To assess the burden of several determinants on health-related quality of life (HRQOL) and to study its heterogeneity among the different Spanish regions.
MethodCross-sectional study. Data were obtained from the Spanish National Health Survey (2012), and HRQOL was measured using the EQ-5D-5L questionnaire (utility and visual analogue scale –VAS– scores). Demographic variables, physical health condition, social variables, mental health status, and lifestyle were also analysed. Tobit regression models were employed to study the relationships between expressed HRQOL and personal characteristics.
ResultsA total of 20,979 surveys were obtained. Of them, 62.4% expressed a utility score of 1, corresponding to perfect health (95%CI: 61.8%–63.2%), and 54.2% showed VAS scores ≥80 (95%CI: 53.5%–54.9%). HRQOL was mainly described as a function of age, chronic limitation in daily activities, and mental health status. Belonging to a higher-class strata and physical activity were related to better self-perceived HRQOL. Ageing worsened perceived HRQOL, but did not influence its determinants, and differences in HRQOL by regions were also not significant after model adjustment.
ConclusionHRQOL perception in the Spanish population varied slightly depending on the measure used (utilities index or VAS). Age, chronic limitations in daily life, and mental health status best explained the variability in perception, and no meaningful differences in HRQOL perception among regions were found after adjustment.
Evaluar la carga de ciertos determinantes de la calidad de vida relacionada con la salud (CVRS) y su heterogeneidad entre diferentes regiones españolas.
MétodosEstudio transversal. Utilizando datos de la Encuesta Nacional de Salud (2012), se midió la CVRS con el cuestionario EQ5D-5L (utilidad y escala visual analógica [EVA]). Se analizaron variables demográficas, estado de salud, variables sociales, salud mental y estilos de vida, utilizando modelos Tobit.
ResultadosSe incluyeron 20.979 encuestas. El 62,4% de los sujetos expresó una utilidad de 1, perfecta salud (intervalo de confianza del 95% [IC95%]: 61,8% -63,2%), y el 54,2% mostró puntuaciones en la EVA ≥80 (IC95%: 53,5%-54,9%). La CVRS se vio modificada fundamentalmente por la edad, la limitación crónica en las actividades diarias y el estado de salud mental. La clase social alta y la actividad física aparecían relacionadas con una mejor CVRS. La edad empeoró la percepción de la CVRS, pero no se asoció con un cambio en la influencia de sus determinantes. Después de ajustar los modelos, no había diferencias en la CVRS en las diferentes regiones.
ConclusiónLa percepción de la CVRS en la población española varió dependiendo de la medida utilizada (utilidades o EVA). La edad, las limitaciones crónicas en la vida diaria y el estado de salud mental explicaban fundamentalmente las diferencias en la CVRS, y las diferencias entre regiones se explicaron principalmente por diferentes características poblacionales.
Health is one of the main components of wellbeing in developed societies. World Health Organization defined health broadly about 60 years ago, but life expectancy and mortality have typically been used to define a population's state of health. As medical and public health advances have led to cures and better treatment of diseases, and thereby delayed mortality, it is logical that those who measure health outcomes will begin to assess the population's health not just on the basis of extending life expectancy, but also in terms of improving the quality of life.1 Thus, the concept of health-related quality of life (HRQOL) and its determinants has evolved over the last 40 years. Some authors have described HRQOL as the outcome of the interaction of variables across four levels: biological and psychological factors, symptoms, functioning (psychologically and socially), and general health perception.2 HRQOL has been defined as the individual's perception of their position in life in the context of the culture and value systems they live in, and in relation to their goals, expectations, standards, and concerns. It is a broad ranging concept affected in a complex way by the person's physical health, psychological state, level of independence, social relationships, and their relationship to salient features of their environment.3
Measuring HRQOL can help summarise the patient's experience of illness, and therefore characterise the social burden of chronic disease. Assessing HRQOL and its distribution across populations will help monitor our progress in achieving population health objectives, therefore contributing to reduce health inequalities between individuals, communities, and regions in our society through greater improvements in more disadvantaged communities.4 Understanding relationships among the HRQOL components will allow for designing more effective public health interventions.5
HRQOL determinants have been broadly studied. Numerous studies have demonstrated the association between physical,6 psychological,7 and social determinants and changes in HRQOL perception.8,9 Individuals with better functioning capacity, social support,10,11 socioeconomic status,12,13 and psychological condition14 display superior perception of HRQOL. Self-perceived HRQOL has also been related to lifestyle factors, such as being physically active;15,16 in contrast, it has been found to be inversely correlated with negative conditions, such as obesity.17
In the Spanish population, HRQOL has been described in detail, and differences in HRQOL by regions have been reported,18,19 although the extent of the influence of personal and environmental factors on HRQOL perception is unclear. Understanding these relationships can be of great interest in planning interventions to improve health outcomes and elucidating the reasons for certain outcomes. This study sought to identify the burden of several determinants on HRQOL, measured via the EQ-5D-5L, in the Spanish population, and to assess the potential HRQOL heterogeneity among the different Spanish regions.
MethodsDesignCross-sectional study using data from the 2011-2012 National Health Survey (NHS), whose methodology is published and described in detail.20
PopulationThe NHS was performed in 2,000 of the 35,960 sections of the 2011 Municipality Population Census, including 12 households per section area. Three-phase sampling, stratified by population size, was performed (census section, homes, and people in the home suitable for survey participation), to achieve a representative sample at a region level. The sample comprised one survey for minors and one for individuals aged >15 years.
Variables- •
Dependent variables: the selected dependent variable was perceived HRQOL. The NHS assessed quality of life using the EQ-5D-5L questionnaire, a generic survey validated for the Spanish population.21 The first part consists of 5 questions concerning the following dimensions: mobility, self-care, performance of usual life activities, pain/discomfort, and anxiety/depression. Each dimension is measured on a 5-point scale, and a single weighted score —the utility index— is obtained from these five questions. This score lies on a scale in which full health has a value of 1 and death has a value of 0, although negative values are allowed. The algorithm suggested for Spain22 was used to obtain this index. The second part consists of a visual analogue scale (EQ-VAS) ranging from 0 (poorest condition) to 100 (best possible health condition). Both the utility index and the EQ-VAS score were used as dependent variables.
- •
Independent variables: demographic data included age, sex, and the region where individuals resided. The social variables included place of birth (national/foreign), social class (which includes six categories based on occupation),23 and social support measured using the Spanish version of the Dukes-Unk11 scale.24
Three questions from the NHS were chosen to measure the capacity to perform daily activities: “Do you suffer from a chronic or long-lasting disease or problem?” (yes/no); “during the last two weeks, have any health issues forced you to stay in bed for more than half a day?” (yes/no); “in the last six months, how much have you been limited due to a health problem when performing normal daily activities?” (severely limited/mildly limited/not limited at all). The first question allowed assessment of the diagnosed chronic disease, the second determined short-term severe limitation in performing daily activities, and the third determined chronic limitation (with two stages, mild and severe).
Mental health was appraised using Goldberg's General Health Questionnaire (GHQ-12).25 This tool detects probable psychiatric morbidity. Total scores range from 0 (best mental health) to 12 (poorest mental health).
Variables related to lifestyle included smoking habit (active smoker, occasional smoker, ex-smoker, or non-smoker), alcohol consumption (measured in grams per week), body mass index ([BMI]; underweight, normal weight, overweight, or obese), and physical activity (never, occasionally, several times per month, or several times per week).
Statistical analysisThe distributions of the variables were analysed. Confidence intervals (CI) were calculated using bootstrap techniques.
Tobit regression models with upper censoring at 1.0 (or 100 for the EQ-VAS) were used to study the influence of the variables on the expressed HRQOL.26
The marginal effects of the different variables for the unconditional expected score of the HRQOL, measured at the mean values of the other covariates, were reported. These marginal effects are interpreted as the change in the HRQOL score associated with the variable in question, adjusted for the other covariates.27
Separate models were built for utility and EQ-VAS measures.
Covariates were included in the model in five groups, seeking to embrace the described multidimensional concept of HRQOL3: demographic characteristics, physical status and level of independence (chronic conditions and limitations in daily activities), social support, mental health status, and lifestyle. Specification errors and the goodness of fit of the models were examined using Akaike information criteria (AIC), Bayesian information criteria (BIC), and Cox-Snell R2. The lower the AIC and BIC or the higher the R2 scores, the better the model fitted the data.
Residuals were used to study differences in HRQOL by regions, which other studies suggested existed.19 Their intraclass correlation coefficient (ICC) was calculated to estimate how much of the residuals’ variability was related to regional aggregation.28
The best model was chosen based on its goodness of fit, its framing within the previously published literature, and the principle of parsimony. STATA 12® software was used for the analysis.
ResultsOf the 21,007 subjects aged >15 years who answered the questionnaire concerning HRQOL, 20,979 did so in a way in which utility scores could be obtained. Of these, 62.4% (95%CI: 61.8%–63.2%) expressed a utility score of 1. Of the entire sample, 20,821 subjects reported their health condition using the EQ-VAS, 54.2% of whom (95%CI: 53.5%–54.9%) reported a score of ≥80.
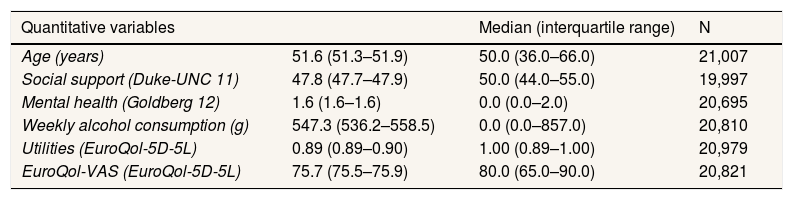
Table 1 shows the distributions of variables and the number of subjects from whom they were obtained.
Characteristics of the population aged >15 years according to the NHS.
| Quantitative variables | Median (interquartile range) | N | |
|---|---|---|---|
| Age (years) | 51.6 (51.3–51.9) | 50.0 (36.0–66.0) | 21,007 |
| Social support (Duke-UNC 11) | 47.8 (47.7–47.9) | 50.0 (44.0–55.0) | 19,997 |
| Mental health (Goldberg 12) | 1.6 (1.6–1.6) | 0.0 (0.0–2.0) | 20,695 |
| Weekly alcohol consumption (g) | 547.3 (536.2–558.5) | 0.0 (0.0–857.0) | 20,810 |
| Utilities (EuroQol-5D-5L) | 0.89 (0.89–0.90) | 1.00 (0.89–1.00) | 20,979 |
| EuroQol-VAS (EuroQol-5D-5L) | 75.7 (75.5–75.9) | 80.0 (65.0–90.0) | 20,821 |
| Qualitative variables | Percentage (95%CI) | N |
|---|---|---|
| Sex | 21,007 | |
| Woman | 54.1 (53.4–54.7) | 11,365 |
| Men | 45.9 (45.2- 46.6) | 9,642 |
| Nationality | 21,007 | |
| Spanish | 93.7 (93.4–94.0) | 19,684 |
| Non-Spanish | 6.3 (6.0- 6.6) | 1,323 |
| Chronic health condition | 20,989 | |
| Yes | 47.2 (46.5–47.9) | 9,907 |
| No | 52.8 (52.1- 53.5) | 11,082 |
| Severe short-term limitations in daily activities (previous 2 weeks) | 21,007 | |
| Yes | 12.2 (11.7–12.6) | 2,563 |
| No | 87.8 (87.4- 88.2) | 18,444 |
| Long-term limitations in daily activities (previous 6 months) | 21,000 | |
| Not limited at all | 78.5 (78.0–79.1) | 16,288 |
| Mild limitations | 17.5 (16.9–18.0) | 3,822 |
| Severe limitations | 4.0 (3.7–4.3) | 890 |
| Smoking habit | 20,894 | |
| Active smoker | 22.7 (22.1–23.2) | 4,762 |
| Occasional smoker | 2.6 (2.9) | 554 |
| Ex-smoker | 19.9 (19.4–20.5) | 4,181 |
| Nonsmoker | 54.7 (54.1–55.4) | 11,487 |
| Physical activity | 20,991 | |
| Never | 44.7 (44.1– 45.4) | 9,390 |
| Occasionally | 36.1 (35.5–36.8) | 7,585 |
| Several times per month | 11.1 (10.6–11.4) | 2,321 |
| Several times per week | 8.1 (7.7–8.4) | 1,695 |
| Body mass index | 19,069 | |
| Underweight | 2.0 (1.8–2.1) | 375 |
| Normal weight | 42.9 (42.2–43.6) | 8,176 |
| Overweight | 37.6 (36.9–38.3) | 7,171 |
| Obese | 17.6 (17.0–18.1) | 3,347 |
| Social class | 20,246 | |
| I. Manager, director | 10.6 (10.2–11.0) | 2,143 |
| II. Intermediate positions | 7.7 (7.4–8.1) | 1,569 |
| III. Skilled nonmanual worker | 18.7 (18.2–19.2) | 3,785 |
| IVa. Skilled manual worker | 14.7 (14.2–15.2) | 2,986 |
| IVb. Partially skilled manual worker | 3.3 (3.2–3.4) | 6,711 |
| V. Unskilled manual worker | 15.1 (14.6–15.6) | 3,052 |
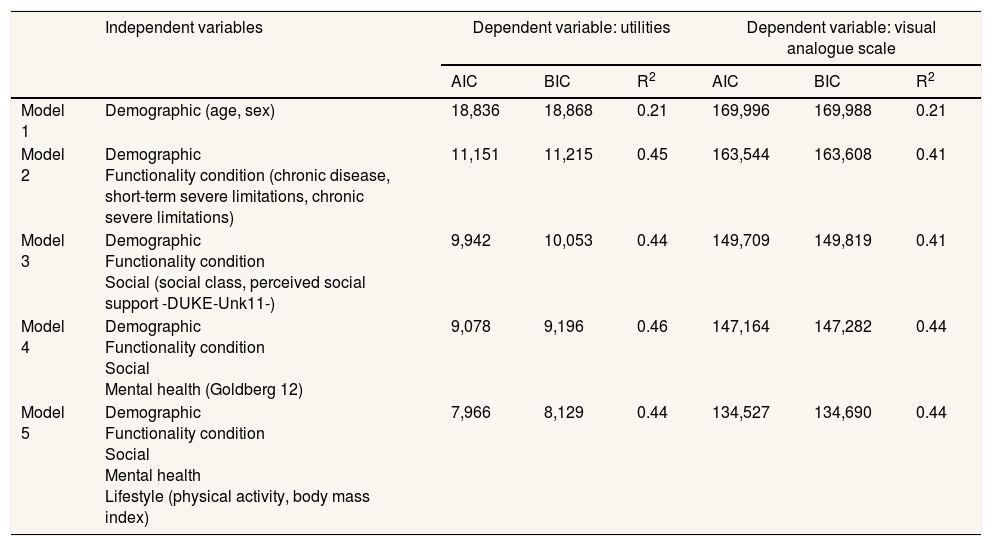
Table 2 shows how the incorporation of additional covariates improved the fit of the models to the HRQOL data. Demographic variables contributed significantly to explaining the variability in responses, and so did disease-related variables. Social variables were strongly correlated with HRQOL perception but did not improve the model, and even reduced the R2. The variable accounting for mental health improved the model adjustment. Variables related to lifestyle (physical activity and BMI) were also associated with HRQOL, but did not improve the global capacity of the model. Alcohol consumption and smoking habit were not included in model 5, since their coefficients were negligible and worsened the model's fit.
Goodness of fit of several models to explain the variability of perceived health related quality of life.
| Independent variables | Dependent variable: utilities | Dependent variable: visual analogue scale | |||||
|---|---|---|---|---|---|---|---|
| AIC | BIC | R2 | AIC | BIC | R2 | ||
| Model 1 | Demographic (age, sex) | 18,836 | 18,868 | 0.21 | 169,996 | 169,988 | 0.21 |
| Model 2 | Demographic Functionality condition (chronic disease, short-term severe limitations, chronic severe limitations) | 11,151 | 11,215 | 0.45 | 163,544 | 163,608 | 0.41 |
| Model 3 | Demographic Functionality condition Social (social class, perceived social support -DUKE-Unk11-) | 9,942 | 10,053 | 0.44 | 149,709 | 149,819 | 0.41 |
| Model 4 | Demographic Functionality condition Social Mental health (Goldberg 12) | 9,078 | 9,196 | 0.46 | 147,164 | 147,282 | 0.44 |
| Model 5 | Demographic Functionality condition Social Mental health Lifestyle (physical activity, body mass index) | 7,966 | 8,129 | 0.44 | 134,527 | 134,690 | 0.44 |
AIC: Akaike information criteria; BIC: Bayes information criteria; R2: Cox-Snell R2.
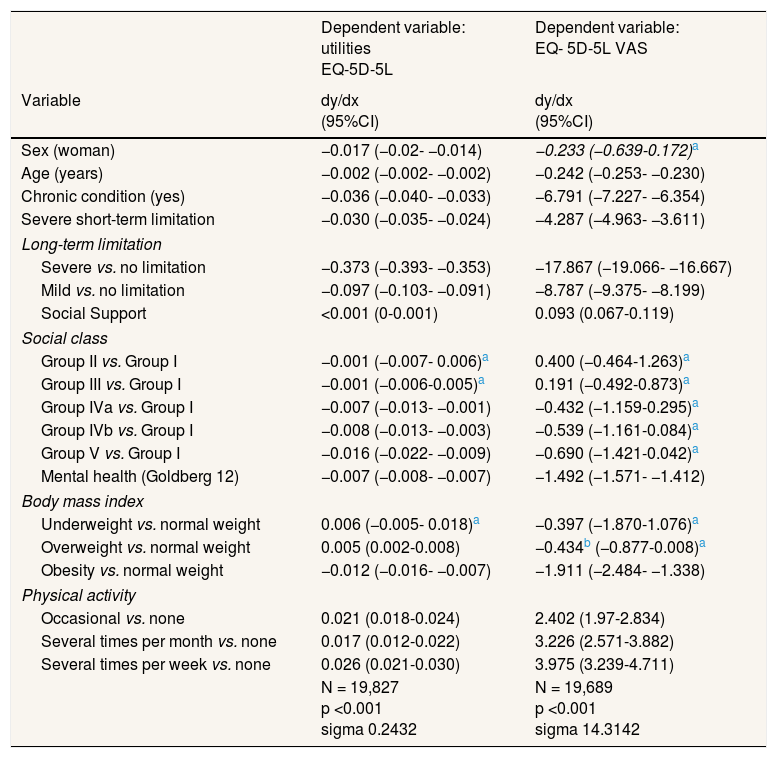
In Table 3, the best models are shown in detail. Female sex was associated with a reduction in HRQOL measured in utilities (−0.017 points). Each 10-year increase in age was associated with a decrease of 0.020 points in utilities, and 2.420 points on the EQ-VAS. Age squared coefficients were tested in the model, but did not achieve a better fit.
Marginal effects for the unconditional expected value of the HRQOL score.
| Dependent variable: utilities EQ-5D-5L | Dependent variable: EQ- 5D-5L VAS | |
|---|---|---|
| Variable | dy/dx (95%CI) | dy/dx (95%CI) |
| Sex (woman) | −0.017 (−0.02- −0.014) | −0.233 (−0.639-0.172)a |
| Age (years) | −0.002 (−0.002- −0.002) | −0.242 (−0.253- −0.230) |
| Chronic condition (yes) | −0.036 (−0.040- −0.033) | −6.791 (−7.227- −6.354) |
| Severe short-term limitation | −0.030 (−0.035- −0.024) | −4.287 (−4.963- −3.611) |
| Long-term limitation | ||
| Severe vs. no limitation | −0.373 (−0.393- −0.353) | −17.867 (−19.066- −16.667) |
| Mild vs. no limitation | −0.097 (−0.103- −0.091) | −8.787 (−9.375- −8.199) |
| Social Support | <0.001 (0-0.001) | 0.093 (0.067-0.119) |
| Social class | ||
| Group II vs. Group I | −0.001 (−0.007- 0.006)a | 0.400 (−0.464-1.263)a |
| Group III vs. Group I | −0.001 (−0.006-0.005)a | 0.191 (−0.492-0.873)a |
| Group IVa vs. Group I | −0.007 (−0.013- −0.001) | −0.432 (−1.159-0.295)a |
| Group IVb vs. Group I | −0.008 (−0.013- −0.003) | −0.539 (−1.161-0.084)a |
| Group V vs. Group I | −0.016 (−0.022- −0.009) | −0.690 (−1.421-0.042)a |
| Mental health (Goldberg 12) | −0.007 (−0.008- −0.007) | −1.492 (−1.571- −1.412) |
| Body mass index | ||
| Underweight vs. normal weight | 0.006 (−0.005- 0.018)a | −0.397 (−1.870-1.076)a |
| Overweight vs. normal weight | 0.005 (0.002-0.008) | −0.434b (−0.877-0.008)a |
| Obesity vs. normal weight | −0.012 (−0.016- −0.007) | −1.911 (−2.484- −1.338) |
| Physical activity | ||
| Occasional vs. none | 0.021 (0.018-0.024) | 2.402 (1.97-2.834) |
| Several times per month vs. none | 0.017 (0.012-0.022) | 3.226 (2.571-3.882) |
| Several times per week vs. none | 0.026 (0.021-0.030) | 3.975 (3.239-4.711) |
| N = 19,827 p <0.001 sigma 0.2432 | N = 19,689 p <0.001 sigma 14.3142 | |
95%CI: 95% confidence interval.
Experiencing a chronic condition, severe limitations for the preceding 2 weeks, and chronic limitation for the preceding 6 months were also associated with a perception of poorer quality of life, with severe limitations experienced for the preceding 6 months exerting the greatest effect. These limitations caused average reductions of 0.373 points in utilities and 17.867 points on the EQ-VAS.
Disadvantaged social classes were associated with poorer perceived HRQOL, measured using both the utility index and the EQ-VAS, and a gradient was observed indicating that the lower the social class, the poorer the HRQOL reported. Differences of 0.016 points in utilities were observed between social classes I and VI. Similarly, every two standard deviations (15.0 points) increase in the social support score was related to a decrease of 0.003 points in utilities and 1.397 points on the EQ-VAS.
The association between Goldberg's test score and HRQOL was negative. Every two standard deviations (5.52 points) increase in Goldberg's score was associated with a decrease of 0.041 points in utilities and 8.234 points on the EQ-VAS. The relationship between BMI and HRQOL was only evident when comparing obesity with normal weight (−0.012 points in utilities and −1.911 on the EQ-VAS). Physical activity was related with improved HRQOL. Individuals who engaged in physical activity several times per week had increases of 0.026 points in utilities and 3.975 points on the EQ-VAS compared to those not performing any physical activity.
Models for subjects older and younger than 50 years of age were built, but no significant differences were observed between their coefficients; therefore, only general models are presented.
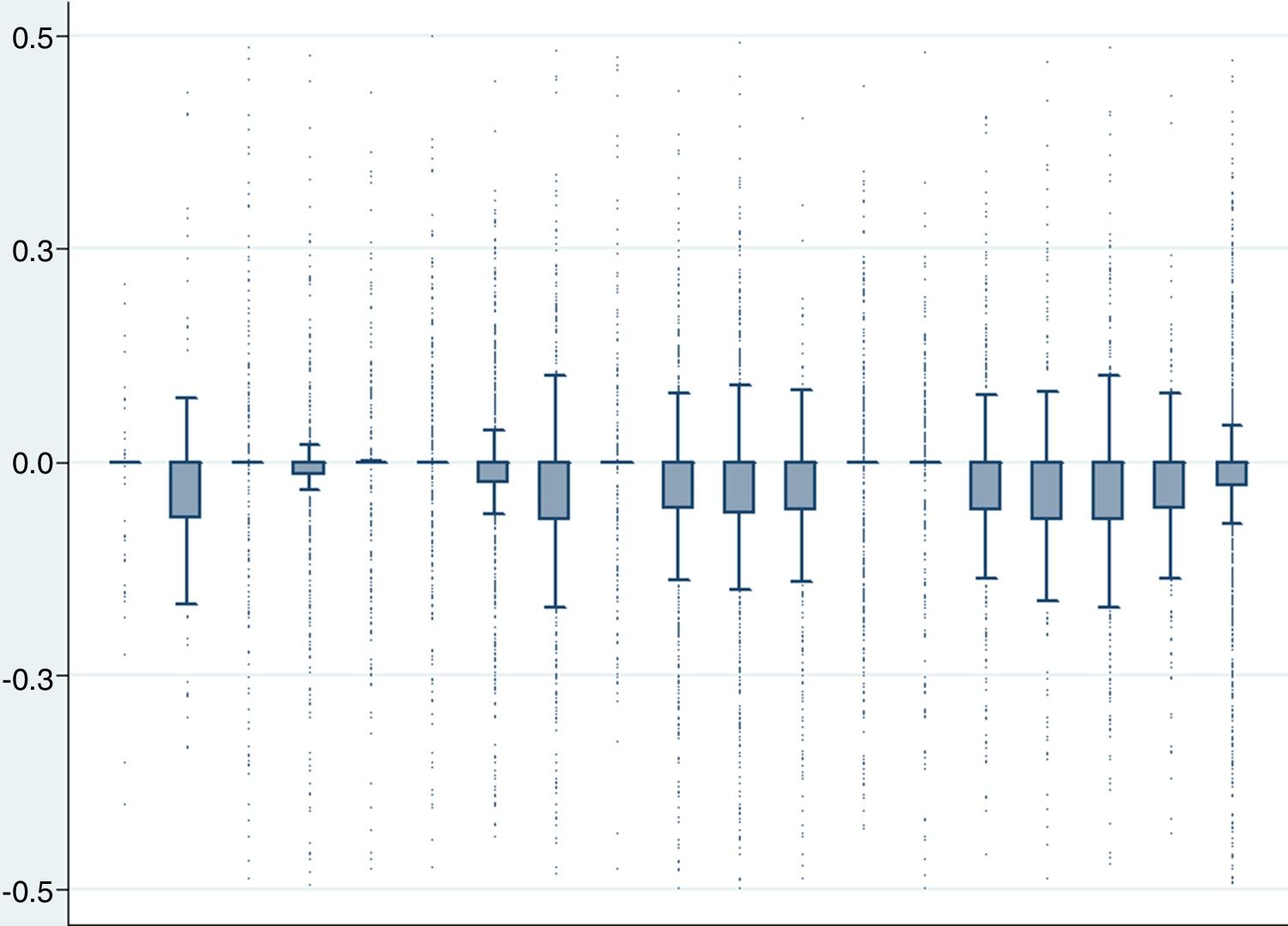
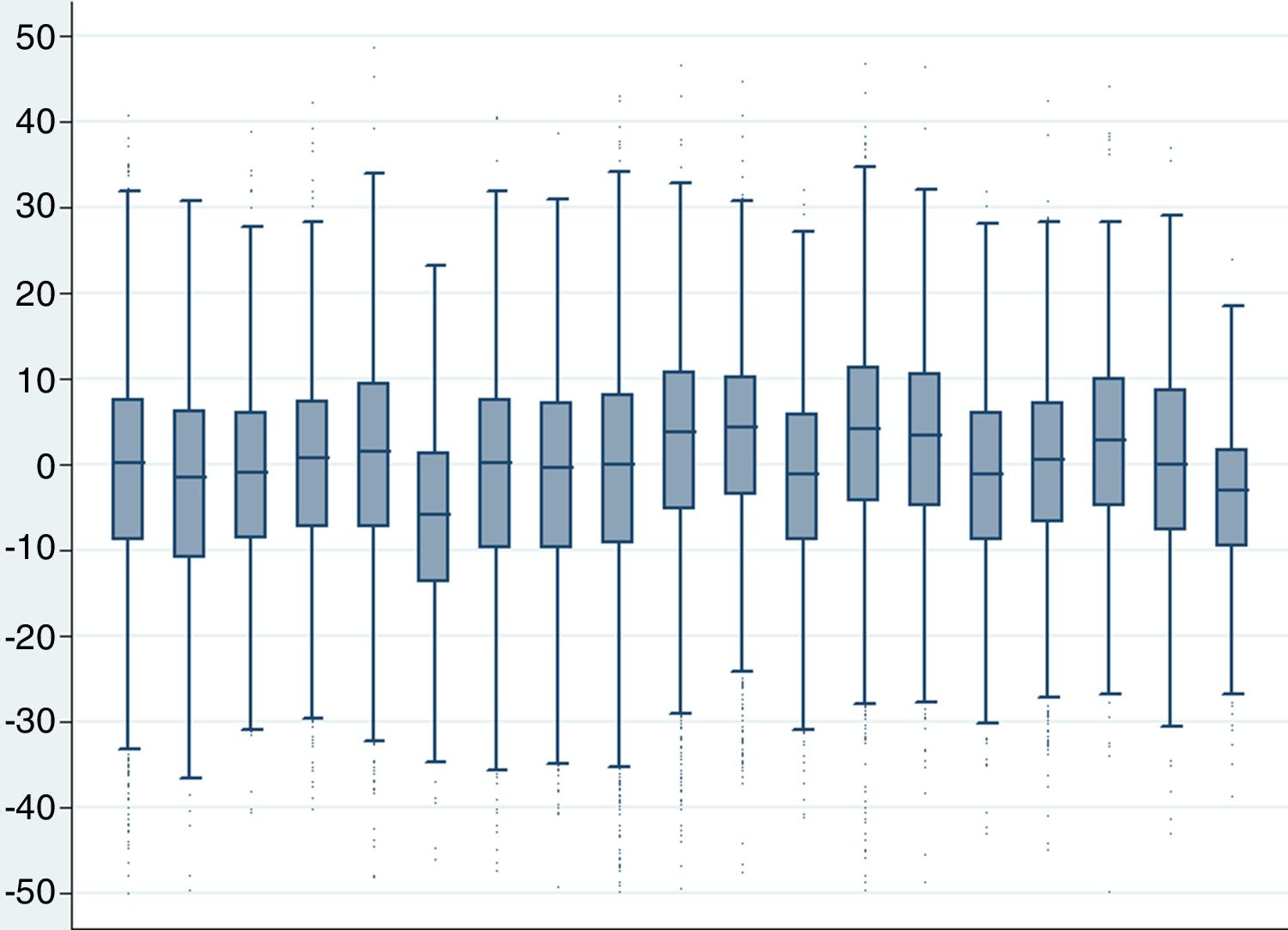
Figure 1 shows the distribution of the gross residuals for the utility values in each region (the non-explained variability). Figure 2 shows the residuals for the EQ-VAS model. No significant differences were found between different regions once the adjusted predicted values were subtracted from the expressed values. The ICC was 0.004 for the utility residuals and 0.020 for the EQ-VAS score residuals, which implies that 0.4% and 2%, respectively, of the variability of the residuals was due to the effect of regional aggregation.
HRQOL perception in the Spanish population varied slightly depending on the measure used (utility index or EQ-VAS). HRQOL was strongly related to age, mental health, and the presence of limitations in daily life activities, particularly in the case of long-term limitations. Social class was positively correlated with HRQOL, as were certain health behaviours such as being physically active or maintaining a normal weight. These results are not surprising as these factors have been found to be related to HRQOL in other studies;11,14,29 however, the way in which emotions, mental distress, social problems, and physical illness are perceived, experienced, and expressed are dependent on culture and environment.30 Therefore, we found it valuable to study the distribution and relative weight of determinants of HRQOL in the Spanish population in a comprehensive way. Additionally, the findings suggest that previously reported differences in HRQOL by regions were due to differences in the population characteristics rather than contextual effects.
Sociodemographic characteristics, especially ageing, were strongly related to HRQOL, although health expectations have been hypothesised to be readjusted throughout life.31 Contrary to other studies,32 we did not find differences in the factors that impact HRQOL between people under or over 50 years of age, suggesting that ageing worsened perceived HRQOL, but did not influence its determinants. Previously observed differences in HRQOL33 by sex were only noted when utility indexes were used, and could be influenced by social determinants and lifestyle, particularly in older individuals.34
Variables related to social class12,13 and social support10,11 have been shown to greatly influence differences in HRQOL. It has been reported that more generous welfare regimes experience lesser socioeconomic inequalities in their quality of life.9 Hence the relative importance of social class and how one's perception of social support is associated with perceived HRQOL, which could be studied in future research in the context of our welfare system's strength.
The influence of factors related to chronic disease in explaining HRQOL is well known,35 but this study emphasizes the role of perceived limitations to shape the relationship between disease and HRQOL,6 and the findings suggest that interventions addressing limitations can provide significant health benefits.36
Mental health condition has been found to have a strong association with reported HRQOL.14 The negative effect of a poor mental condition on the individual's HRQOL has been previously reported in the Spanish population, suggesting the need for global policies aimed at reducing this burden.7 These results highlight the fact that mental health status can be as relevant as age and chronic limitations in explaining differences in reported HRQOL in the Spanish population.
Regarding the role of health-related behaviours, alcohol and tobacco consumption did not showed a clear association with reported HRQOL. The relationship between alcohol consumption and HRQOL has been difficult to model,37 and smoking has been related to a worse perception of HRQOL,38 but it is possible that people with poorer health are recommended to cease these habits; therefore, expected associations are spurious or do not occur. Better HRQOL was observed in those who referred any physical activity in their leisure time as opposed to those with no physical activity, after adjusting for other determinants of HRQOL, which is relevant because moderate increase of physical activity has been shown to produce improvements in HRQOL.39
Obesity has been described as a factor associated with higher morbidity and poorer HRQOL.17 In this study, overweight subjects showed a slightly higher HRQOL than normal weight subjects, measured by utility score but not when using the VAS scale. Robust differences in HRQOL were only found between obese and normal-weight subjects, as other studies reported.40
Research on health-related contextual effects has been performed, maybe spurred by an increasing interest in macro-social influences on the individual's health status. The research has mainly focused on the relationship between spatially concentrated deprivation and health, but empirical findings are controversial and depend on the studied aggregation level.41 Significant differences in expressed HRQOL by regions has been described in Spain,19 as well as in other countries.11,42,43 Differences in the effect of context on HRQOL have also been reported in the Spanish population.29 In contrast to these works, we studied a larger body of variables related to HRQOL, such as social class and, perhaps even more importantly, perceived limitations, which yielded negligible differences among regions. This suggests that differences could mainly be due to compositional differences among region populations rather than contextual effects, which could explain the differences in reported HRQOL. As with other studies, the relatively large size of the included administrative area can hinder the detection of any significant contextual effect related to HRQOL at those regional levels,44 but these findings are relevant in the Spanish health setting since services are designed at that specific level. Reported differences in HRQOL could lead to change normative values of HRQOL tests,42 or to strengthen public health policies in disadvantaged regions 43. In Spain, interventions to improve HRQOL should be tailored for different target populations according to age, impairment, mental health status, or social class, but not different regions.
This study was subject to design limitations. First, its cross-sectional design limits the possibility to establish causal relationships. Therefore, the absence of an association between tobacco or alcohol consumption and HRQOL could be a consequence of disease or the actions of health agents. Another limitation is that some data were self-reported, and a certain bias of indulgence might be present. Additionally, tariffs for EQ-5D-5L were estimated from the cross-walk index from the Spanish tariffs, an approach with several limitations, like placing an artificial floor effect on the values of the 5L, when the EQ-5D-3L is used for comparison.22 On the other hand, there is a current debate on whether censoring regression methods are appropriate to make estimations over the censored part of the variables, as previous anchor measures for the utilities and VAS should not be used.45
Regarding the strengths of the study, the survey methodology poses the best approximation of the Spanish population's health at present, and the methodology used in the analysis fits the particularity of the sampling method.
This study has several implications. It must be noted that when assessing the effect of a disease on HRQOL in the Spanish population, its impact is better explained by the impairment or emotional burden rather than the presence of the disease itself. Hence, interventions to improve HRQOL must act on the components that result in limitations in daily activities and the agents that affect mental health, a valid approach for any age range. Promoting physical activity, especially for those who do not engage in leisure physical activity, and interventions aimed at preventing obesity could also be helpful for the maintenance of good HRQOL perception. On the other hand, HRQOL can be a useful measure to identify health inequalities among individuals and communities, and this study highlights the importance of taking social class into consideration when public health interventions are being planned. However, in order to study differences in HRQOL by regions, identifying compositional effects is necessary before attributing these differences to contextual covariates.
In summary, and given the relevance of HRQOL for a population's health, the findings of this study can allow for identifying subgroups which should be specifically targeted, like the elderly or those belonging to the least favoured classes, and to set priorities for effective public health interventions, especially promoting physical activity or healthy ageing, early interventions to limit impairment or chronic conditions, and mental health strategies.
Association between physical, psychological, and social determinants and changes in HRQOL perception is well established. Nevertheless, it is no clear enough the weight of each component of these associations and if there are differences among regions in Spain.
What does this study add to the literature?Age, chronic limitations, and mental health best explained the variability in HRQOL. In Spain, interventions to improve HRQOL could be targeted for different populations defined by age, chronic limitations to perform daily activities, mental health status or social class, but not for different regions as compositional rather than contextual effects explained HRQOL differences.
Maria-Victoria Zunzunegui.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsJ. Martín-Fernández, I. del Cura-González and A. Sarria-Santamera conceived the idea and designed the study. J. Martín-Fernández and I. del Cura-González got the cleaned and annotated database. J. Martín-Fernández, G. Ariza-Cardiel, E. Polentinos-Castro and T. Sanz-Cuesta developed the statistical analysis and discussed the preliminary results. J. Martín-Fernández, G. Ariza-Cardiel, E. Polentinos-Castro, T. Sanz-Cuesta, A. Sarria-Santamera and I. del Cura-González studied the meaning of the results and their health policy implications. All authors have discussed and approved the submitted manuscript.
FundingThis manuscript has been translated and edited with the support of ISCIII and FEDER Funds, Grant Number RD12/0001/0012. Publication charges have been supported by ISCIII, grant Number 1300648.
Conflicts of interestNone.
We thank Caroline Vass, Research Fellow in Manchester Centre for Health Economics, for her comments, which helped us to improve the manuscript.