The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoThis study aimed to evaluate the health care quality among insured patients hospitalized in the Indonesian mother and child hospital.
MethodA secondary data analysis was performed to evaluate the health care services received by the insured patients hospitalized in the Indonesian mother and child hospital. Data were extracted from the BPJS health insurance e-claim database from January 1 to December 31, 2019 and from January 1 to June 30, 2020. A descriptive and bivariate analysis were used to examine total patients and hospital admissions; INACBGs diagnoses, procedures by severity; types of inpatient wards; length of stay; discharge status; hospital costs; and 30-day readmissions.
ResultsTotal inpatient unit admissions were 2870 in 2019 and 1533 in 2020. From total hospital admissions in 2019 and 2020, over 50% were admitted to the 3rd class of inpatient units, less than 10% had length of stays more than 5 days, and over 98% were discharged based on physician approval. However, hospital readmissions were also found for about 20.1% in 2019 and 2.9% in 2020 and about 42.9% in 2019 and 61.3% in 2020 were found causing hospital financial losses. Older patients, longer hospital stays, inpatient ward class 1 & 2, high hospital tariff, inadequate clinical pathway implementation, lack of interprofessional collaboration, and ineffective nurse manager supervision were identified as contributing factors to the hospital financial losses.
ConclusionIntegrated clinical pathways with interprofessional collaboration that are implemented through professional nursing practice model are suggested for health care quality improvement.
Hospitals as the health care facilities are obliged to provide excellent health care quality that is safe, effective, patient-centred, timely, efficient, and equitable.1–3 Likewise, the Indonesian Hospital Accreditation Committee also requires all hospitals to deliver health care services focusing on patient-centred and safety.4 To enhance the health care quality at the Indonesian hospitals, since 2011 the Hospital Accreditation Committee had developed the national standard for hospital accreditation that has been integrated with the principles for health care standards set by the International Society for Quality in Health Care (ISQua).4,5 This national standard was then used by health care providers as the guideline for them to deliver health care services and utilized by the hospital accreditation surveyors as the benchmark to assess the actual work of health care providers.4
In line with the Hospital Accreditation Committee, since 2014 the national health insurance of Indonesia called as Badan Penyelenggara Jaminan Sosial (BPJS) had also implemented the case-based payment system (prospective payment system), which determining health care tariff rates based on the Indonesian Case Base Groups (INA-CBGs). The INA-CBG implementation aimed at controlling health care costs, providing an excellent standard care, avoiding unnecessary health services, facilitating reimbursement for every claim, and supporting cost containment.
Today, it has been six years since the INA-CBGs payment system initially applied in Indonesian hospitals. However, assessment of health care quality among insured patients in Indonesian hospital during the implementation of INS-CBGs payment system had not been conducted yet. Hence, the purpose of this study was to evaluate health care quality among insured patients, especially in the Indonesian mother and child hospital.
MethodStudy design and data sourcesA longitudinal, secondary data analysis was used in this study to address the research aim. This study used patient data from the 2019–2020 BPJS health insurance e-claim databases of one of mother and child hospitals located in Makassar city, South Sulawesi, Indonesia.
Setting and sampleThe study site was a 66-bed mother and child hospital owned by the government of South Sulawesi Province. Inclusion criteria for the sample were all insured patients hospitalized in inpatient units and had been discharged from January 1 to December 31, 2019 and from January 1 to June 30, 2020. A total of 2870 inpatient ward admissions in 2019 and 1533 inpatient ward admissions in 2020 were included in this study.
Study measuresStudy measures were categorized into three concepts: structure, process, and outcomes. Structure consists of patient characteristics (sex & age); types of inpatient wards (1st, 2nd, and 3rd class) and hospital admission categories (index admission & readmission). Meanwhile process comprises INACBGs diagnoses & procedures by severity; and length of hospital stays (1–3, 4–5, 6–9, and ≥10 days). Finally, outcomes encompass discharge status (physician approval, patient referred, patient request, patient died, and others); hospital costs (financial loss & profit); and 30-day hospital readmissions (readmitted once, twice, and ≥3 times).
Ethical considerationsEthical approval was obtained from the Research Ethics Committee for Health Sciences Research, Faculty of Medicine, Hasanuddin University (Number 376/UN4.6.4.5.31/PP36/2020) prior to data collection from the BPJS health insurance e-claim database at the Indonesian mother & child hospital, located in Makassar, South Sulawesi, Indonesia.
Data analysisA univariate and bivariate analysis were used to examine variables of structure, process, and outcomes. Descriptive statistics including means (M), standard deviations (SD), frequencies (n), and percentage (%) were calculated to describe the patient characteristics; hospital admission categories; types of inpatient wards; INACBGs diagnoses & procedures by severity; length of hospital stays; discharge status; hospital costs; and 30-day hospital readmissions. Meanwhile bivariate analysis, i.e., one-way ANOVA, was used to examine differences in hospital costs based on age, types of inpatient wards, and length of hospital stays.
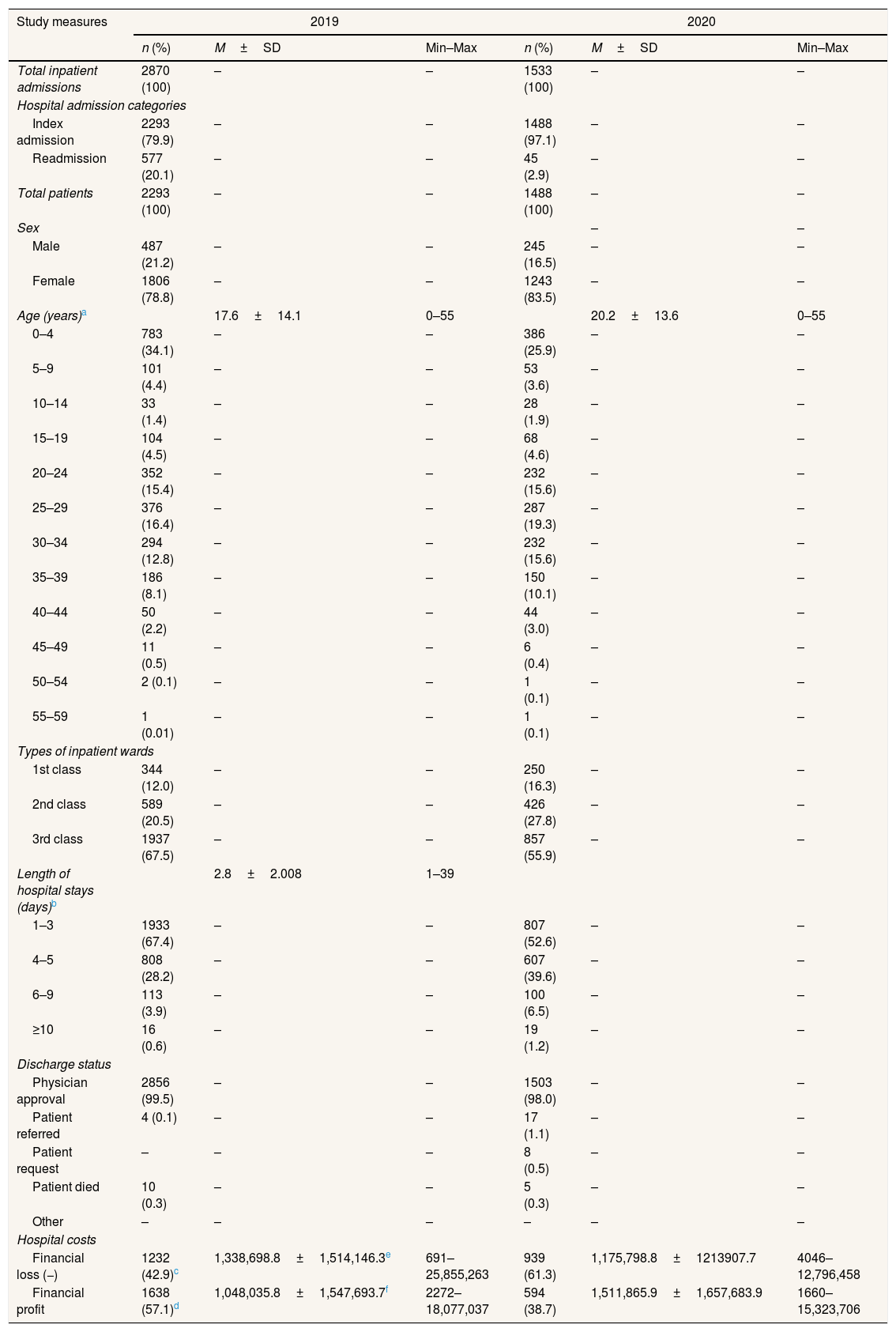
ResultsAs shown in Table 1, there were 2870 inpatient admissions in 2019 and 1533 inpatient admissions in 2020, extracted from the BPJS health insurance e-claim database of the Indonesian mother and child hospital. Of those inpatient admissions, 79.9% (2019) and 97.1% (2020) were index admissions and 20.1% (2019) and 2.9% (2020) were readmissions. Majority patients were females, 78.8% (2019) versus 83.5% (2020), and dominated by patients aged 0–4 years, 34.1% (2019) versus 25.9% (2020). More than half of the total admissions in the year of 2019 and 2020 were hospitalized for 1–3 days at the 3rd class of inpatient wards and most of them were discharged with the physician approval. However, of the total inpatient admissions, 42.9% in 2019 and 61.3% in 2020 caused financial losses on average of IDR 1,338,698.8 per admission in 2019 and IDR 1,175,798.8 per admission in 2020.
Distribution of total inpatient admissions & patients, sex, age, hospital admission categories, types of inpatient wards, length of hospital stays, discharge status, and hospital costs during 2019–2020.
| Study measures | 2019 | 2020 | ||||
|---|---|---|---|---|---|---|
| n (%) | M±SD | Min–Max | n (%) | M±SD | Min–Max | |
| Total inpatient admissions | 2870 (100) | – | – | 1533 (100) | – | – |
| Hospital admission categories | ||||||
| Index admission | 2293 (79.9) | – | – | 1488 (97.1) | – | – |
| Readmission | 577 (20.1) | – | – | 45 (2.9) | – | – |
| Total patients | 2293 (100) | – | – | 1488 (100) | – | – |
| Sex | – | – | ||||
| Male | 487 (21.2) | – | – | 245 (16.5) | – | – |
| Female | 1806 (78.8) | – | – | 1243 (83.5) | – | – |
| Age (years)a | 17.6±14.1 | 0–55 | 20.2±13.6 | 0–55 | ||
| 0–4 | 783 (34.1) | – | – | 386 (25.9) | – | – |
| 5–9 | 101 (4.4) | – | – | 53 (3.6) | – | – |
| 10–14 | 33 (1.4) | – | – | 28 (1.9) | – | – |
| 15–19 | 104 (4.5) | – | – | 68 (4.6) | – | – |
| 20–24 | 352 (15.4) | – | – | 232 (15.6) | – | – |
| 25–29 | 376 (16.4) | – | – | 287 (19.3) | – | – |
| 30–34 | 294 (12.8) | – | – | 232 (15.6) | – | – |
| 35–39 | 186 (8.1) | – | – | 150 (10.1) | – | – |
| 40–44 | 50 (2.2) | – | – | 44 (3.0) | – | – |
| 45–49 | 11 (0.5) | – | – | 6 (0.4) | – | – |
| 50–54 | 2 (0.1) | – | – | 1 (0.1) | – | – |
| 55–59 | 1 (0.01) | – | – | 1 (0.1) | – | – |
| Types of inpatient wards | ||||||
| 1st class | 344 (12.0) | – | – | 250 (16.3) | – | – |
| 2nd class | 589 (20.5) | – | – | 426 (27.8) | – | – |
| 3rd class | 1937 (67.5) | – | – | 857 (55.9) | – | – |
| Length of hospital stays (days)b | 2.8±2.008 | 1–39 | ||||
| 1–3 | 1933 (67.4) | – | – | 807 (52.6) | – | – |
| 4–5 | 808 (28.2) | – | – | 607 (39.6) | – | – |
| 6–9 | 113 (3.9) | – | – | 100 (6.5) | – | – |
| ≥10 | 16 (0.6) | – | – | 19 (1.2) | – | – |
| Discharge status | ||||||
| Physician approval | 2856 (99.5) | – | – | 1503 (98.0) | – | – |
| Patient referred | 4 (0.1) | – | – | 17 (1.1) | – | – |
| Patient request | – | – | – | 8 (0.5) | – | – |
| Patient died | 10 (0.3) | – | – | 5 (0.3) | – | – |
| Other | – | – | – | – | – | – |
| Hospital costs | ||||||
| Financial loss (−) | 1232 (42.9)c | 1,338,698.8±1,514,146.3e | 691–25,855,263 | 939 (61.3) | 1,175,798.8±1213907.7 | 4046–12,796,458 |
| Financial profit | 1638 (57.1)d | 1,048,035.8±1,547,693.7f | 2272–18,077,037 | 594 (38.7) | 1,511,865.9±1,657,683.9 | 1660–15,323,706 |
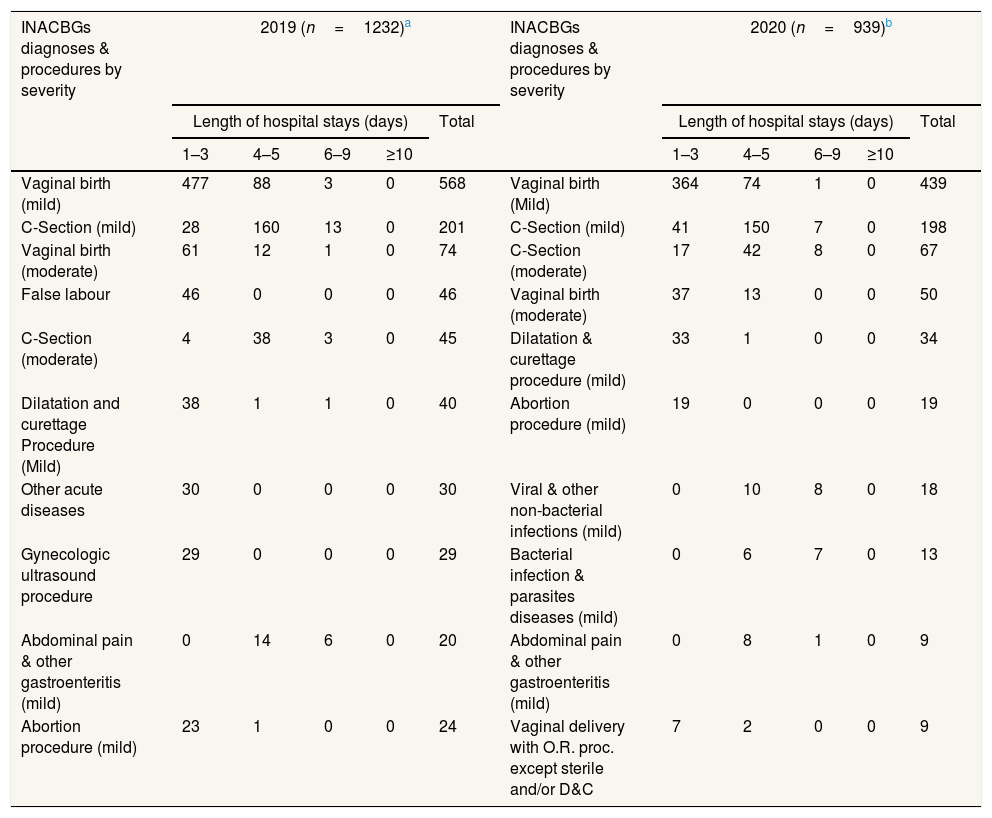
Table 2 depicts top 10 of the INACBGs diagnoses & procedures by severity that caused financial losses among insured patients hospitalized in the Indonesian mother and child hospital in the period of 2019 and 2020. As clearly seen in Table 2; vaginal birth (mild & moderate), C-section (mild & moderate), dilatation & curettage (mild), and abortion (mild) were procedures by severity that found high volume, risks, and costs during the year of 2019 and 2020. Meanwhile, abdominal pain & other gastroenteritis (mild), and viral/bacterial/non-bacterial infections (mild) as well as parasite diseases (mild) were identified as INACBGs diagnoses that were high volume, risks, and costs in the year of 2019 and 2020. These INACBGs diagnoses and procedures caused the patients hospitalized for more than 3 days and up to 9 days at the hospital, leading to financial losses.
Top 10 high volume, high risk, and high cost of INACBGs diagnoses & procedures by severity among insured patients hospitalized in the indonesian mother & child hospital in the year of 2019 & 2020.
| INACBGs diagnoses & procedures by severity | 2019 (n=1232)a | INACBGs diagnoses & procedures by severity | 2020 (n=939)b | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Length of hospital stays (days) | Total | Length of hospital stays (days) | Total | ||||||||
| 1–3 | 4–5 | 6–9 | ≥10 | 1–3 | 4–5 | 6–9 | ≥10 | ||||
| Vaginal birth (mild) | 477 | 88 | 3 | 0 | 568 | Vaginal birth (Mild) | 364 | 74 | 1 | 0 | 439 |
| C-Section (mild) | 28 | 160 | 13 | 0 | 201 | C-Section (mild) | 41 | 150 | 7 | 0 | 198 |
| Vaginal birth (moderate) | 61 | 12 | 1 | 0 | 74 | C-Section (moderate) | 17 | 42 | 8 | 0 | 67 |
| False labour | 46 | 0 | 0 | 0 | 46 | Vaginal birth (moderate) | 37 | 13 | 0 | 0 | 50 |
| C-Section (moderate) | 4 | 38 | 3 | 0 | 45 | Dilatation & curettage procedure (mild) | 33 | 1 | 0 | 0 | 34 |
| Dilatation and curettage Procedure (Mild) | 38 | 1 | 1 | 0 | 40 | Abortion procedure (mild) | 19 | 0 | 0 | 0 | 19 |
| Other acute diseases | 30 | 0 | 0 | 0 | 30 | Viral & other non-bacterial infections (mild) | 0 | 10 | 8 | 0 | 18 |
| Gynecologic ultrasound procedure | 29 | 0 | 0 | 0 | 29 | Bacterial infection & parasites diseases (mild) | 0 | 6 | 7 | 0 | 13 |
| Abdominal pain & other gastroenteritis (mild) | 0 | 14 | 6 | 0 | 20 | Abdominal pain & other gastroenteritis (mild) | 0 | 8 | 1 | 0 | 9 |
| Abortion procedure (mild) | 23 | 1 | 0 | 0 | 24 | Vaginal delivery with O.R. proc. except sterile and/or D&C | 7 | 2 | 0 | 0 | 9 |
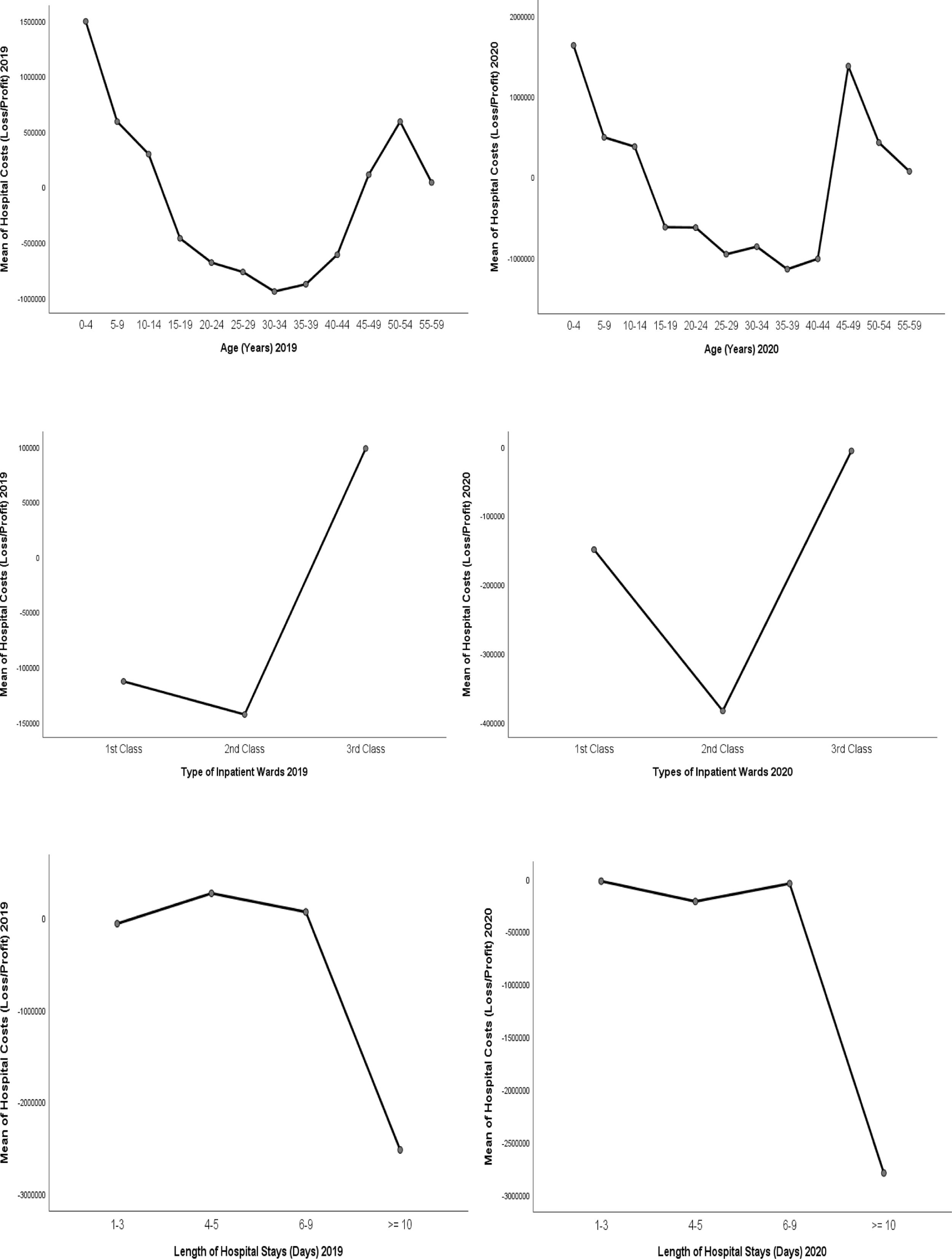
Graph 1 reveals there were significant differences in hospital costs, either hospital facing financial loss or profit, based on the patient age, type of inpatient wards, and length of hospital stays. In both years, similar trends were identified. As clearly seen in Graph 1, the hospitalization of patients aged 15–44 years had higher hospital costs that led to financial losses compared to those aged 0–14 and 50–59 years during 2019–2020 (p=0.0001). Moreover, patients admitted to the 1st and 2nd class of inpatients wards (p=0.004) and hospitalized more than 10 days (p=0.0001) also had higher hospital costs resulting in financial losses, compared to those admitted to the 3rd class of inpatient units and hospitalized less than 9 days.
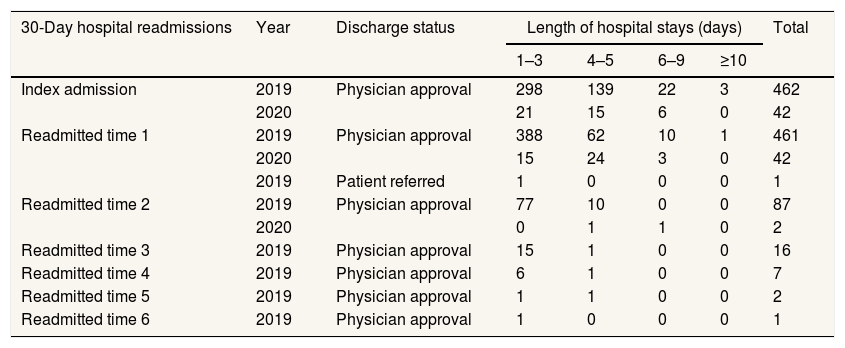
Table 3 demonstrates the 30-day hospital readmissions of insured patients hospitalized in the Indonesian mother & child hospital during 2019 and 2020 based on their discharge status and length of hospital stays. There were 462 patients who had index admission and discharged from the hospital with the physician approval in 2019 and 42 patients who had also index admission and discharged with the physician approval in 2020, unfortunately they experienced with 30-day hospital readmissions. All these patients readmitted once and less than 19% of them readmitted twice and up to 6 times to the hospital within 30 days after they were discharged from the initial admission. Patients who had readmissions three times or more were hospitalized less than 5 days, while those who had been readmitted twice or less were hospitalized more than 5 days.
Distribution of 30-day hospital readmissions based on discharge status and length of hospital stays of insured patients hospitalized in the indonesian mother & child hospital during 2019 & 2020.
| 30-Day hospital readmissions | Year | Discharge status | Length of hospital stays (days) | Total | |||
|---|---|---|---|---|---|---|---|
| 1–3 | 4–5 | 6–9 | ≥10 | ||||
| Index admission | 2019 | Physician approval | 298 | 139 | 22 | 3 | 462 |
| 2020 | 21 | 15 | 6 | 0 | 42 | ||
| Readmitted time 1 | 2019 | Physician approval | 388 | 62 | 10 | 1 | 461 |
| 2020 | 15 | 24 | 3 | 0 | 42 | ||
| 2019 | Patient referred | 1 | 0 | 0 | 0 | 1 | |
| Readmitted time 2 | 2019 | Physician approval | 77 | 10 | 0 | 0 | 87 |
| 2020 | 0 | 1 | 1 | 0 | 2 | ||
| Readmitted time 3 | 2019 | Physician approval | 15 | 1 | 0 | 0 | 16 |
| Readmitted time 4 | 2019 | Physician approval | 6 | 1 | 0 | 0 | 7 |
| Readmitted time 5 | 2019 | Physician approval | 1 | 1 | 0 | 0 | 2 |
| Readmitted time 6 | 2019 | Physician approval | 1 | 0 | 0 | 0 | 1 |
The main findings of this study were the hospital costs exceeded the BPJS health insurance tariff leading to financial losses and the patients experienced with 30-day hospital readmissions. For the first finding, the following patient and clinical characteristics were found increasing the hospital costs: patients’ age, INACBGs procedures & diagnoses by severity, type of inpatient wards, and length of hospital stays. Our study discovered that reproductive-age patients (15–44 years) were accounted for 91% of admissions that causing high-cost hospitalizations in 2019 and 2020. The high percentage of admissions reported in this age group because these reproductive-age patients most frequent encountered the hospital to receive reproductive and maternity health care services, particularly vaginal birth, C-section, dilatation & curettage, and abortion. This result is in line with the result from the earlier study reporting that relative per capita costs were higher in at child-bearing ages.8
The second finding was that hospitalizations for vaginal birth (mild & moderate), C-section (mild & moderate), dilatation & curettage (mild), abortion (mild), abdominal pain & other gastroenteritis (mild), viral/bacterial/non-bacterial infections (mild), and parasite diseases (mild) were reported not only high volume, but also high risks and costs in 2019 and 2020. High volume in patients admitted to the hospital for vaginal birth indicated that the health care access and utilization in the studied hospital after the implementation of the INACBGs tariff was better than before the prospective payment system implemented.9 This finding shows that the BPJS health insurance almost achieved the Universal Health Coverage (UHC) aims while also supporting the Sustainable Development Goal 3, “Good Health and Well-Being”.10,11 The high number hospitalization for patients received C-section procedures showed that patients had good awareness to seek help from the health care providers that were competent and safe.12
However, the third finding of this study revealed that although patients received similar INACBGs procedures and diagnosed with similar INACBGs diagnoses, their length of hospital stays were different (1–9 days) resulting in hospital costs exceeded the BPJS health insurance tariff. The discrepancies in length of hospital stays for patients with similar INACBGs diagnoses and procedures were mainly due to clinical guidelines had not been developed, integrated clinical pathways (ICPs) had not been implemented, and lack of interprofessional collaboration. The other reasons were hospital managers did not conduct regular patient care supervision, patient health record audits, and clinical decision making based on the BPJS e-claim database. Hence, hospital experienced with financial loss. This financial loss occurred mainly due to the hospital tariffs that determined by the South Sulawesi Government – as this hospital was under the management of it – were higher than the BPJS health insurance tariffs. This finding was relevant with the previous studies conducted in UNS teaching hospital and Ngawi regional public hospital that also found that the hospital tariffs were higher than the BPJS health insurance tariffs, but the earlier studies focusing on patients diagnosed with stroke and dengue haemorrhagic fever.13–15 These conditions led the hospitals faced financial losses as they had to cover the costs that exceeded the BPJS health insurance tariffs.14 In contrast, the result from a study conducted in the Sanglah hospital targeting patients diagnosed with breast, cervical, and nasopharyngeal cancers contradicted with our findings through which they reported that health care costs for these three types of cancers were lower than the BPJS health insurance tariffs. It means that the hospital did not provide extra money as all costs covered by the BPJS health insurance. The INACBG and hospital tariff discrepancies (profit/loss) found in some diagnoses and procedures at various hospitals must be addressed by reviewing the current INACBG tariffs and ensuring its implementation adheres to the goal of UHC and standardize for all Indonesian hospitals.3,10
The fourth finding was the hospital costs were higher than the BPJS health insurance tariff based on the type of inpatient wards and length of hospital stays. Patients admitted to 1st and 2nd class of inpatient wards and hospitalized for more than 10 days causing the financial loss. More than 10 days This finding is similar to the results from the previous study conducted in a private hospital in Yogyakarta, through which the researcher discovered that patients diagnosed with stroke admitted to the 1st class and hospitalized for more than 7 days had higher average real costs than the INACBGs costs (the BPJS health insurance tariff).15
Finally, the last finding of this study was patients who discharged from the hospital with the physician approval at index admission readmitted to the hospital within 30 days after they had been discharged. The most frequent 30-day hospital readmissions found in this study were patients diagnosed with the following ICD-10-CM Codes: Z48.8 (encounter for other specified postprocedural aftercare) and O34.2 (Maternal care for scar from previous caesarean section).16,17 This finding was relevant with the findings from a study conducted in the Ireland hospital reporting that complications of C-section was one of the causes for readmission.18
This study had a limitation which was the BPJS e-claim datasets from the studied hospital did not provide breakdown for the hospital costs based on the health care services received by each patient admission. Hence, future study is needed to evaluate the hospital costs spent based on the health care services delivered to the patients.
ConclusionHospital financial loss and 30-day hospital readmissions would be addressed by implementing ICPs that were developed based on clinical guidelines and delivering care with interprofessional collaboration approach through the implementation of professional nursing practice model.
Conflicts of interestThe authors declare no conflict of interest.
This study was supported by the grant from the Institute for Research and Community Service [Lembaga Penelitian dan Pengabdian Kepada Masyarakat], Universitas Hasanuddin, Makassar, Indonesia with the Grant ID #1585/UN4.22/PT.01.03/2020.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.