The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoThis study was to determine the relationship between a praziquantel-related adverse event with the health community perception to chemopreventive of Schistosomiasis in Dodolo village, Napu Valley, Central Sulawesi.
MethodsA cross-sectional study was conducted among the 79 residents of Dodolo village, who following praziquantel-mass drug administration. A-questionnaire was used to collect demographic information of the subject who participated in the study, the presence of treatment-related symptoms, and community perception. The health perception was based on the health belief model (HBM) framework. Data were analyzed using Chi-square.
ResultThe incidence of praziquantel-related adverse events was 92% (73), with the highest frequency were nausea (69%), vomit (57%), and headache (47%). The total number of treatments related to symptoms was significantly correlated with age (p 0.030). 78% (62) of participants had a supportive perceived susceptibility, 71% (56) participants had a supportive perceived severity, 63% (50) participants had supportive perceived benefits, meanwhile 58% (46) had a not supportive perceived barrier to praziquantel mass drug administration. The presence of praziquantel-related adverse events was significantly correlated with a perceived barrier of the participant to the chemopreventive program.
ConclusionThe Dodolo community had a supportive health perception for the success of the Schistosomiasis elimination program, despite the high frequency of adverse events after praziquantel consumption.
Schistosomiasis is a parasitic disease caused by trematodes of the genus Schistosoma. There are two major Schistosomiasis – Intestinal and urogenital – caused by five main species of Schistosoma, which are transmitted through water, contain infected feces and urine. Schistosomiasis is a chronic disease presenting in subsequent symptoms, including fever, malaise, growth failure, hematemesis, and irreversible organ damage. One of the most life-threatening Schistosomiasis complications is liver cirrhosis and bladder cancer.1–3 Considered as a neglected tropical disease, Schistosomiasis remains a serious global public health problem that affected more than 250 million people worldwide, with high prevalence in tropics and subtropics areas.4,5 Preventive chemotherapy using mass drug administration (MDA) of praziquantel is one of the strategies recommended by WHO to control Schistosomiasis. At least 229 million people required chemopreventive in 2018.6 The success of this chemopreventive program is determined by some factors like compliance, coverage, community knowledge, and also acceptability to the drugs.7
Praziquantel (PZQ) is a recommended drug against all stages of schistosome. PZQ with a dose of 40–60mg/kg body weight was given yearly up to 5 years for a minimum of 75% coverage for people in endemic areas. These treatments aim to reduce mortality and morbidity and also prevent new infection by reducing transmission through human and animal reservoir MDA with praziquantel giving a challenge because of its size, taste, quantity, and side effect after consumption.8 Some studies reported side effects of PZQ such as headache, nausea, abdominal pain, and syncope, which lasting 30min up to 4h after treatment.9–11 Those weaknesses of PZQ could give a bad community health perception related to programs and decrease compliance in the next round of MDA if they do not treat properly. Therefore health promotion and some prevention of compliance programs should be given intensively to increase community knowledge along with the compliance and coverage rate of MDA.
Schistosomiasis in Indonesia is exclusively endemic in three areas in Central Sulawesi Province including Lindu Lake, Bada Valley, and Napu Valley. Dodolo village, located in Napu valley, is the area with the highest prevalence of Schistosomiasis, 2.7% in 2017. The objective of this study was to determine the relationship of adverse events after praziquantel consumption and the community perception of MDA praziquantel in the Dodolo village as the area with the highest prevalence of Schistosomiasis in Indonesia.
MethodsThis study was a cross-sectional study conducted in Dodolo village, Napu Valley, Central Sulawesi Province, Indonesia. Dodolo village is located in Lore Utara Sub-district, Poso District, Central Sulawesi Province, Indonesia. The study area represents the highest prevalence of Schistosomiasis in Indonesia. Dodolo village has a total population of 389 people (2018). The study population consists of all individuals in this village who eligible to consumpt praziquantel as MDA for Schistosomiasis. The ones who did not eligible were elderly 65 years old, pregnant woman, children under five years old, and severe-ill persons. The study participant included a random sample of 79 people drawn from Dodolo village in September 2018. Respondents were interviewed at their homes three days after the implementation of the MDA of praziquantel in this village.
The data were collected using structured-questioners. The first questioner asked the independent variables included: patients demographics and whether they had had a headache, fever, dizziness, diarrhea, stomachache, vomiting, nausea, syncope, urine discoloration, decreased appetite, and rash immediately after taking praziquantel up to the following two days. An adverse event was a measure on the nominal scale and grouped into the present and not present of PZQ-related adverse events. The second, a-structure questioner about dependent variable: community perception based on Health Belief Model which determine perceived of severity (degree of seriousness a person believes his condition creates for him), perceived of susceptibility (the degree to which a person believes he is at risk for hospitalization), perceived of benefits (the perceived efficacy of treatment and attitude toward a provider), and perceived of barrier (the deleterious side effect of praziquantel). The community perception was measured on a nominal scale and grouped into supporting and not supporting perceptions. Data were analyzed using the Chi-square test, and a p value less than 0.05 was cut-off for a significant difference.
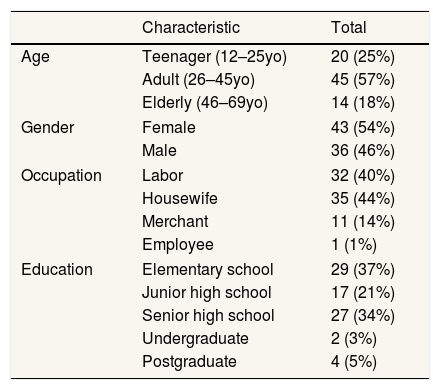
ResultDistribution of respondentsThe data of socio-demographic characteristics of respondents can be seen in Table 1.
Socio-demographics characteristics of respondents.
| Characteristic | Total | |
|---|---|---|
| Age | Teenager (12–25yo) | 20 (25%) |
| Adult (26–45yo) | 45 (57%) | |
| Elderly (46–69yo) | 14 (18%) | |
| Gender | Female | 43 (54%) |
| Male | 36 (46%) | |
| Occupation | Labor | 32 (40%) |
| Housewife | 35 (44%) | |
| Merchant | 11 (14%) | |
| Employee | 1 (1%) | |
| Education | Elementary school | 29 (37%) |
| Junior high school | 17 (21%) | |
| Senior high school | 27 (34%) | |
| Undergraduate | 2 (3%) | |
| Postgraduate | 4 (5%) | |
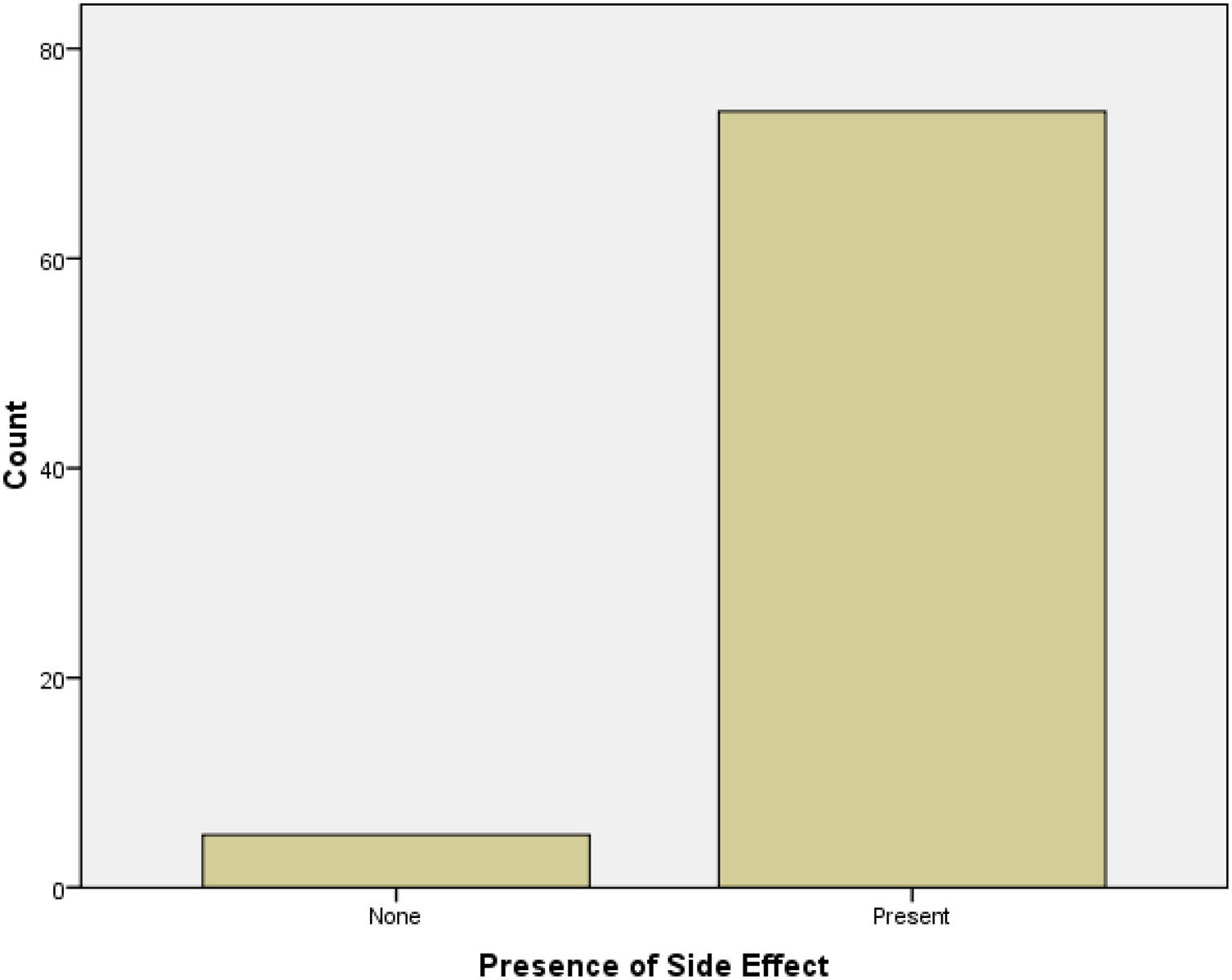
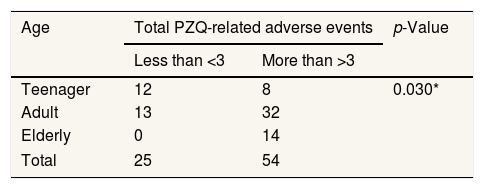
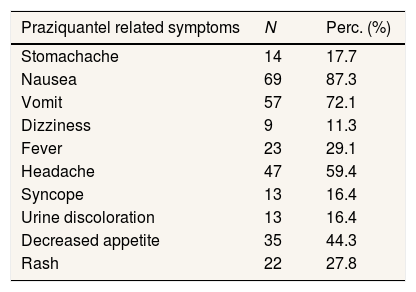
PZQ-related adverse event incidence is presented in Table 1. Out of 79 people, 73 (92%) showed up for the interview 48h post-treatment about PZQ-related adverse events that they had experienced. Sixty-four persons experienced more than three symptoms, and the most commonly reported PZQ-related adverse events were nausea (69%), vomit (57%), and headache (47%). The total manifested symptoms showed significantly associated with age (p value 0.030). The highest frequency of PZQ-related symptoms being observed in the elder (40–69 years) group with 14 of 14 persons, followed by a group of people in 26–45 years old with 32 of 45 persons experiencing PZQ-related symptoms. Most of the PZQ-related adverse events were transient and mild, lasting only 30min to 5h after treatment. A list of symptoms related to praziquantel consumption was shown up in Table 3, and the Presence of PZQ-related adverse events following the MDA program in Dodolo village can be seen in Fig. 1.
The data of total manifested-symptoms related to PZQ consumption based on group age can be seen in Table 2.
The list of treatment-related symptoms after praziquantel consumption can be seen in Table 3.
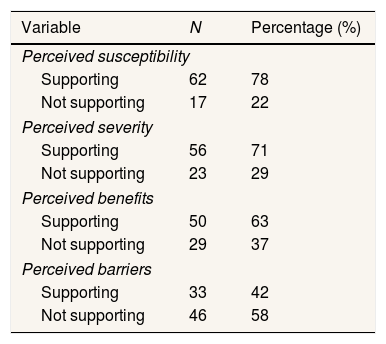
Analysis of community perception related to MDA Praziquantel ProgramThe data of a summary of the participant's perceptions toward MDA praziquantel based on the health belief model can be seen in Table 4.
The summary of participant's perceptions toward mda praziquantel based on the health belief model.
| Variable | N | Percentage (%) |
|---|---|---|
| Perceived susceptibility | ||
| Supporting | 62 | 78 |
| Not supporting | 17 | 22 |
| Perceived severity | ||
| Supporting | 56 | 71 |
| Not supporting | 23 | 29 |
| Perceived benefits | ||
| Supporting | 50 | 63 |
| Not supporting | 29 | 37 |
| Perceived barriers | ||
| Supporting | 33 | 42 |
| Not supporting | 46 | 58 |
The data showed that 62 people had a supporting health perception toward susceptibility to disease, in which 58 people experienced a side effect, and four people had no side effect after praziquantel consumption. Meanwhile, 17 people had a not supporting health perception, with 16 people had praziquantel's side effect. There was no significant relationship between the presence of praziquantel-related symptoms and perception of susceptibility toward Schistosomiasis. Fifty-six persons had a supporting perception of the severity of the disease, while 23 persons had not supporting health perception. Among 56 people who had a supporting perception, 54 persons experienced praziquantel's side effect, and two persons have no symptoms. In 23 people who had not supported health perceived severity, 20 people had experienced treatment-related symptoms, and three people without any symptoms after praziquantel consumption. There was no significant relationship between the presence of praziquantel-related symptoms and perceptions of the severity of the disease.
The result showed that 50 people had a good health perception toward benefit MDA using praziquantel even though 47 people experienced treatment-related symptoms after praziquantel consumption. On the other hand, there were 29 people who had not a supporting health perception with 27 people had praziquantel's side effects, and two people had not any symptoms. There was no significant relationship between the Presence of praziquantel-related symptoms and the perception of benefits toward praziquantel-mass drug administration. The relation between Presence of treatment-related side effect symptoms and Community Perception Toward MDA praziquantel in Dodolo village can be seen in Table 5.
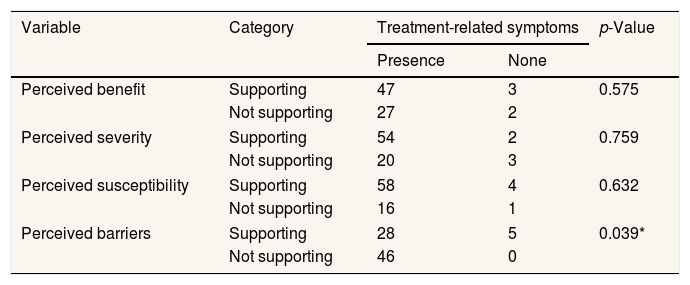
Relation between presence of treatment-related side effect symptoms and community perception toward MDA praziquantel in Dodolo village.
| Variable | Category | Treatment-related symptoms | p-Value | |
|---|---|---|---|---|
| Presence | None | |||
| Perceived benefit | Supporting | 47 | 3 | 0.575 |
| Not supporting | 27 | 2 | ||
| Perceived severity | Supporting | 54 | 2 | 0.759 |
| Not supporting | 20 | 3 | ||
| Perceived susceptibility | Supporting | 58 | 4 | 0.632 |
| Not supporting | 16 | 1 | ||
| Perceived barriers | Supporting | 28 | 5 | 0.039* |
| Not supporting | 46 | 0 | ||
Based on the data of perception toward the barrier, 33 people had a supporting health perception; meanwhile, 46 people were in the opposite. Among 33 people, there was 28 people had to experience treatment-related symptoms, and five people had none symptoms after praziquantel consumption. All of 46 people who had a not supporting health perception of the barrier had had experience praziquantel related symptoms. The result of the Chi-square test indicated there was a significant relationship between the Presence of treatment-related symptoms and the perceived barrier of people in Dodolo village toward mass drug administration praziquantel to eliminate Schistosomiasis (p value=0.039).
DiscussionThis study evaluated the presence of treatment-related symptoms suggestive side effects of praziquantel and its correlation with community health perception based on the Health Belief Model. We found that 94% of treated persons experienced some symptoms after drug consumption. Most of the symptoms were mild and transient, lasting from 30min until 5h after consumption.5 The most frequence of the treatment-related symptoms were nausea, headache, and vomit. This data was in agreement with previous studies, even though there are variations in the overall incidence and frequency of the symptoms observed. A study by Erko et al. (2012) observing side effects of praziquantel in mass drug administration for Schistosoma mansoni in Ethiopia reported overall side-effect incidence was 83%, with the most frequent being headache (47%), nausea (43%), and abdominal pain (39.9%). This variation might be caused by different agents of the parasite, an intrinsic factor of the host, pre meals treatment status, nutritional status, the intensity of infections, and drug factors.10
Praziquantel is the drug of choice for Schistosomiasis since 1970. PZQ has the ability to stimulate the worm's motor activity, spasmodic contraction of musculature, and formation of the vesicle in the tegument, which caused the death of the worm.12 Praziquantel is used in MDA Schistosomiasis programs for children >5 years until the elderly. This study observed that 54% of treated persons complained of experienced more than three symptoms after praziquantel consumption. A-number of treatment-related symptoms had a significant association with age, in which the elderly in the 45–69 age group experienced a high proportion of side effects. In contrast with a study by Erko, which reported a high proportion of PZQ-related adverse events in the 10–14 age group, which had a correlation with pre-treatment Schistosoma infection intensity.10 Despite the difference in age group, both studies agree that a-number of treatment-related symptoms had an association with age. It might be caused by the intrinsic factor of the host to metabolize the drug and the total amount of chemicals released from dying schistosomes. Since this study did not evaluate the pre-treatment intensity of infection, further study is needed.
Some factors like knowledge, perception are associated with an increased likelihood of uptake praziquantel during the MDA program. The Health Belief Model (HBM) provides a useful framework for discussing the correlation between people's knowledge, perception, and attitude to diseases on the one hand and their decision toward prevention action on such diseases. Based on the Health Belief Model, this study divided perceptions into five parts, perception of susceptibility, perception of benefits, perceived of the barrier, and perception of severity. Perceived susceptibility refers to an individual's subjective perception of the like hood of getting a disease or illness. According to our study finding, 68 respondents (78%) felt that they were susceptible to getting Schistosomiasis, which could be referred to as a supportive perception. A sense of being threatened against a disease encourages the community to take necessary health actions to protect themselves from the disease. In this case, the community will have a willingness to take part in Schistosomiasis preventive programs conducted by the government. Perceived severity refers to the feeling of the seriousness of suffering the disease or leaving it untreated. This study found that 56 participants (71%) thought that Schistosomiasis is a serious health problem that can lead to death. It was also a supportive perception of the chemopreventive program. The more seriously a person feels Schistosomiasis, the more likely they will adopt healthy habits for prevention or to reduce its severity. A supportive perceived susceptibility and perceived severity can be a success factor in the implementation of the Schistosomiasis elimination program.
Perceived benefits refer to an individual's assessment of the value in joining praziquantel mass drug administration to reduce the threat of Schistosomiasis. The study showed that 50 participants (63%) felt getting the advantages of joining the MDA program. The HBM proposes that the more benefits that individuals perceive will have regarding advantages of treat, then the more likely they will engage in the next round of MDA program regardless of objective fact concerning the effectiveness or adverse events of the drug consumption. The perceived benefits have to outweigh the perceived barriers in order for health behavior to occur. Perceived barriers refer to a potential complication involved in praziquantel consumption, which can act as obstacles to undertaking the MDA program. According to the data, 33 participants (42%) had not felt a barrier to taking the drugs; meanwhile, the rest, 46 persons, felt the barrier of undertaking the praziquantel. Having a perception of having no barrier to undertaking the chemopreventive program is a supportive health perception toward the chemopreventive program. 28 of 33 persons with supporting health perception had had experienced adverse events after taking the drugs, and all of the 46 people who had not supportive perceived of the barrier, felt any symptoms after PZQ consumption.
Among the four perceptions, only perceived barriers of the MDA program was found to significantly influenced by the presence of treatment-related symptom after praziquantel consumption. Participants who got the praziquantel's side effects more likely to feel the disadvantages of joining the MDA program. This should be a warning for the local government because the presence of side effects could influence the community to not taking the drugs anymore and contribute to non-compliance of MDA in the next round. The fear of adverse reactions to praziquantel, along with lack of knowledge about Schistosomiasis and misconception about alternative forms of treatment, were associated with non-compliance to MDA treatment in the rural Philippines.6
Before the next round of the MDA program, some side effect prevention strategies should be done. Pre-treatment snack which is given to prevent treatment side effect as shown in Uganda, which also can contribute to increasing the coverage of treatment.13,14 The Presence of PZQ-related symptoms had no correlation with perceived susceptibility, perceived severity, and perceived benefits. The community thought that its important to take part in the MDA program even though they suffered side effects symptoms, respectively. Based on perceived susceptibility, perceived severity, perceived benefits, and perceived barriers, the Dodolo community had a supportive perception for the success of the Schistosomiasis elimination program, despite there was a high-frequency incidence of PZQ-related symptoms. This study had a limitation do not cover all of the endemic Schistosomiasis in Indonesia. Further studies with bigger area and higher number of participants are needed.
ConclusionThe Dodolo community had a supportive health perception for the success of the Schistosomiasis elimination program, despite the high frequency of adverse events after praziquantel consumption.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.