Social capital is defined as the resources available to individuals and groups through membership in social networks. However, multiple definitions, distinct dimensions and subtypes of social capital have been used to investigate and theorise about its relationship to health on different scales, creating a confusing picture. This heterogeneity makes it necessary to systematise social capital measures in order to build a stronger foundation in terms of how these associations between the different aspects of social capital and each specific health indicator develop. We aim to provide an overview of the measurement approaches used to measure social capital in its different dimensions and scales, as well as the mechanisms through which it is presumed to influence health. Understanding the mechanisms through which these relationships develop may help to refine the existing measures or to identify new, more appropriate ones.
El capital social se define como los recursos disponibles para individuos y grupos gracias a su membresía en redes sociales. Sin embargo, varias definiciones, dimensiones y subtipos de capital social se han utilizado para investigar y teorizar sobre su relación con la salud a diferentes escalas, lo que genera un panorama confuso. Esta heterogeneidad hace necesario sistematizar las mediciones de capital social con el fin de obtener una base más sólida acerca de cómo se producen estas asociaciones entre los diferentes aspectos del capital y cada indicador específico de salud. Nuestro objetivo es proporcionar una visión general de los métodos de medición utilizados para medir el capital social en sus diversas dimensiones y escalas, así como los mecanismos mediante los cuales se presume que este influye en la salud. La comprensión de los mecanismos por los que esta relación se produce puede orientar el perfeccionamiento de las medidas existentes o la identificación de otras nuevas y más adecuadas.
The incorporation of social capital in the social determinants of health discourse has only increased, since it first appeared in the public health literature in the late 1990s. This is also evident in recent publications in Gaceta Sanitaria, which in 2015 motivated a methodological note on its measurement.1 The purpose of this paper is to take over from Villalonga-Olives and Kawachi's work1 to deepen in the measurement of social capital. Specifically, we aim to provide an overview to the measurement approaches used to measure social capital at different scales and to the mechanisms through which it is presumed to influence health with the final intention of offering new directions on how improved measures can help to obtain more trustworthy data.
A unified definition of social capital upon which all scholars agree is not available to date. Instead, multiple definitions, distinct dimensions and subtypes of social have been used to investigate and theorize about its relationship to health, creating a confusing landscape.1,2 Pierre Bourdieu, James Coleman and Robert Putnam have been referred to as the parents of the concept, yet, significant differences stem from their approaches. Bourdieu explains social capital in terms of social networks and connections. In his model, individuals’ network connections accrue shared norms and values, exchanges and obligations that can potentially provide access to different resources such as emotional, informational or instrumental support.3
Coleman defines social capital as a set of socio-structural resources “that have two characteristics in common: they all consist of some aspect of the social structure. And they facilitate actions of individuals who are within the structure”, and he continues “Unlike other forms of capital, social capital inheres in the structure of relations between persons and among persons. It is lodged neither in individuals nor in physical implements of production”.4 Contrary to Bourdieu, Coleman highlights the fact that social capital is a resource between families and communities, introducing a socio-structural approach. Putnam extends the scope of the collectivistic approach by including in the definition elements such as sense of belonging, community cooperation, civic engagement and norms of trust and reciprocity.5 The focus here is not in the individual, but in the community in which it is embedded.
Despite the differences, what all of them have in common and can be understood as the core of all social capital interpretations is “the presence of more or less structuralized networks between people or groups of people […] that facilitate certain actions for different actors within the structures”.6 Social capital, then, comprehend the resources that individuals can access thanks to their membership in a network, and includes both the resources accessible through direct, individual connections as well as the ones that are available to all the members of a given network thanks to the relationships within the network itself.7 Social capital represents a feature of the social structure, an ecologic characteristic whether we look at it from the individual (ego-centred) or collective (socio-centred) point of view. In studying the relationship of social capital and health, we should aim at understanding how these different resources and network characteristics influence individual and collective health.
A further relevant element of differentiation between Bourdieu's and Coleman's/Putnam's definition is the social framework within which relationships are understood. While Coleman and Putnam view on social capital departs from a rather static view of societies, Bourdieu's conceptualization of social capital is part of a more elaborated theory of conflict power distribution in society and, as such, entails that some of the potentially available resources may not be actually accessible. Authors like Carpiano, have pointed out that this is a relevant feature missing in the study of social capital in Public Health, which has mainly drawn upon Putnam's work (this is, overlooking aspects such as the availability of resources while intensively focusing on elements such as trust or reciprocity).8 As we shall discuss in the next paragraphs, these are the origins of the two main schools in the study of social capital in Public Health, namely the social cohesion and social network approaches*.
Social cohesion refers to the extent of closeness and solidarity within groups, and as such, the most used measures tap into indicators such as sense of belonging, trust and norms of reciprocity. The terms social capital and social cohesion sometimes confusing. We agree with Kawachi and Berkman that social cohesion is a broader concept than social capital, and includes: a) the absence of latent conflict and b) the presence of strong social bonds and solidarity–of which social capital is one aspect. Thus, one can have social capital without social cohesion but not social cohesion without social capital. Network-based approaches to social capital, in turn, attempt to map and characterize individual relationships (in terms of degrees of separation, nature of the ties, connectedness among the different actors, etc.) and the resources embedded in those network ties. These resources are typically referred to as social support and are classified according to different subtypes, including emotional, instrumental, appraisal and informational support.9 Although research normally restricts itself to one of these focuses, both dimensions are complementary and have been recognized and demonstrated to offer both benefits and downsides, although they unequivocally entail differences.1,2,10 The reader will notice that our proposal departs from the social cohesion approach to social capital, but also includes the consideration of social support as a fundamental element of social connections.
In order to better operationalize the complexity of social capital, several subconstructs have been differentiated.10 Discriminating between bonding, bridging and linking social capital allows to classify the links between the members of the group in terms of homogeneity. Bonding social capital refers to relations between members of a network that perceive themselves as being similar in terms of their shared social identity. Bridging social capital, by contrast, comprise relations of respect and mutuality between people who know that they are not alike in some socio-demographic (or social identity) sense (differing by age, ethnic group, class, etc.). Linking social capital introduces hierarchical or unequal relations, steaming from differences in power, resources or status.
A further differentiation is that of structural versus cognitive social capital. The structural component describes properties of the networks, relationships and institutions that bring people and groups together; while the cognitive dimension is derived from mental processes and reflects people's perceptions of the level of trust, confidence, and shared values, norms and reciprocity.1,10
Last, the scale which social capital is conceptualized at constitutes an additional point that needs to be addressed. Public health research has investigated the effect of social capital embedded in very diverse contexts, such as state or country level, neighbourhood, workplace or family. The mechanisms through which social capital may influence health at these different levels are not the same, and, in agreement, the measures used to capture social capital in each of the cases should not be the same either. Although the question of the variety of mechanisms underlying the relationship between social capital and health is beginning to be understood, more solid research is needed, as well as an extended debate and consensus about how we measure social capital at each scale.1
We suggest that using systematized social capital measures will allow to gain a stronger foundation on how the associations between the different aspects social capital and each specific health outcome occur and what the relationship of each of these with other social determinants of health is, since they are likely to be differently related.2,10,11 From here, a further understanding of the mechanisms through which they happen can orientate the refinement of the existent measures or the identification of new, more appropriate ones. Even when social capital is certainly dependent on the social and cultural context, a minimum degree of agreement about what aspects of social capital to measure and through which ways is indispensable to advance in social capital research. Context adaptation should then be conducted when necessary.
In the next sections, we review the mechanisms through which the association between social capital at these scales and health outcomes is thought to happen as well as the measures used to assess it.
Social capital at the macro level: country and state measuresTwo main pathways through which country/state level social capital is likely to influence health have been proposed:2
- •
Informal control and normalization of health-related behaviors, according to shared values of what is acceptable and desirable, thanks to which community members are able to maintain or achieve the desired goals.
- •
Enhanced collective efficacy and increased civic engagement in front of significant health-related issues, fruit of a cohesive community that is willing to intervene for common goods because of the mutual trust and solidarity among neighbors, including voting turnouts and advocacy efforts to influence policies that impact health outcomes.
The links between social capital and health at a state or country-level varies considerably across geographical regions. This is due to its strong correlation with income inequalities and also to the different interactions that the components of social capital and the particular institutional and political characteristics of different types of welfare states are thought to generate in relation to health outcomes.10,11 Whether these correlations are causal, mere interactions or mediated by confounders is not clear yet. Wilkinson and Pickett elaborated that income inequalities may cause a decrease in social capital.12 Work by Kawachi et al. provides a bases for this relationship, but proposes a different explanation: in a cross-sectional study based on data from 39 US states the authors found that the increased mortality seen as a result of income inequality was mediated by a disinvestment in social capital.13 States with a lesser egalitarian distribution of income showed higher level of social mistrust which, in turn, was associated with higher mortality rates. In this study, social capital was measured by two items from the General Social Survey, namely, per capita density of membership in voluntary groups in each state, and the level of social trust, estimated through the share of residents in each stated that agreed that people could be trusted. For both indicators, there was a correlation between social capital and age-standardized total and cause-specific mortality rates. The authors discuss whether poverty might be a potential confounder, and while they dismiss this hypothesis after adjusting for state poverty rates, educational attainment, age, race, urban/rural mixes are mentioned as further elements to take into account.
As mentioned earlier, also the institutional and political climate is very likely to influence this relationship. According to Rostila11 social-democratic regimes such as those in the Nordic Countries have implicit higher levels of universalism and solidarity, when compared to the other two regime types, namely the market-dominated liberal regime (in which state-protection is scarce and citizens are obligated to rely on personal connections to access more resources–as is the case of the US, UK or Ireland), and the conservative/corporativist type (where rights and benefits are strongly attached to class and status–as what happens in France, Germany or the Netherlands, among others). The Mediterranean regime (as represented in Spain, Italy, Greece and Portugal), is characterized by an even higher degree of familialism and a less developed social security system. Last, post-socialist regimes, such as those found in the postcommunist Eastern Europe show the lowest levels of social benefits, along with the highest levels of social inequalites and poverty. These differences in the sociopolitical landscape constitute strong structural forces that shape the effect that social capital at this level can have on health outcomes and, when possible, should be taken into account. Overall, the effect of social capital at the macro level seem to be interrelated with other social determinants of health and the state model, as well as with individual characteristics.2,11
Most of the first studies investigating the effect of social capital on health were conducted at a state/country level, departing from Putnam's social cohesion approach to social capital and encompassing measures of trust, civic engagement, reciprocity, informal control and perceived social support. Specific measures vary greatly depending on whether such measures have been designed for the specific purpose of gathering information about social capital or have been adapted from already existent questions within health surveys.2 In any case, macro-level social capital measure are mostly collected at the individual level and then aggregated to represent the collective, as in the former example by Kawachi et al. There have been attempts to develop strategies to obtain collective data at the meso level such as counting the number of individuals that would put a dropped letter back into the mailbox. At this scale, socio-centric network analysis is too difficult and costly to conduct.
Social capital at the meso level: neighborhood and community measuresNeighborhood level has been, by far, the scale at which social capital has been conceptualized the most. The pathways by which social capital at the meso level is presumed to exert a contextual effect on individual health are consistent with the ones described in the previous section, including some local specifics:2
- •
the diffusion of information on health-related questions,
- •
the maintenance of health-related norms through informal control,
- •
the promotion of access to local services and amenities, and
- •
the psychosocial processes that provide mutual support.
At these levels, several methodologic approaches have been used. The Framingham Study constitutes an excellent example from the social network perspective. Here, network influence on smoking, alcohol consumption, obesity and other health risks was examined in a longitudinal study from 1971 to 2003 by analyzing how being connected to obese individuals or smoking quitters affected the likelihood of people changing their behavior or BMI.14,15 Researchers were able to draw these relationships thanks to a detailed mapping of each participant's social network in terms of number of connections, their health situation, etc. In any case, socio-centered (or whole) network studies are not very common because of the elevated time and expenses involved.
Two reference-instruments to measure community social capital through health surveys are the World Bank's social capital Assessment Tool, SOCAT,16 and the Adapted social capital Assessment Tool, ASCAT,17 along with its short version, SASCAT. These questionnaires tap into questions such as group membership, social norms, civic engagement, social support and cognitive social capital (trust, sense of belonging, reciprocity and justice), and gather data at the individual level that can be aggregated to obtain collective results. Besides the robustness of such questionnaires, an additional strength of these tools is that they allow comparisons between studies, even when cultural adaptations have been made, as is the case of the work done within the Young Lives study.18 It is obvious that the different dimensions of social capital will take different forms in different contexts, hence they should be captured in the most representative way for each environment.
Social capital at the individual level: ego-centered measuresMechanisms through which ego-centered social capital may influence health include the following:2
- •
The provision of social support (both perceived and actual), in the form of emotional but also instrumental, appraisal and informational support.
- •
Social influence through shared norms or social control. Here face-to-face contact is not a requirement for social influence to occur. Nor is it a deliberate intention to modify other's attitudes or behaviors. On the contrary, people obtain normative guidance by comparing themselves’ to others within the same group.
- •
Social engagement and social participation, which result from the representation of the potential roles in real life. Being a parent, a friend, a worker, a sports fan… provides the individual with different resources and opportunities.
- •
Person-to-person contacts, which are especially relevant in infectious diseases through pathogen exposure, or certain behaviors such as secondhand cigarette smoke or shared food or drinks.
At this level, psychological (such as the effect of gratitude, loneliness or security on self-efficacy, self-esteem or depression) and physiological (like an increase of inflammatory markers of cortisol levels) mechanisms are ultimately responsible for their influence on health outcomes.
Again, measures used at this scale vary according to the chosen perspective to social capital: tools like Name Generators, the Position Generator19 or the Resource Generator20 are examples of instruments used from the social network approach. Position Generators assess the social resources to which an individual can gain access through its connection to somebody that, because of his or her occupation, is expected to embody valued resources represented by wealth, power and prestige. Resource Generators is more complex in its use, because it requires that the researcher defines the list of relevant resources beforehand. However, they can be more precise than Position Generators with regard to health outcomes, since they measure access to specific resources that are relevant to the outcome. Besides, they give information that can remain silent with position generators, such as the resources provided through home-based economies. Name generators are socio-metric measures that include a whole mapping of an ego-centered network and are considerably more time-consuming than the other two instruments. On the other hand, they are –obviously– more thorough, and unlike resource generators which typically focus on instrumental resources, put a greater emphasis on emotional support.19 Beyond these, many other approaches have been used to assess networks and social relationships, although some argue that the isolated use of these tools may omit upstream forces such the influence of society norms and values, the sociopolitical context or other socioeconomic factors such as poverty or inequality rates.
On the other extreme, social cohesion-based measures do not capture specific information about the respondent's social network. Rather, survey items inquire about the resources that individuals can gather thanks to their belonging to a group (at whatever level it is asked), through the assessment of their attitudes, cognitions and perception about the group (that is, cognitive social capital) on one hand, and of their actual behaviors of interaction, norms and participation (structural social capital) on the other. In this way, questions about social capital at the individual level from a social-cohesion perspective, equate the type of inquiries made through the same approach but at an ecological level (whatever the spatial area is defined as), and tap into questions such as trust, shared values and norms, perceptions of collective efficacy and informal control as part of cognitive social capital, and social interaction, civic engagement and social support concerning the structural dimension. Network approaches, when operationalized through surveys do not differ much from this perspective.9
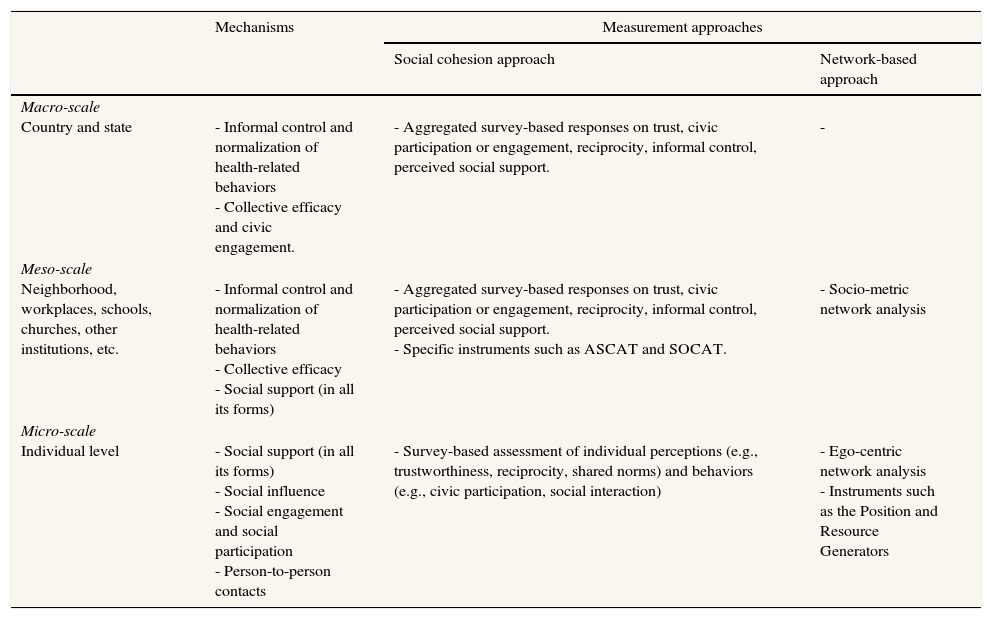
Table 1 provides a synthesis of this section, with the aim to clarify the different measures used to assess social capital according to the different approaches and scales of measurement, as well as the pathways through which it influences health in every case.
Measurement approaches and mechanisms through which social capital is thought to influence at the different scales.
| Mechanisms | Measurement approaches | ||
|---|---|---|---|
| Social cohesion approach | Network-based approach | ||
| Macro-scale Country and state | - Informal control and normalization of health-related behaviors - Collective efficacy and civic engagement. | - Aggregated survey-based responses on trust, civic participation or engagement, reciprocity, informal control, perceived social support. | - |
| Meso-scale Neighborhood, workplaces, schools, churches, other institutions, etc. | - Informal control and normalization of health-related behaviors - Collective efficacy - Social support (in all its forms) | - Aggregated survey-based responses on trust, civic participation or engagement, reciprocity, informal control, perceived social support. - Specific instruments such as ASCAT and SOCAT. | - Socio-metric network analysis |
| Micro-scale Individual level | - Social support (in all its forms) - Social influence - Social engagement and social participation - Person-to-person contacts | - Survey-based assessment of individual perceptions (e.g., trustworthiness, reciprocity, shared norms) and behaviors (e.g., civic participation, social interaction) | - Ego-centric network analysis - Instruments such as the Position and Resource Generators |
Source: own elaboration.
While some see the implicit divergences of social capital as a weakness of the concept and a limitation of its validity, others argue that they reflect the rich array of hypotheses that have been made with regard to social capital relationships to health and that, when empirically tested, they allow us to understand a greater diversity of pathways through which this association may happen and, thus, to explore the usefulness of the different approaches to explain health, as different researches have shown.2,16,17
When designing research to study this topic, it is essential to consider the theory behind social capital, its different dimensions and their relationship to health at every level. In this way, before choosing any measure of social capital one should consider the level at which variables will be measured and inferences wanted to be made; as well as through which mechanisms are thought to mediate these associations. Additionally, the more different dimensions an instrument is able to capture, the richer will be the data recalled and the more significant the analysis. Based on this premise, measures should ideally tap on both cognitive and structural and bonding, bridging and linking dimensions of social capital. When appropriate we also stress the usefulness of differentiating subdimensions of the former (i.e., sense of belonging, trust, social interaction, norms and values, etc.).
For example, if we were to study social capital and obesity at the community level all the four mechanisms above specified should be ideally taken into account. This means that, for instance, when looking for how the existing social norms may influence BMI and/or eating and physical behaviors, measures should be specifically focused on these norms that may influence these variables (and no others). Along the same lines, the specific norms that we will seek to identify will need to be relevant for the precise context in which research will be conducted. Social norms on body shapes, the social use of food or physical activity practices will be surely influenced by the sociocultural environment. In this sense, caution must be taken when importing social capital measures from different sociocultural and political contexts.
In the Spanish Health Survey, a macro level study, achieving this degree of precision in the measures is not possible (or even desirable), since multiple outcomes variables are normally considered and also different territories with slightly different social realities are included. In this sense, we agree with Villalonga-Olives and Kawachi that, beyond including specific questions to assess social capital, at least a positioning on the conceptualization of social capital and measures chosen is necessary to obtain reliable data and correctly interpret results.
Editor in chargeCarlos Álvarez-Dardet.
Authorship contributionsE. Carrillo Álvarez and J. Riera Romaní designed, wrote and revised the manuscript.
FundingThis paper is part of a research conducted with the support of a grant from the Spanish Training University Lecturers Programme (Formación de Profesorado Univeristario - FPU) from the Spanish Ministry of Education, Culture and Sports MECD (AP2010-3946).
Conflicts of interestsNone.
For a more detailed explanation on the genealogy and evolution of the concept of social capital in Public Health, see Moore S, Haines V, Hawe P, Shiell A. Lost in translation: a genealogy of the “social capital” concept in public health. J Epidemiol Community Health. 2006;60:729-34.