specialties14. Nonetheless, according to data from our hospital, most medical specialties still show a predominant number of men in comparison with women among the permanent specialist positions, with the difference in favour of men being even greater among higher hierarchal positions.
It has been suggested that the slower career progression of women compared with their male colleagues is a cohort effect; therefore women will increasingly assume leadership roles as they mature in the medical establishment. In fact, the proportion of women among consultant physicians, the top level in the British National Health Service hospitals, rose from 19% in 1995 to 25% in 200415 and reached 28% in 2007, with over 40% of all women consultants concentrated in four specialties: anaesthetics, paediatrics, pathology, and psychiatry16. The analysis of our data in 2008, the last year of this study, showed that one-third of women compared to men physicians reached the grade of senior consultant, the top level of the PC.
The reason for the continuation of the “leaky pipeline phenomenon” in the 21st century remains unclear. One may argue that the significant lack of equity shown by our data imply that women have a lower level of training than men in hospital medicine. A lack of high profile academic due to lesser scientific output17–19 could be the reason why fewer women reach the highest positions of leadership. Women physicians tend to be more careful than men in addressing emotional issues and assessing the socio-cultural aspects that go beyond objective pathology; they spend more time on care and the promotion of a good relationship with their patients20. Therefore, women may spend less time on research than men due to the conflict in the priority of their dedication to the patient for their professional satisfaction. Thus, gender could play a role in curricular evaluation because the rules and merits helping men progress may not be as appealing or even feasible for women.
In the recent survey among 800 Catalan general practitioners a formal hierarchal position was held by 18.7% of the women compared with 33.8% of men studied. It is of note that women accounted for 8 points more than men, 28.8% versus 21.3%, while the proportion of men with a hierarchal position was higher than that of women, with no relationship with age, seniority or type of institution21.
Differences in gender values and ambitions have been suggested as reasons why fewer women than men reach the highest levels of medical positions. The predominant responsibility for child care is still borne by women and the issue of balancing career and family seems to be of paramount importance for women physicians in Europe22,23. The reason why fewer women reach the echelons of formal medical hierarchy may be due to their resignation because they do not want to assume such roles, but hardly explains the weak progress of recognition under the PC system shown by our results. Gender roles contribute to unconscious assumptions that have little to do with the actual knowledge and abilities of an individual and negatively influence decision-making when it comes to promotion.
Undoubtedly women in medicine have forged new pathways to allow physicians to balance career and family responsibilities. Medical centres have accommodated the needs of their workforce and adjusted policies to allow women to work part time. But time-to-tenure rules and family indicate that a balance between work and life must be applied to both sexes in order to promote equality of opportunity between men and women and that not penalise women in this career.
Our study had some limitations. This was conducted in one workplace and thus generalizability of the results must be cautious. We cannot exclude the possibility that a proportion of women have left the competition. Further determination of the underlying factors for the differences observed between women and men in advanced medical positions are required. Nonetheless, our study has the strength of being the first to obtain and analyse data about the advances achieved in the careers of female physicians over a period of 13 years.
In a meta-analysis Eagly24 emphasized the ability of women encouraging leadership. Women tend to demonstrate more interest than men in the personal difficulties of team members beyond the strictly occupational, which is useful to avoid interference in the workplace. Women focus their work more towards the results of the team than on their own prestige which may still be perceived as “risks” associated with any change in service delivery which could endanger the predominant medical power within the institutional model25.
Differences in work and opportunities, hierarchical and institutional support, lack of female mentor models and institutional gender bias may contribute to the slow career progression and limited visibility of medical women with respect to their male colleagues. Despite the feminization of medicine, women constitute the workforce, whereas the tasks of management and direction of the “production process” continue to be in the hands of men as occurs in the classical general social scheme.
Scarcity of women in senior positions inevitably means that their individual and collective opinions are less likely to be voiced in decision-making processes. If women in medicine are not seen to be succeeding in their careers, young women will not be motivated to achieve top careers. It has been demonstrated that political and government initiatives alone are not sufficient to advance the position of women in medicine26–28. Strategies to address gender inequality must arise from the institution: attitudes of the managers, visible commitment, provision of support during and on return from maternity leave, and, finally, encouraging women to apply for appointments and promotions.
Gender equality has an impact on the way hospital medicine follows the feminization of medicine because gender barriers are no longer accepted by women as easily as prior to the 21st century. The full potential of the increasing number of women physicians will not be achieved without continuing efforts to improve the ways in which they are educated and trained in becoming specialists and the mentoring women receive. The feminization of medicine will involve a continuous renewal of the health system that should be foreseen in human resources policies.
Editor of the articleCarmen Vives- Cases.
The number of women has increased from less than 10% of the medical students and less than 15% of physicians to being majority among new graduates in medicine and more than 40% of physicians in Western countries over the past four decades.
There is little knowledge on the advancement of women physicians in their careers due to reluctance to provide such data.
What does this study add to the literature?Whereas women among training physicians hold up to 50% permanent positions, hierarchal and intern professional promotion is significantly lower than that of men. Strategies to address gender inequality must arise from the institution.
P. Arrizabalaga conceived and designed the study, acquired the data from the Human Resources Departments in Hospital Clínic and did the data analysis and the drafting of the manuscript. R. Abellana designed the statistical analysis, collaborated in the interpretation of data with revision of the text throughout its preparation. O. Viñas and A. Merino worked on the selection of the results for publication with intellectual contributions. C. Ascaso provided the definition and usage of the femininity index, collaborated as statistical consultant and in the discussion of the results, and did the critical revision of the manuscript. All the authors have approved the final version of the manuscript.
FundingThis article was made thanks to funding from the Agència de Gestió d’Ajuts Universitaris i de Recerca (AGAUR) de la Generalitat de Catalunya, (N 2007 RDG 00008).
Conflict of interestNone declared.
The authors acknowledge the assistance of Laura Corredoira for the statistical analysis and support in the visual representation of the data, and the assistance of Mercé Viger for the PubMed search strategy.
Subsequently to the development of the study in 2013, and, after including one grade of professional career promotion, 60% of the 2-consultants and more than 82% of the Senior consultants, the two highest grades, are still men. Oral communication in “La situació professional de la dona metge a Catalunya”. June 14, 2014. Colegio Oficial de Médicos de Barcelona (book in preparation).