The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
More infoThis study aims to describe the implementation of continuity of care model in maternal health services starting from pregnancy, childbirth, and the puerperium.
MethodsLiterature is obtained from online journal databases, namely PubMed, EBSCO, and ScienceDirect, and other related sources, systematically from 2012 to 2019.
ResultsSixteen articles on the implementation of the continuity of care model of antenatal, intranatal, and postnatal care were described by demographic characteristics, scope, and impact. Barriers and facilitators for three categories include process, communication, information and education, organization and human resources, caseload, burnout, psychological, expectation, and satisfaction.
ConclusionThe continuity of care model is useful for developing sustainability settings in all maternal health services. The practical implication is the feasibility of a midwife-led continuity of care model to avoid service dropouts. The quality of service is determined by the psychological comfort of women. Further considerations, need to include collaboration in this model.
Continuity of maternal care is a model that was first used in 1970 according to Liebowitz and Brody (1970), revealing that no patient was lost to follow-up or separated from care.1 This continuity model is supportive and useful for increasing service coverage and satisfaction for mothers, families, the wider community, midwives, and nurses. This care delivery strategy is needed to reduce maternal morbidity and mortality.2 However, trends in philosophical approaches that differ from professional collaboration service groups in maternity care arise in routine practice. In both Western and Eastern countries, there is an assumption that midwives’ practice when labor is normality and obstetricians focus on managing complications of labor. From evidence-based statements, the benefits of normal delivery minimize surgical intervention.3 Practices of the continuity of care (CoC) model in several countries are inadequate. Constraints that arise are women's limited access to facilities and service providers, health workers, caseload, family support, lack of partnerships, and community participation. Of some articles that will be known in this study, for example, studies in Australia less than 10% of women have access; In the United Kingdom by Pangas et al. (2019) and New Zealand by Gray et al. (2016) has the highest continuation rate of around 85%, services are provided in an integrated manner to save costs,4 and reduce caseloads.5 Furthermore, research in Africa on service outages occurred in the postpartum period,6 and sub-Saharan Africa had a low level of CoC utilization.7 The results of the following study also revealed that unfavorable experiences occurred in the health care system by Grigg and Tracy (2013), Berg et al. (2012) in Swedish8,9 and the emergence of cultural, social, and communication barriers, and about the possible lack of trust in decision making.
Although many reviews have been carried out, we have taken the initiative to discuss practical evidence from some of these CoC model studies as a reference for experiences in the model of care practices in three maternal services that are often disconnected and have an impact on declining and deteriorating health conditions in the community. Therefore, this review aims to identify and learn more about the implementation of the CoC model received by mothers from service providers in three service categories, namely antenatal care (ANC) during pregnancy, intranatal care (INC) during delivery, and postnatal care (PNC).
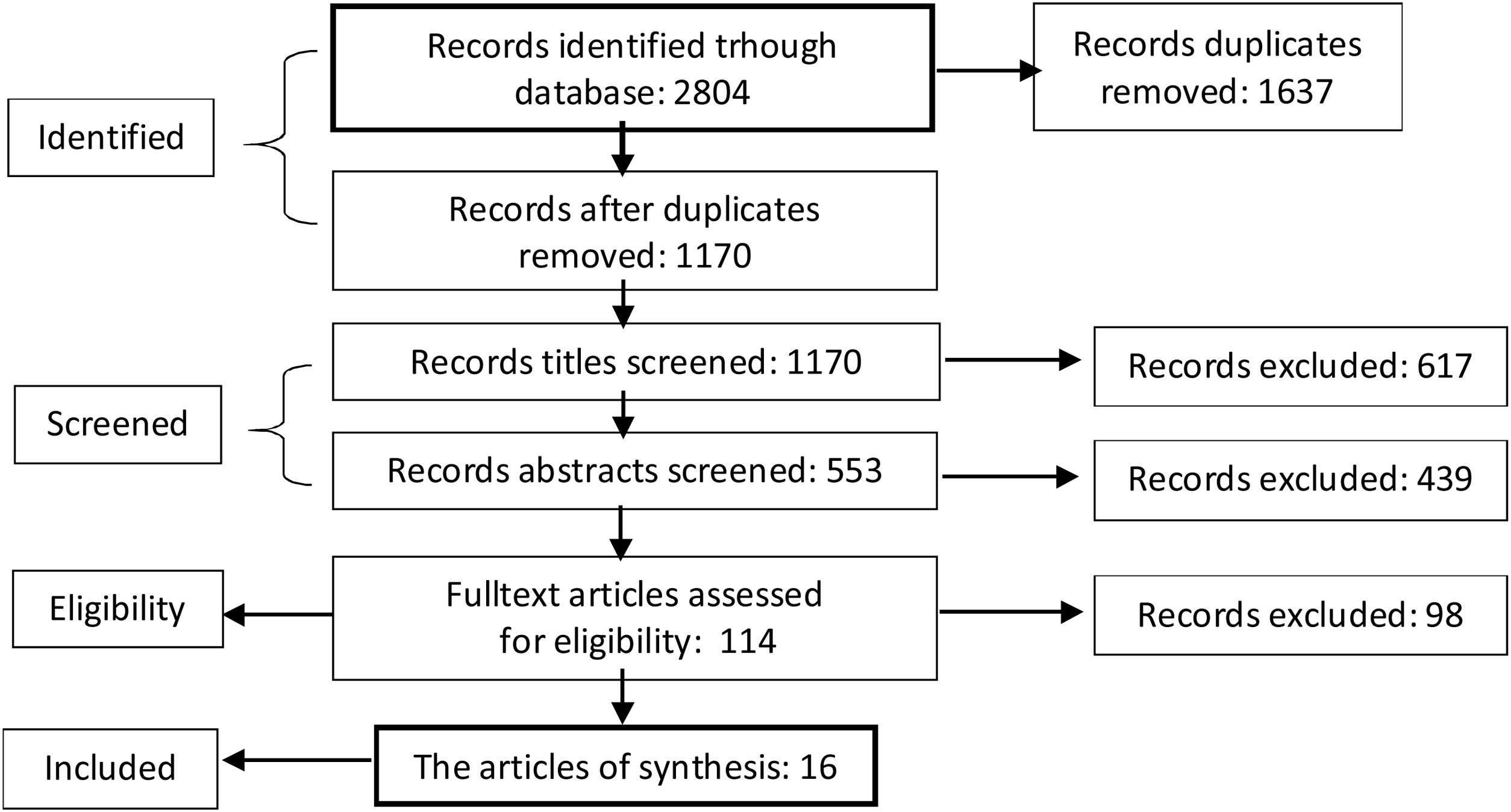
MethodsLiterature search strategyWe conduct a literature review, systematically in line with the Pre-ferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.10 A computerized search was performed using Pubmed, Medline, Researchgate, Google Scholar, and the science web. Search studies were published between 2012 and 2019.
Eligibility criteriaThe process starts with the title and abstract filtering. Articles were independently reviewed based on inclusion criteria. Reference was found to the experiences of women, midwives, and service providers in the CoC model. The articles that were excluded were women with high-risk pregnancies and cesarean sections, the practice of the CoC model by midwifery students while studying at a midwifery academy, and issues of ethnicity, religion, race, and other conflict groups.
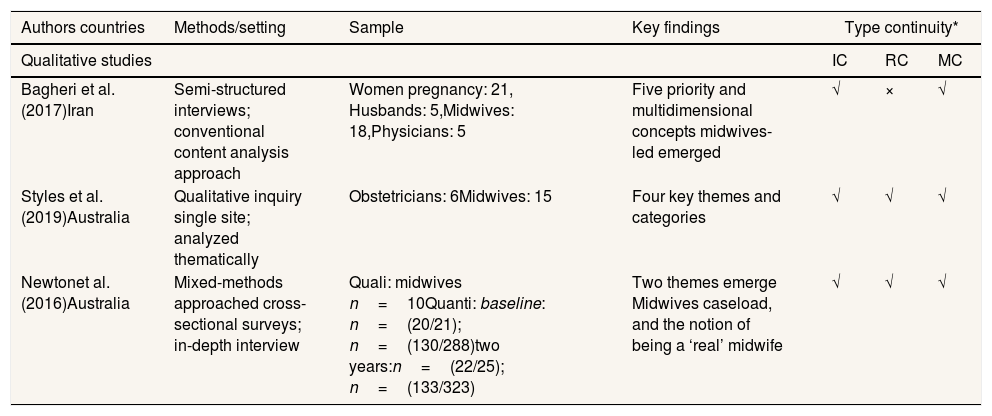
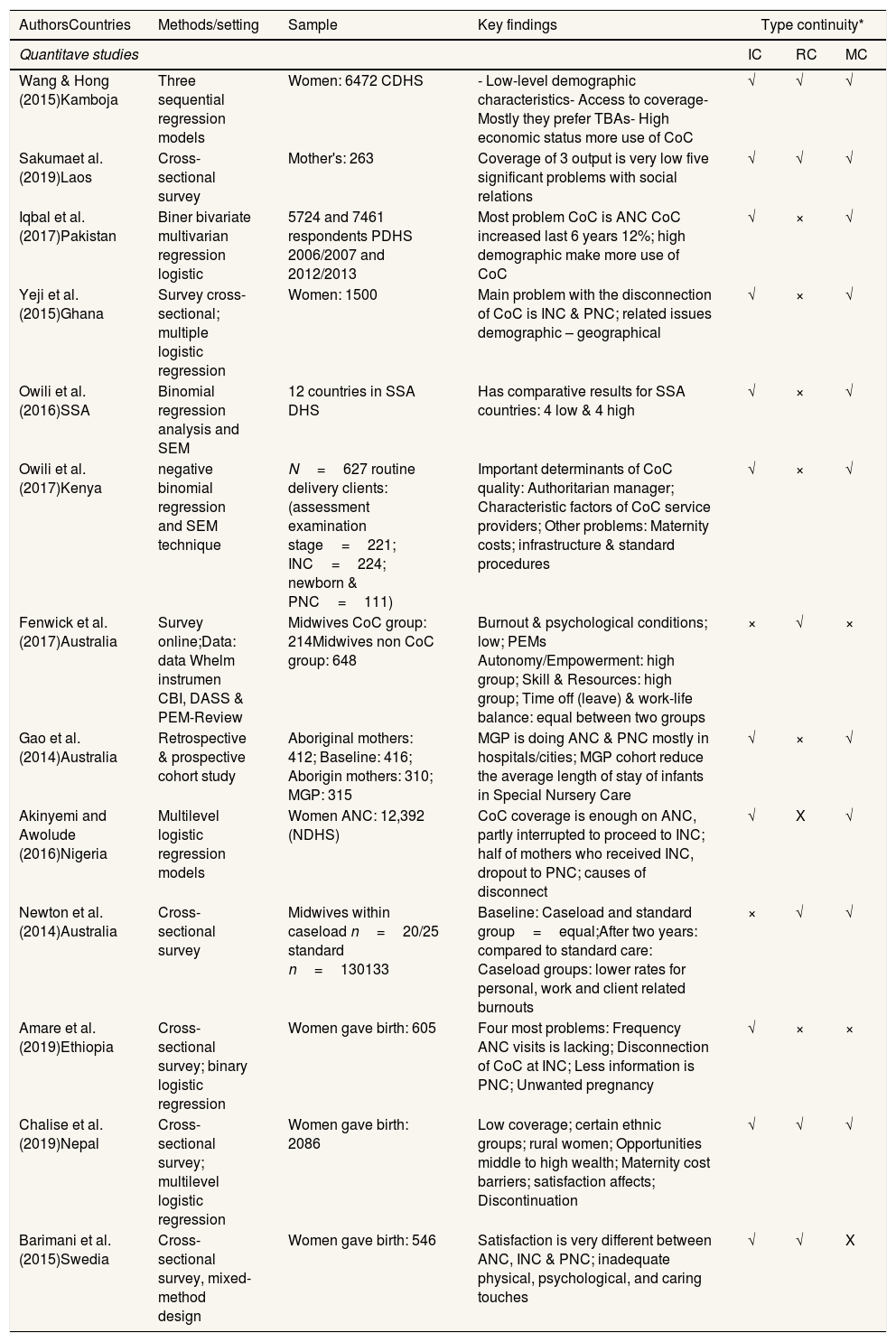
The data extraction and synthesisThe literature was analyzed using a data extraction template. Templates are designed using keywords and scoring rubrics on relevant papers. Information extracted from each literature includes a country, objective, type of study, data collection, study sample size, and findings. Synthesis analyzes are presented and organized in an extraction table format (Table 1). Findings are presented in a narrative manner, taking into account each review question in order.
Synthesis of study results in qualitative research.
| Authors countries | Methods/setting | Sample | Key findings | Type continuity* | ||
|---|---|---|---|---|---|---|
| Qualitative studies | IC | RC | MC | |||
| Bagheri et al. (2017)Iran | Semi-structured interviews; conventional content analysis approach | Women pregnancy: 21, Husbands: 5,Midwives: 18,Physicians: 5 | Five priority and multidimensional concepts midwives-led emerged | √ | × | √ |
| Styles et al. (2019)Australia | Qualitative inquiry single site; analyzed thematically | Obstetricians: 6Midwives: 15 | Four key themes and categories | √ | √ | √ |
| Newtonet al. (2016)Australia | Mixed-methods approached cross-sectional surveys; in-depth interview | Quali: midwives n=10Quanti: baseline: n=(20/21); n=(130/288)two years:n=(22/25); n=(133/323) | Two themes emerge Midwives caseload, and the notion of being a ‘real’ midwife | √ | √ | √ |
Covering 2804 articles were identified, 1170 abstract titles relevant to research objectives were screened. 114 articles were retrieved and reviewed based on inclusion and exclusion criteria and 16 articles were obtained descriptively (Fig. 1).
Study characteristicsSummaries of 16 articles, five conducted in Australia, five in Africa, five in Asia, and one study from Sweden. Two qualitative design articles, one mixed method (Table 1), and 13 quantitative articles (Table 2).
Synthesis of study results in quantitative research.
| AuthorsCountries | Methods/setting | Sample | Key findings | Type continuity* | ||
|---|---|---|---|---|---|---|
| Quantitave studies | IC | RC | MC | |||
| Wang & Hong (2015)Kamboja | Three sequential regression models | Women: 6472 CDHS | - Low-level demographic characteristics- Access to coverage- Mostly they prefer TBAs- High economic status more use of CoC | √ | √ | √ |
| Sakumaet al. (2019)Laos | Cross-sectional survey | Mother's: 263 | Coverage of 3 output is very low five significant problems with social relations | √ | √ | √ |
| Iqbal et al. (2017)Pakistan | Biner bivariate multivarian regression logistic | 5724 and 7461 respondents PDHS 2006/2007 and 2012/2013 | Most problem CoC is ANC CoC increased last 6 years 12%; high demographic make more use of CoC | √ | × | √ |
| Yeji et al. (2015)Ghana | Survey cross-sectional; multiple logistic regression | Women: 1500 | Main problem with the disconnection of CoC is INC & PNC; related issues demographic – geographical | √ | × | √ |
| Owili et al. (2016)SSA | Binomial regression analysis and SEM | 12 countries in SSA DHS | Has comparative results for SSA countries: 4 low & 4 high | √ | × | √ |
| Owili et al. (2017)Kenya | negative binomial regression and SEM technique | N=627 routine delivery clients: (assessment examination stage=221; INC=224; newborn & PNC=111) | Important determinants of CoC quality: Authoritarian manager; Characteristic factors of CoC service providers; Other problems: Maternity costs; infrastructure & standard procedures | √ | × | √ |
| Fenwick et al. (2017)Australia | Survey online;Data: data Whelm instrumen CBI, DASS & PEM-Review | Midwives CoC group: 214Midwives non CoC group: 648 | Burnout & psychological conditions; low; PEMs Autonomy/Empowerment: high group; Skill & Resources: high group; Time off (leave) & work-life balance: equal between two groups | × | √ | × |
| Gao et al. (2014)Australia | Retrospective & prospective cohort study | Aboriginal mothers: 412; Baseline: 416; Aborigin mothers: 310; MGP: 315 | MGP is doing ANC & PNC mostly in hospitals/cities; MGP cohort reduce the average length of stay of infants in Special Nursery Care | √ | × | √ |
| Akinyemi and Awolude (2016)Nigeria | Multilevel logistic regression models | Women ANC: 12,392 (NDHS) | CoC coverage is enough on ANC, partly interrupted to proceed to INC; half of mothers who received INC, dropout to PNC; causes of disconnect | √ | X | √ |
| Newton et al. (2014)Australia | Cross-sectional survey | Midwives within caseload n=20/25 standard n=130133 | Baseline: Caseload and standard group=equal;After two years: compared to standard care: Caseload groups: lower rates for personal, work and client related burnouts | × | √ | √ |
| Amare et al. (2019)Ethiopia | Cross-sectional survey; binary logistic regression | Women gave birth: 605 | Four most problems: Frequency ANC visits is lacking; Disconnection of CoC at INC; Less information is PNC; Unwanted pregnancy | √ | × | × |
| Chalise et al. (2019)Nepal | Cross-sectional survey; multilevel logistic regression | Women gave birth: 2086 | Low coverage; certain ethnic groups; rural women; Opportunities middle to high wealth; Maternity cost barriers; satisfaction affects; Discontinuation | √ | √ | √ |
| Barimani et al. (2015)Swedia | Cross-sectional survey, mixed-method design | Women gave birth: 546 | Satisfaction is very different between ANC, INC & PNC; inadequate physical, psychological, and caring touches | √ | √ | X |
Abbreviations: CoC: continuity of care; MGP: Midwifery Group Practice; ANC: Antenatal Care; INC: Intranatal Care; PNC: Postnatal Care; CHC: Child Health Care; MNCH: Maternal, Newborn and Child Health; DHS: Demographic and Health Surveys; SSA: sub-Saharan Africa; TBAs: Traditional Birth Attendants; IC: Information Continuity; RC: Relationship Continuity; MC: Management Continuity; Type Continuity*: √: yes; ×: no.
Research location characteristics were collected from health facilities, communities, and states. There are 7 studies using DHS data, one online computer-based survey, and 8 questionnaires. Many quantitative methods are 12 cross-sectional studies, as well as one prospective cohort study. Most analysis tests use multivariate regression models and SEM 11 studies, followed by descriptive analysis. One study was conducted with a cohort design.11
All identified studies were midwifery care practices in antenatal (pregnancy), intranatal (childbirth), and postnatal (postpartum) care in hospitals, health centers, and even districts/states.12 Most of the studies describe complete socio-demographic characteristics. Two qualitative studies13,14 related to changes in management, organization, and changes in professionalism in the workplace of midwives, nurses, and doctors.
Meanwhile, the elements of hope and satisfaction of women, husbands, and families are emphasized. Another illustration, research in Australia, midwives, or nurses experience caseload, fatigue, psychological conditions, and open communication between them. Likewise in studies in Asia and Africa, coverage of the three service categories found the impact of CoC chain including its accompanying characteristics.
Three types of continuityThree types of continuity are reviewed to see the part of the continuity setting based on the findings obtained in the CoC model practice. This finding refers to the concept of Haggerti et al. (2003) on Continuity of care: a multidisciplinary review.15
Information continuityContinuity of information reported is an unsatisfactory response,16,17 the husband is confused where, to whom exactly complaints and questions are asked, less see the condition of mother,18,19 reliable source of information and education reliable source of information and education,13,20 unwanted pregnancy, future hopes for both parties, midwives always there, and on time.14 And, CoC perception is emphasized on caseload, burnout,18 and rather than general labor. However, on other hand, the workload is felt by midwives as being directly involved in a woman's real life.21 Most of the findings of maternal characteristics are demographic, socioeconomic, educational, and location distance,22–24 skills, resources: health facilities, medicines, standard procedures,23 delivery costs,17 information media, and transportation,19 traditional birth attendants in PNC.22
Relationship continuityThe practice of midwives in this finding revealed that women should understand how the practice of midwives worked during ANC to PNC, caseload with general care,21,24 family support, and joint decision making between women (mothers), families (husbands), and midwives. Newton et al. (2015)21 emphasize the uniqueness that first: work is a vocation that marginalizes personal needs, free time is provided, although burnout appears, at the same time must avoid boredom. Second: The notion of becoming a ‘real’ midwife. Psychological interaction between midwives and women has a comforting effect, that it turns out that in addition to a precious call also brings hope that they (midwives) become empathy, alert, and awake whenever needed, for the care process, given physical touch is also obtained psychological touch that affects effective communication and service satisfaction.23
Management continuityThis section focuses on how CoC is carried out and what are the results? The role of management, structural/organizational change, client, and service provider satisfaction. In line with the findings of some of these review studies, how important is access to coverage, the emergence of dropouts of services, their responsibilities and changing needs, service providers across programs, competence, and preparedness? In cases where this connection exists, concluded the importance of interprofessional collaboration and planning the right way and time.
Then, what is the scope of CoC and display out of service? Access to CoC coverage only increased antenatally, even among sub-Saharan Africa 4 low and 4 high from 12 states.7 Conversely, for less coverage, low in PNC and INC,6 and the lowest is ANC.12 Meanwhile, the output is lacking in three maternal care. For loss of CoC services, intranatal occurs,20 antenatal,11,17 appear in the intranatal half, and postnatal because of cost, rural and remote location, low education, and poor.6
In addition to drop out of service, another important aspect is the lack of ANC and PNC health facilities, authoritarian managers,23 Midwifery Group Practices mostly in urban hospitals.11 Professional satisfaction from the caseloads group, good interaction, reduced burnout, after a two-year trial from the baseline. Furthermore, qualitative studies, discussed management, the nursing process includes a philosophy: responsibility, being present on time, and effective communication. Example of a special faculty member interview “if we are going to reduce cesarean birth rates, midwives must always be accessible to pregnant women”. In home care management: high internal and external coordination, evaluation, program revision, and documentation increase. Therefore, the rights of recipients and health service providers are needed. Also, there is a neglect of professionalism ethics, commitment and human values, client rights and health provider rights,13 organizational changes, and future directions.14 That is the main interest of professionalism that should be avoided as a continuous violation. Professionalism also involves responsibility, accountability, autonomy, and legitimacy of the practice.21
DiscussionThe important insights discussed are contributions that are broader than just aspects of knowledge. Various information facilitates their access to continuing care, and this is very dependent on the history of pregnancy, childbirth, and the postpartum period, so that mothers feel comfortable in making decisions, receiving health facilities, and choosing who is the provider of services. It also discusses decision-making which is the shared responsibility of women (mothers), families (husbands) and midwives, or nurses.9 Then in this discussion also evidence of practice from CoC model for ANC, INC, and PNC problems in MNCH from several countries is emphasized.
Information continuityOverall, the study shows that demographic characteristics, time, and place have an impact on each indicator of service coverage. Assessment of female characteristics is important as early recognition of risk factors and how the use of resources determines the priority of maternal best practice. In this regard, strategic efforts need to be strengthened at the micro-system level, and a holistic approach through socio-cultural, personal relationships between women and midwives, emotional, physical, and spiritual needs, in accordance with women's own expectations.25
Relationships continuityAcknowledging the evidence of this CoC model, in Indonesia, it is both a challenge and an opportunity to achieve universal targets and reduce maternal mortality2 which is still the center of attention in Asian and African countries. Why is it important to study income differences and the similarities and geographic characteristics of different countries? Because responsive services can be provided to bridge the psychological needs of women and midwives or other related professions.26 Satisfaction and women's psychology as a measure of value and quality that must be presented and recognized.27,28
Management continuityThe barriers and facilitator elements play a role in determining the path between communication, two-way interaction, and management change. Therefore, detailed service findings vary in understanding patterns. One of the antenatal confounding factors is the case of unwanted pregnancy. For ANC, access is first made, and 42 days after delivery is the end of full service. INC was cut off due to constraints on the distance from the house to the facilities and assistance was not on time. For PNC, it is the highest mortality trend due to bleeding and eclampsia which is often ignored because it is considered a transitional period or rest at home so that these cultural and cultural factors also determine.29 Follow-up from 48h postpartum until menstruation is complete, accompanied by a traditional birth attendant (TBA). In line with qualitative research in Indonesia,30 the existence of TBA's in PNC is preferred by the community to midwives, therefore coverage is always low and services are interrupted between INC and PNC.
ConclusionThis model reinforces evidence and experiences of ongoing relationships between women, families, midwives/nurses as companions for emotional support. And more importantly, caseload, burnout, and psychological aspects between the two arise when the treatment process finds the key to satisfaction, hope, and new value from the current track record of childbirth experiences. This has a good impact on service utilization, equity, and accessibility. The practical implication is that the feasibility of a midwife-led CoC model to avoid leaving care, a collaboration between professionals and across sectors needs to be considered as a health welfare goal that is highly valued by women and their families.
Conflicts of interestThe authors declare no conflict of interest.
We would like to express our thanks to LPDP as the 2020 dissertation scholarship granter for funding this research.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.