To describe gender differences in injection and sexual risks behaviours, and human immunodeficiency virus (HIV) and hepatitis C (HCV) prevalence among injecting drug users (IDU) in Catalonia, Spain.
MethodsCross-sectional studies in 2008–2009 (n=748) and 2010–2011 (n=597) in the network of harm reduction centres. Face to face interviews were conducted and oral fluid samples were collected to estimate HIV/HCV prevalence.
ResultsFemale were more likely than male IDU to have had a steady sexual partner (68.2% versus 44.9%), to have had an IDU steady sexual partner (46.6% versus 15.1%) and to have exchanged sex for money or drugs in the last 6 months (25.5% versus 2.3%). There were no gender differences in injecting risk behaviours. HIV prevalence was 38.7% (91/235) in women and 31.5% (347/1103) in men (p=0.031). HIV prevalence among female IDU who reported having exchange sex for money or drugs was 53.3% (32/60). The prevalence of HCV was 67.4% (159/236) and 73.6% (810/1101) in female and male IDU, respectively (p=0.053). After adjustment by immigrant status, age and years of injection, differences among HIV/HCV prevalence by gender were not significant.
ConclusionsThis study demonstrated differences in sexual risk behaviours between male and female IDU, but failed to find gender differences in injecting risk behaviours. Apart from that, the higher prevalence of HIV among women than among men, together with a lower prevalence of HCV, provides evidence that sexual transmission of HIV is important among female IDU. Additional studies are needed to analyze in-depth these specific risk factors for women in order to develop appropriate prevention and health education programs.
Describir diferencias de género en las conductas de riesgo sexual y parenteral, y en la prevalencia de los virus de la inmunodeficiencia humana (VIH) y de la hepatitis C (VHC) en los usuarios de drogas por vía parenteral (UDVP) en Cataluña.
MétodosEstudios transversales realizados en 2008-09 (n=748) y 2010-11 (n=597) en centros de reducción de daños. Se realizaron entrevistas y se recogieron muestras de fluido oral para estimar la prevalencia del VIH y del VHC.
ResultadosEn relación a las conductas sexuales de los últimos 6 meses, un mayor porcentaje de mujeres que de hombres declaró tener una pareja estable (68,2% frente a 44,9%), declaró tener una pareja estable también UDVP (46,6% frente a 15,1%) y afirmó haber mantenido relaciones sexuales comerciales (25,5% frente a 2,3%). No se observaron diferencias según género en las conductas de riesgo relacionadas con la inyección. La prevalencia global del VIH fue del 38,7% (91/235) en las mujeres y del 31,5% (347/1103) en los hombres (p=0,031), con una prevalencia del 53,3% (32/60) en las mujeres que declararon tener relaciones sexuales comerciales. La prevalencia del VHC en las mujeres fue ligeramente inferior a la observada en los hombres: 67,4% (159/236) y 73,6% (810/1101), respectivamente (p=0,053). Al ajustar por ser o no inmigrante, edad y años de inyección, las diferencias en la prevalencia de ambos virus no resultaron estadísticamente significativas.
ConclusionesEl estudio muestra diferencias de género en las conductas de riesgo sexual de los UDVP, pero no en las conductas de riesgo parenteral. Estos datos, junto con una mayor prevalencia del VIH en las mujeres y una prevalencia inferior en relación al VHC, ponen de manifiesto la relevancia de la transmisión sexual del VIH en este colectivo. Serán necesarios estudios adicionales para explorar en profundidad estos factores de riesgo específicos en las mujeres UDVP y poder desarrollar programas de prevención adaptados a sus necesidades.
Women who inject drugs have substantially different needs and face higher risk of disease and violence than do male injecting drug users (IDU).1 Regarding HIV infection, gender has emerged as an important factor in both injection related and sexual risk taking in IDU in different parts of the world, with female IDU more likely than males to take risks that may lead to HIV infection.2–5 In particular, female IDU are more likely than males to have a sexual partner who also injects drugs6–9 as well as to engage in sex for money or drugs,2,7,10 both factors previously associated with a greater risk of HIV transmission.11,12 Despite this, many harm reduction programs do not respond to the specific needs of female IDU, such as a reproductive health care. At the same time, female IDU may also encounter barriers in accessing services because of household responsibilities, lack of family support, and lack of financial resources.13
Recent available data among IDU in Europe showed a prevalence of HIV of 13.6% among men and 21.5% among women. In contrast to HIV, prevalence for hepatitis C virus (HCV) was very similar in male and female IDU: 58.1% and 56.4%, respectively.14 The contrasting findings for HIV and HCV could suggest that the large gender difference in HIV prevalence is probably due to differences in sexual risks in males and females, in line with a previous European multicenter study in which sexual behaviour emerged as the strongest predictor of HIV in this population.15
The Spanish HIV epidemic has been characterized by extremely high rates in IDU from the mid 1980s to date,16 and previous studies have pointed to a higher HIV prevalence and incidence among female than male IDU.17 Few studies in Spain have been conducted on gender differences in risk behaviour among IDU. An understanding of these differences will have major implications for designing preventive programmes and interventions. This study aims to describe gender differences in injection and sexual risks behaviours, and HIV/HCV prevalence among IDU in Catalonia (Spain).
Material and methodsStudy designAs part of the Integrated HIV/STI Surveillance System (SIVES),18 biennial bio-behavioural surveillance surveys among IDU are implemented in Catalonia. In particular, two cross-sectional studies were carried out in 2008–2009 and 2010–2011 in the network of harm reduction centres. These centres provide needle exchange programs, supervised injecting facilities, and “outreach programs” defined as an approach for contacting drug users in their local neighbourhoods and providing them with education, risk reduction counselling and the means to change their risk behaviours related to HIV. The data from both surveys were combined in order to increase the number of women IDU and to have greater statistical power.
ParticipantsAfter collecting data on the number and characteristics of clients contacted by harm reduction centres in the previous year, a convenience stratified sample of 748 and 760 IDU was selected, respectively, according to the type of centre and country of origin using proportional allocation for each study. For the purpose of the study, participants who admitted having been completed a questionnaire in the previous survey were excluded to ensure independence of samples (N=163). The total sample included in the analysis was 1345. Individuals who reported having injected in the previous six months and who attended these centres were eligible to take part. Those who agreed to participate signed the informed consent document and received 24€.
MeasuresFace to face interviews were conducted by trained interviewers using an anonymous structured questionnaire adapted from that of the World Health Organization.19 The questionnaire was translated into Spanish, Romanian, Russian, English, and French, and included questions on sociodemographic characteristics (country of origin, age, sex, education level, occupational status, where they live, in treatment for drug addiction), drug use (frequency of injection, sharing of syringes, drugs used), sexual practices (commercial sex work, use of condoms with steady and casual partners), access to free condoms, knowledge of HIV and HCV status and previous history of sexually transmitted infections (STI). The majority of questions regarding behaviour referred to the preceding 6 months.
Oral fluid samples were also taken anonymously to determine the prevalence of HIV and HCV infection. Anti-HIV antibodies were detected in oral fluid using Genscreen HIV1-2 v.2.0 from BIORAD according to the manufacturer's instructions (sensitivity=98.5%; specificity=100%)20; anti-HCV antibodies were detected using HCV 3.0 SAVe ELISA (sensitivity=86.7%; specificity=100%).21
Ethical approval was obtained from the Hospital Universitari Germans Trias i Pujol Ethics Committee. Details of the method have been reported elsewhere.22
Statistical analysisGender differences were examined using chi-square tests and the Fisher's exact test for categorical variables and the Mann–Whitney test for continuous variables. Logistic regression models were used to determine factors associated with being female after adjustment for some possible confounding factors such as the age (less than 35 or more), immigrant status (yes/no), and years of injection (less than 5 years or more). Statistical significance was set at p<0.05. The analyses were performed using SPSS version 17.
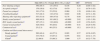
ResultsA total of 748 (17.8% women) and 597 (17.3% women) IDU were included in the analysis in 2008–2009 and 2010–2011, respectively. The main socio-demographic characteristics and patterns of drug use are presented in Table 1. Overall, female IDU were younger (median age 35 versus 36 years), less likely to be an immigrant (26.7% versus 44.5%) and to have an employment (14.5% versus 22.3%), and more likely to report living in occupied houses (squatters) (16.5% versus 10.4%) and to receive any kind of pension (28.1% versus 18.6%) compared to male. More men than women reported having injected speedball in the last 6 months (62.5% versus 45.1%).
Socio-demographic and patterns of drug use characteristics by gender.
| Male IDUn (%) | Female IDUn (%) | p-valuea | |
| Median age (IQR) | 36 (31–42) | 35 (28–42) | 0.027 |
| Immigrant | 494 (44.5) | 63 (26.7) | <0.0001 |
| Educational level: primary or less | 277 (25.1) | 52 (22.0) | 0.322 |
| Living in occupied houses (squatters)b | 115 (10.4) | 39 (16.5) | 0.007 |
| Homelessb | 263 (23.7) | 38 (16.1) | 0.011 |
| Ever in prison | 754 (68.1) | 121 (51.3) | <0.0001 |
| Employmentb | 245 (22.3) | 34 (14.5) | 0.008 |
| Receiving a pensionb,c | 205 (18.6) | 66 (28.1) | 0.001 |
| In treatment for drug addiction | 542 (48.9) | 129 (54.9) | 0.206 |
| Frequency of injection: dailyb | 546 (49.2) | 105 (44.5) | 0.186 |
| Injection of heroineb | 898 (81.3) | 185 (78.7) | 0.354 |
| Injection of cocaineb | 748 (67.8) | 159 (67.7) | 0.978 |
| Injection of speedballc | 688 (62.5) | 105 (45.1) | <0.0001 |
| Median years of injection (IQR) | 15 (7–22) | 13 (6–21) | 0.097 |
IDU, injecting drug users; IQR, interquartile range.
There were no gender differences in injecting risk behaviours in this sample. Regarding sexual risk behaviours, female were more likely than male IDU to have had a steady sexual partner (68.2% versus 44.9%), to have had an IDU steady sexual partner (46.6% versus 15.1%) and to have exchanged sex for money or drugs in the last 6 months (25.5% versus 2.3%). In contrast, the proportion of men with casual partners was higher than among women (38.6% versus 20.8%). In the last episode of sexual intercourse with a steady partner, fewer female IDU used condoms than male (27.3% versus 40.4%). After controlling for age, immigrant status and years of injection, female were more likely than male to report sexual risks behaviours such as a higher prevalence of sexual steady partners (odds ratio [OR]=2.62; 95% confidence interval [95%CI]: 1.93–3.56), IDU sexual steady partners (OR=4,85; 95%CI: 3.54–6.63), and commercial sex (OR=15,2; 95%CI: 9.14–25.2) (Table 2).
Injecting and sexual risk behaviours by gender.
| Male IDUn (%) | Female IDUn (%) | p-valuea | ORb | (95%CI) | |
| Ever sharing syringes | 550 (49.7) | 131 (55.5) | 0.104 | 0.20 | (0.89–1.62) |
| Accepted syringesc | 176 (16.0) | 42 (17.9) | 0.470 | 1.11 | (0.76–1.63) |
| Passed on syringesc | 191 (17.8) | 53 (22.9) | 0.069 | 1.29 | (0.90–1.84) |
| Front/backloadingc | 517 (48.3) | 110 (47.8) | 0.892 | 0.96 | (0.72–1.29) |
| Sharing other injecting equipmentc | 553 (51.9) | 108 (47.0) | 0.176 | 0.80 | (0.59–1.07) |
| Steady sexual partnerc | 498 (44.9) | 161 (68.2) | <0.0001 | 2.62 | (1.93–3.56) |
| IDU steady sexual partnerc | 167 (15.1) | 110 (46.6) | <0.0001 | 4.85 | (3.54–6.63) |
| Casual sexual partnerc | 428 (38.6) | 49 (20.8) | <0.0001 | 0.41 | (0.29–0.58) |
| Commercial sexc | 25 (2.3) | 60 (25.5) | <0.0001 | 15.2 | (9.14–25.2) |
| Condom usec(last sexual intercourse) | |||||
| Steady partnerd | 200 (40.4) | 44 (27.3) | 0.003 | 0.57 | (0.38–0.85) |
| Casual partnerd | 333 (78.5) | 33 (67.3) | 0.076 | 0.61 | (0.32–1.17) |
| Clientd | 22 (88.0) | 53 (88.3) | 1.000 | 1.57 | (0.32–7.78) |
IDU, injecting drug users; OR, odds ratio; 95%CI, 95% confidence interval.
Differences by gender in sexual risk behaviour were similar among immigrants than among the entire sample. Regarding injecting risk behaviours, a greater proportion of immigrant men (compared to immigrant women) reported to have practised indirect sharing (OR=0.49; 95%CI: 0.28–0.84) (Table 3).
Comparison of risk behaviours by gender among immigrants IDU (n=557).
| ImmigrantMale IDUn (%) | ImmigrantFemale IDUn (%) | p-valuea | ORb | (95%CI) | |
| Ever sharing syringes | 203 (41.2) | 31 (49.2) | 0.762 | 1.36 | (0.78–2.35) |
| Accepted syringesc | 87 (17.7) | 13 (21.0) | 0.476 | 1.01 | (0.50–2.03) |
| Passed on syringesc | 87 (18.4) | 16 (25.8) | 0.173 | 1.26 | (0.66–2.41) |
| Front/backloadingc | 234 (49.7) | 34 (54.8) | 0.645 | 1.14 | (0.66–1.96) |
| Sharing other injecting equipmentc | 267 (56.6) | 26 (41.9) | 0.029 | 0.49 | (0.28–0.84) |
| Steady sexual partnerc | 246 (49.9) | 39 (61.9) | <0.0001 | 1.46 | (0.85–2.53) |
| IDU steady sexual partnerc | 80 (16.3) | 32 (50.8) | <0.0001 | 5.00 | (2.86–8.76) |
| Casual sexual partnerc | 194 (39.3) | 13 (20.6) | 0.004 | 0.41 | (0.21–0.78) |
| Commercial sexc | 15 (3.0) | 14 (22.2) | <0.0001 | 8.92 | (4.04–19.7) |
| Condom usec(last sexual intercourse) | |||||
| Steady partnerd | 92 (37.7) | 9 (23.1) | 0.008 | 0.54 | (0.24–1.19) |
| Casual partnerd | 154 (80.6) | 8 (61.5) | 0.147 | 0.42 | (0.13–1.39) |
| Clientd | 13 (86.7) | 14 (100) | 0.483 | – | – |
IDU, injecting drug users; OR, odds ratio; 95%CI, 95% confidence interval.
The self-reported prevalence of syphilis (5.5% versus 2.5%), genital warts (13.6% versus 3.4%), herpes (3.8% versus 1.5%) and Chlamydia (3.0% versus 0.4%) was higher among women. The prevalence of HIV in oral fluid samples was higher among women than among men (38.7% vs. 31.5%, p=0.031). Contrarily, HCV prevalence was higher among male in comparison to female IDU (73.6% vs. 67.4%, p=0.05). After controlling for age, immigrant status and years of injection, female were more likely than male to self-report syphilis (OR=2.08; 95%CI: 1.02–4.25), genital warts (OR=4.04; 95%CI: 2.41–6.77), herpes (OR=2.5; 95%CI: 1.08–5.82), and Chlamydia (OR=6.9; 95%CI: 1.88–25.9) (Table 4).
Self-reported sexually transmitted infections and HCV/HIV prevalences in oral fluid samples by gender.
| Male IDUn (%) | Female IDUn (%) | p-valuea | ORb | (95%CI) | |
| Diagnosis of syphilis | 28 (2.5) | 13 (5.5) | 0.016 | 2.08 | (1.02–4.25) |
| Diagnosis of gonorrhoea | 44 (4.0) | 8 (3.4) | 0.660 | 0.78 | (0.34–1.74) |
| Diagnosis of genital warts | 37 (3.4) | 32 (13.6) | <0.0001 | 4.04 | (2.41–6.77) |
| Diagnosis of genital or anal herpes | 16 (1.5) | 9 (3.8) | 0.028 | 2.50 | (1.08–5.82) |
| Diagnosis of Chlamydia | 4 (0.4) | 7 (3.0) | 0.001 | 6.98 | (1.88–25.9) |
| Diagnosis of hepatitis B | 229 (21.1) | 46 (19.7) | 0.630 | 0.88 | (0.61–1.28) |
| HIV positive (oral fluid samples) | 810 (31.5) | 159 (38.7) | 0.031 | 1.26 | (0.92–1.72) |
| HCV positive (oral fluid samples) | 347 (73.6) | 91 (67.4) | 0.053 | 0.83 | (0.60–1.14) |
IDU, injecting drug users; OR, odds ratio; 95%CI, 95% confidence interval; HIV, human immunodeficiency virus; HCV: hepatitis C virus.
Clearly differences were seen in the prevalence of HIV among female IDU who reported having exchange sex for money or drugs compared to the other group of women (53.3% versus 33.3%) (Fig. 1).
DiscussionThis study examined gender differences in HIV risk behaviours, HIV and HCV prevalence among IDU recruited in harm reduction centres. In general, the study demonstrated differences between male and female IDU with regard to sexual risk behaviours, but failed to find differences related to injecting risk behaviours.
As in previous studies conducted in the USA, Europe and other developing and transitional countries,4,15,23 female had higher rates of sexual risk behaviours than male IDU. In particular, women were more likely than men to have an IDU steady partner and to report unprotected sex with these partners. In general among this population, studies have found that long-term relationships and involvement with a partner are not perceived as high risk.24 A recent qualitative study which explored narratives about experience of preventing sexual transmission of HIV among IDU and their sexual partners showed the level of trust and commitment to be one of the main factors for not using condoms.25
Consistent with studies in different European cities,15,26 a greater proportion of female IDU had exchanged sex for money or drugs in the last 6 months, and HIV prevalence was more than 50% among this group. These groups of women are at heightened risk of sexually acquired HIV from exposure to different sexual risk factors such as multiple sexual partners and limited condom use with them.1,27 Moreover, they are also exposed to environmental risks from the circumstances under which sex work often takes place, such as higher threats of violence and social marginalization.28,29 Harm reduction projects should be able to more effectively address sex work related vulnerabilities, taking into account that not all females who inject drugs and engage in sex work will necessarily identify as an IDU. This is particularly important where these women may not see themselves as vulnerable to particular risks because of their lack of identification with these risk groups and therefore may be left out of targeted interventions.
In contrast to differences in sexual risk behaviours between men and women, there were no differences in drug-using behaviours among the overall sample of injectors. Although some studies in New York and England have found that female IDU are more likely to share needles and equipment than male IDU,30,31 others find no association between gender and high-risk injection practices.9,32 It seems that patterns of needle sharing are often different between men and women; for example, female IDU are more likely than males to share needles with a sex partner who injects, and males with close friends.2,33,34
Gender differences in sexual risk behaviours were confirmed among the subgroup of migrant IDU, in which female IDU face a higher risk of sexual HIV infection than male IDU. In contrast, the prevalence of indirect sharing among female immigrant IDU was lower than among male immigrant IDU. Future studies about the use of drugs according to different countries of origin would be interesting for the development of educational, social, preventive and health care strategies that are culturally adapted to this heterogeneous group, in particular among women.
Another issue distinguishing between female and male IDU was the prevalence of STI. A previous survey conducted in Catalonia in a similar group of IDU confirmed the higher prevalence of STI observed in female, compared to male IDU. In particular, prevalences of Chlamydia trachomatis and/or Neisseria gonorrhoea were 6.8% and 2.0%, respectively.22 Apart from being an indicator of unprotected sex, STI are important cofactors in the transmission and acquisition of HIV infection, thus control of one may have beneficial effects on the control of the other.35 Sexual and reproductive health services should be better incorporated into harm reduction and drug treatment services.
As in previous studies conducted in Spain,14,17 HIV prevalence was higher among female IDUS. Although the higher HIV prevalence in female IDU may be explained in part by biological factors such as a greater mucous membrane exposure during sex,36 the higher HCV prevalence among male in comparison to female IDU, an infection which is not commonly transmitted sexually, confirms that sexual transmission of HIV could be relevant among female IDU. The findings are consistent with data available in other European countries from IDU mostly in drug treatment centres or other drug services.12 A recent systematic review to assess differences in HIV prevalence among female and male IDU in high seroprevalence areas showed that in the studies with a higher HIV prevalence among female compared to male, the authors suggested that sexual transmission was the reason for the difference.37 After adjustment by immigrant status, age and years of injection, differences among HIV prevalence by gender were not significant. Further analysis taking into account the influence of migration will be necessary to explore those factors that may increase HIV risk among female IDU.
The results of this study should be interpreted in light of the following limitations. This was a convenience sample of IDU from harm reduction centres, which means that results may not be generalizable to other IDU populations in Catalonia. Moreover, the study sampled IDU who accessed services at harm reduction centres (18.3% of the estimated number of IDUs who visited these centres). No information was available on the injectors that were not approached by these centres. The second limitation concerns the validity of data, since the prevalence of some risk behaviours and/or self-reported STI could be underestimated. In this sense, data collectors attempted to create an anonymous atmosphere for the interviews and used simple and understandable language. Also, research has demonstrated that self-reported risk behaviours are valid and not influenced by social desirability bias.38 In addition, although women may be underrepresented in these centres, the present study has accessed an impressive number of female IDU who tend to be a more “hidden” group than male IDU.
In conclusion, female IDU in Catalonia face gender-specific risks for HIV infection. They are more likely than their male counterparts to have a sexual partner who inject drugs and these relationships may leave the women in particularly vulnerable positions because they are dependent upon these men and are therefore potentially in a subordinate position and less capable of negotiating safe sex and injection behaviours. Interventions focusing on the sexual partnership appear to be a necessity for understanding fundamental questions of harm reduction relative to prevention, since the use of drugs is common within couples. It is common for female IDU to engage in sex work, adding a further element which increases their vulnerability to HIV infection. Taking into consideration that research suggests that the provision of enhanced harm reduction services for women can increase uptake and improve the outcomes of these interventions,13,39 gender-sensitive approaches to HIV prevention should be integrated in these centres in Catalonia, especially for those engaging in sex work. Finally, additional studies are needed to analyse in-depth these specific risk factors for women in order to develop appropriate preventive and health education programs.
Regarding HIV infection, gender has emerged as an important factor in both injection related and sexual risk taking in IDU in different parts of the world, with female IDU more likely than males to take risks that may lead to HIV infection. In Spain, previous studies have pointed to a higher HIV prevalence and incidence among female than male IDU. An understanding of these differences will have major implications for designing preventive programmes and interventions.
What does this study add to the literature?The higher prevalence of HIV and sexual risk behaviours among female IDU in relation to men, together with a lower prevalence of HCV, suggests that sexual transmission of HIV is important among this group. Prevention programs tailored to IDU should be culturally adapted and respond to the specific needs of female IDU, especially for those engaging in sex work. Sexual and reproductive health should be better incorporated into harm reduction programs.
C. Folch and J. Casabona contributed to the conception and design of the study. C. Folch analyzed the data and wrote the manuscript. A. Espelt contributed to data management. X. Majó, M.T. Brugal, and M. Meroño collaborated in the questionnaire and protocol development. M. Meroño coordinated the study implementation and data collection. V. González contributed to the laboratory analysis. C. Folch wrote the first draft of the paper, which was revised with contributions from all authors.
FundingThe study was supported by the following: Direcció General de Salut Pública, Departament de Salut, Generalitat de Catalunya; Subdirecció General de Drogodependències, Departament de Salut, Generalitat de Catalunya; Agència de Gestió d’Ajuts Universitaris i de Recerca – AGAUR (2005/SGR/00505), Departament d’Universitats, Recerca i Societat de la Informació, de la Generalitat de Catalunya; and Red de Trastornos Adictivos [RD06/0001/1018].
Conflict of interestNone.
The authors thank all interviewers, participants and the centres who have collaborated in this study: Àmbit Prevenció; SAPS, Baluard, “El Local” Sant Adrià; AEC-Gris Hospitalet/PIGAD; Asaupa’m Badalona i Santa Coloma; CAS Reus, AIDE Terrassa, Alba Terrassa, Arrels Lleida; Creu Roja Constantí, IAS Girona, CADO Vic.
REDAN Study Group: Joan Colom (Subdirecció General de Drogodependències, Departament de Salut, Generalitat de Catalunya, Barcelona); Vicenç Ausina, Elisabeth Bascuñana (Microbiology Service, Hospital Universitari Germans Trias i Pujol, Badalona, Barcelona); Alexandra Montoliu, Rafa Muñoz, Anna Esteve (CEEISCAT); Carmen Vecino (Agència de Salut Pública de Barcelona) and Anna Altabas (Àmbit Prevenció, Barcelona).