This is the first time that the effectiveness of cognitive-behavioural therapy for post-disaster stress (CBT-PD) in symptoms of posttraumatic stress disorder (PTSD) has been tested outside the United States of America.
DesignQuasi-experiment with three groups. In the quasi-control group, complete CBT-PD was applied even though its members did not have PTSD; in quasi-experimental conditions, participants received complete treatment because they had this diagnosis; and in the third group, participants with PTSD received an abbreviated treatment (double sessions) due to organisational requirements.
LocationPrimary health care workers in Constitución (Chile), city exposed to earthquake and tsunami; public department workers in Talca (city exposed only to earthquake) and teachers from a school (Constitución).
ParticipantsA total of 13 of the 91 people diagnosed with PTSD participated. In addition, 16 people without diagnosis voluntarily participated. The treatment was completed by 29 participants. There were no dropouts. Only 1 of the 9 participants in the quasi-experimental group did not respond to treatment.
InterventionsCBT-PD is a group therapy (10-12 sessions) that includes psychoeducation, breathing retraining, behavioural activation and cognitive restructuring. CBT-PD (complete and abbreviated) was applied between September and December 2010.
MeasurementsShort Posttraumatic Stress Disorder Rating Interview (SPRINT-E) was used to measure PTSD symptoms before and after treatment.
ResultsThe group that received the complete treatment and was diagnosed with PTSD showed a significant decrease in the total symptoms to below dangerous levels (IGAAB: 31.556; p<0.01; 95%CI: 0.21-2.01]; η2=0.709).
DiscussionThe effectiveness and benefits of incorporating CBT-PD in the health network after events like disasters were discussed.
Evaluar la eficacia de la terapia cognitivo-conductual para el estrés posdesastre (TCC-PD) en síntomas de estrés postraumático (TEPT) por primera vez fuera de los Estados Unidos.
DiseñoCuasiexperimental con tres grupos. Al grupo de cuasicontrol se le aplicó la TCC-PD completa pese a que sus miembros no tenían diagnóstico de TEPT; el grupo cuasiexperimental recibió el tratamiento completo porque sus miembros tenían ese diagnóstico. En el tercer grupo, las personas con TEPT recibieron un tratamiento abreviado (sesiones dobles) por exigencias organizativas.
EmplazamientoTrabajadores de atención primaria de salud de Constitución (Chile), ciudad expuesta al terremoto y tsunami; trabajadores de un servicio público de Talca (ciudad expuesta solo al terremoto) y profesores de escuela (Constitución).
ParticipantesParticiparon 13 de las 91 personas diagnosticadas de TEPT; además, 16 personas sin diagnóstico participaron voluntariamente. Finalizaron el tratamiento 29 personas. No se produjeron abandonos. Solo uno de los nueve participantes del grupo cuasiexperimental no respondió al tratamiento.
IntervencionesLa TCC-PD es una terapia grupal (10-12 sesiones) que incluye psicoeducación, reentrenamiento respiratorio, activación conductual y reestructuración cognitiva. Se aplicó TCC-PD (completa y abreviada) entre septiembre y diciembre de 2010.
Mediciones principalesPara medir síntomas de TEPT se utilizó la Short Posttraumatic Stress Disorder Rating Interview (SPRINT-E), antes y después del tratamiento.
ResultadosSolo el grupo que recibió el tratamiento completo y fue diagnosticado de TEPT disminuyó significativamente sus síntomas por debajo de los niveles peligrosos (IGAAB: 31,556; p<0,01; IC95%: 0,21-2,01]; η2=0,709).
ConclusionesSe comprueban la efectividad y los beneficios de incorporar la TCC-PD en la red de salud después de desastres.
On Saturday, February 27th (F-27), at 03:34 A.M. local time, there was an earthquake of 8.8 magnitude (Richter scale). Its epicenter was located at 35.909° South latitude and 72.733° West longitude, about 335 kilometers to the Southwest of Santiago, Chile.1 This earthquake was followed by a tsunami which caused huge destruction of the central coast of Chile, such as Constitucion and Talcahuano.2 Considering the location and intensity, the F-27 is one of the most important in world history. In fact, it is the sixth-strongest earthquake recorded since 1900.3 In Chile, the earthquake affected a large area where 80% of the national population lives and damaged a total of five hundred thousand houses, leaving about two million people affected.3 Authorities reported 521 deaths and 21 missing persons.4,5
Studies performed after the Chilean earthquake showed that peoples’ mental health was negatively affected.6–8 Considering this evidence, it raises the need to validate psychotherapeutic procedures that mitigate the psychological effects, especially the most important health problem after an event like F-27, post-traumatic stress disorder (PTSD).9–11 In fact, depending on the context, after an earthquake the prevalence of this disorder is between 10% and 30% at least one month after the catastrophic event.12–15 It is noteworthy that the number of symptoms after an earthquake is the same as after political violence.16 Specifically, after the F-27 the prevalence of PTSD was 12%, 6.4% for men and 14.8% for women.17 In cities directly affected by the earthquake and tsunami, the prevalence could be higher than 35%.7 Furthermore, it is expected that between 30% and 40% of the affected people in rural areas and between 10% and 20% of health care personnel present PTSD after F-27.18 Probably factors related to the degree of exposure (e.g., lack of social support, additional stress) and, to a lesser extent, pre-traumatic factors (e.g., female gender, previous trauma), are responsible for the variation in the prevalence of PTSD.19
According to DSM-IV, PTSD is an anxiety disorder. In contrast, for DSM-5, PTSD is included in a new group of disorders, the “trauma-and stressor-related disorders”.20 In both cases, PTSD is characterized by symptoms following exposure directly or indirectly (hear stories or see pictures) to extremely stressful and traumatic events, where people respond with fear, helplessness or intense horror. The traumatic event is re-experienced through flashbacks and uncontrollable dreams; this includes images, thoughts or perceptions. This produces an intense psychological distress associated with the avoidance of memories, dull (reluctantly) behavioral activation and physiological responses, which appear especially when the person is exposed to internal or external cues that symbolize or resemble an aspect of the traumatic event. Physiological arousal is so intense that it makes it difficult to fall or stay asleep, concentrate, and increases irritability, angry outbursts, hypervigilance and exaggerated startle responses. These changes could last more than 1month and cause clinically significant distress or impairment in social, occupational or other important areas of functioning. However, these symptoms do not always occur immediately after a disaster. Some improve with time, while others are maintained even 4 years later.16 In fact, the symptoms may appear 6 months after the traumatic event.21
In relation to the treatment of PTSD, it is important to note that not all treatments are equally effective in reducing the symptoms or remitting this disorder. However, trauma-focused cognitive-behavioral therapy, eye movement desensitization and reprocessing, stress management and group cognitive-behavioral therapy are the most effective in reducing PTSD symptoms.22 Although it has been shown that both psychotherapy and pharmacotherapy are useful in the treatment of PTSD, current evidence suggests that psychotherapy is more effective than pharmacotherapy.23 Of all psychotherapies, individual psychotherapy focused on trauma is the most effective, followed by the techniques of stress management and group cognitive-behavioral therapy. In particular, one of the most effective therapeutic procedures is the cognitive-behavior therapy that includes cognitive restructuration. Psychotherapy without a behavioral component (i.e., supportive psychotherapy, hypnosis, psychodynamic psychotherapy) has not proven effective.22,24,25
A cognitive-behavioral psychotherapy that has demonstrated to be effective for PTSD treatment after a natural disaster is the cognitive-behavioral therapy for post-disaster distress (CBT-PD).26–28 The effectiveness of CBT-PD was demonstrated by a quasi-experimental method in which the same treatment was applied to two groups (severe and moderate PTSD) measured on four different occasions (referral, pretreatment, intermediate and post-treatment). While the authors acknowledge that it would have been better to apply an experimental design to test the effectiveness of CBT-PD due to the presence of a control group, this was not feasible in the context of the treatment program in which the study was conducted.27
CBT-PD is a short-term group therapy (10-12 sessions), whose objective is to identify and to intervene in the maladaptive beliefs related to the disaster. The intervention includes four components: psychoeducation, breathing retraining, behavioral activation and cognitive restructuring. Clients receive a workbook and they complete assignments to reinforce the skills that they have learned in session.27 CBT-PD was used in a population with PTSD symptoms after the Katrina hurricane in New Orleans. The evidence shows that the number of severe PTSD symptoms decreased significantly immediately and during the first 5 months after the use of CBT-PD.27,28 However, the effectiveness of CBT-PD has never before been tested outside the United States. Furthermore, the quasi-experimental design used by the authors to test the effectiveness of treatment is not as suitable as in cases where control groups were used. Therefore, given the characteristics of F-27, the opportunity to implement this approach arose to prove the effectiveness of CBT-PD in a Latin American sample.
MethodSample and procedureThe design of this study was quasi-experimental with three groups, one of which was a quasi-control group. The sampling of this study was not probabilistic for two reasons. The first, there was the need to treat the largest number of people after the F-27; leave out someone for random selection criteria was discarded. The second, participation was always voluntary and depended on the willingness of people and organizations to receive this treatment. The people who participated in the CBT-PD were adults of both sexes from three different jobs. The people of the first group were medical healthcare workers living in the city of Constitucion (this group was exposed to the earthquake and tsunami). The people in the second group were public department workers from the city of Talca (this group experienced only the earthquake). The third group consisted of teachers from a school in Constitucion.
Initially, a diagnosis of PSTD was conducted using the SPRINT-E scale.28,29 The measurement was applied to all persons who wished to participate in the study. Seventy-one participants from the medical health center answered the questionnaire (21 men and 50 women), 75 employees from the public department (18 men and 57 women) and 10 from the primary school (3 men and 7 women).
Based on the diagnoses, 91 participants (34 from the health center, 51 from the public department and 6 from the primary school) met the primary criterion for entering treatment and they were invited to participate in the study. This criterion was to have at least three severe symptoms of PTSD (the other criterion was to be over 18 years old, which was met by all participants). However, being a voluntary activity, only 13 (14%) participated in the therapeutic process.
On the other hand, given the needs presented by the three organizations of this study, not all participants received the same treatment. Thus, 25 participants (7 from the health center and 18 from the public department) were treated with the Hamblen procedure, which consists of 10-12 sessions (one per week) between 60 and 90minutes; in this procedure, the activities proposed in the Manual Tasks were performed successfully in all sessions. Moreover, in the case of participants from the primary school, the procedure was concentrated in four sessions of 2hours and 30minutes, designed to end after a month; in this procedure, the activities described in the Manual Tasks were not carried out because of the participants’ workload.
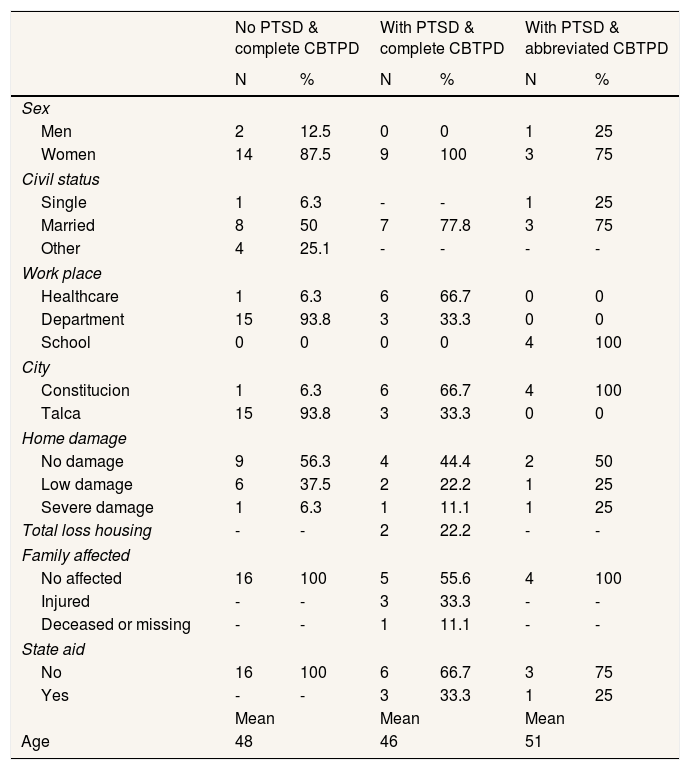
Since not all participants had severe symptoms and the same treatment was not applied, the 29 participants who completed treatment were put in three groups: the first called “no ptsd & complete cbtpd” with 16 participants, who had no more than three severe symptoms and received the original treatment; the second group, was called “with ptsd & complete cbtpd” and consisted of nine participants with more than three severe symptoms and received the original treatment; finally, the third group called “with ptsd & abbreviated cbtpd” consisted of four participants with more than four severe symptoms and who received the original treatment and the abbreviated procedure. Some demographic characteristics of samples are described in Table 1.
Demographic characteristics by posttraumatic stress disorder and cognitive-behavioral therapy for post-disaster stress levels.
| No PTSD & complete CBTPD | With PTSD & complete CBTPD | With PTSD & abbreviated CBTPD | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Sex | ||||||
| Men | 2 | 12.5 | 0 | 0 | 1 | 25 |
| Women | 14 | 87.5 | 9 | 100 | 3 | 75 |
| Civil status | ||||||
| Single | 1 | 6.3 | - | - | 1 | 25 |
| Married | 8 | 50 | 7 | 77.8 | 3 | 75 |
| Other | 4 | 25.1 | - | - | - | - |
| Work place | ||||||
| Healthcare | 1 | 6.3 | 6 | 66.7 | 0 | 0 |
| Department | 15 | 93.8 | 3 | 33.3 | 0 | 0 |
| School | 0 | 0 | 0 | 0 | 4 | 100 |
| City | ||||||
| Constitucion | 1 | 6.3 | 6 | 66.7 | 4 | 100 |
| Talca | 15 | 93.8 | 3 | 33.3 | 0 | 0 |
| Home damage | ||||||
| No damage | 9 | 56.3 | 4 | 44.4 | 2 | 50 |
| Low damage | 6 | 37.5 | 2 | 22.2 | 1 | 25 |
| Severe damage | 1 | 6.3 | 1 | 11.1 | 1 | 25 |
| Total loss housing | - | - | 2 | 22.2 | - | - |
| Family affected | ||||||
| No affected | 16 | 100 | 5 | 55.6 | 4 | 100 |
| Injured | - | - | 3 | 33.3 | - | - |
| Deceased or missing | - | - | 1 | 11.1 | - | - |
| State aid | ||||||
| No | 16 | 100 | 6 | 66.7 | 3 | 75 |
| Yes | - | - | 3 | 33.3 | 1 | 25 |
| Mean | Mean | Mean | ||||
| Age | 48 | 46 | 51 | |||
CBTPD: cognitive-behavioral therapy for post-disaster stress; PTSD: posttraumatic stress disorder.
Both treatments (full and abbreviated) were applied between September and December 2010. After sessions of therapy, seven workers from the health center, 18 from the public department (two men and 13 women) and four teachers from the primary school (one man and three women) completed the therapeutic procedure. A post-evaluation of PTSD symptoms with the SPRINT-E scale was performed at the end of the last session.
The therapists were six women with a degree in psychology. All of them were doing their thesis within the framework of this research. They were trained in the procedure previously. They were monitored weekly during the application of the CBT-PD. In their training and monitoring, therapists had the opportunity to share experiences, difficulties and learnings that emerged from the application of CBT-PD; this helped to standardize the treatment. Each treatment group received two therapists. All people participated voluntarily, received an informed consent (signed by each one) and gave permission to use their data. This study was approved by the Ethic Academic Council of the Faculty of Psychology, University of Talca.
InstrumentsIn order to measure the PTSD symptoms, the SPRINT-E (Short Posttraumatic Stress Disorder Rating Interview) was used.28 The first four items of this questionnaire referred to each of three groups of symptoms of DSM-IV, such as Criterion B “intrusive re-experiencing” (Item 1), Criterion C “avoidance and numbing” (items 2 and 3), Criterion D “hyperactivity” (item 4). Items 5 and 7 assess other important reactions related to PTSD, such as depression and healthy behavior, respectively. Items 6, 9 and 10 refer to the functional impairment in the person, resulting in questions about stress tolerance, performance in their daily work and social functioning, respectively. Moreover, the SPRINT-E has two items that assess the perception that each person has on needing help: item 8 refers to the personal concern for their reactions and 11 is directly related to the need for help. Finally, item 12 is used as a criterion of severity of diagnosis because it assesses suicidal intention. SPRINT-E has proved to be a reliable and valid scale in the Chilean context (after F-27), with an internal consistency and concurrent validity (all items are correlated with the Davidson Trauma Scale and construct validity with two factors).29 In respect to the measuring scale, each item of SPRINT-E is evaluated using a Likert scale from 0 (none) to 4 (very much) points, with the exception of item 12 (suicide intention), which is dichotomous (0 is “no” and 1 is “yes”), so it was removed from the analysis. Following the norms to use SPRINT-E,28 an item (any of its items) was considered as a PTSD intense symptom if its score was 3 or 4 points. Therefore, each participant has a total of intense symptoms. As additional data, SPRINT-E allows to evaluate PTSD cases, using the “rule of 3/7”: if a person reported three or more intense symptoms (three or more items with 3 or 4 points), it is very probably that he or she suffers from PTSD; in other words, there is a case of PTSD. Also, if it registered 7 points or more intense symptoms, the probability of a false positive (a person diagnosed with PTSD when, in fact, is not) is very low.28
Data analysisFirst, for the participants the total of intense symptoms was calculated. In order to determine if there are significant differences in the total of intense symptoms in the pre and post evaluation between groups, a two-factor analysis of variance with repeated measures (ANOVA-RM-AB) was performed. One factor, between-subject factor, was named “group” (composed by “no ptsd & complete cbtpd”, “with ptsd & complete cbtpd” and “with ptsd & abbreviated cbtpd” groups) and the other factor, repeated measures or within-subjects factor, was named “moment” (composed by “before” and “after” measures). Since in quasi-experimental designs the groups are already formed, it is not possible to balance or match them. That is, the groups probably have different sizes and their composition is not homogeneous (e.g., sex, age).30 Therefore, the ANOVA-RM assumptions could be violated and the classic F statistic could make more (or less) error than expected (p=0.05). This can increase the number of false positive or negative cases. In this study, the classic F and improved general approximation (IGA; p<0.05) statistics were analyzed to solve this problem. IGA has proven to be robust when all statistical assumptions are not met (e.g., homogeneity, normality, sphericity).31–33 In addition, tests of homogeneity of variances (Levene and Box; p<0.05), effect size (η2>0.5), statistical power (1–β>0.8) and difference of mean (mean difference I–J; p<0.05) were analyzed. Excepting IGA, all statistical tests were performed with SPSS version 14. From its original formulas, the IGA statistic was programmed in MATLAB 2007.33,34
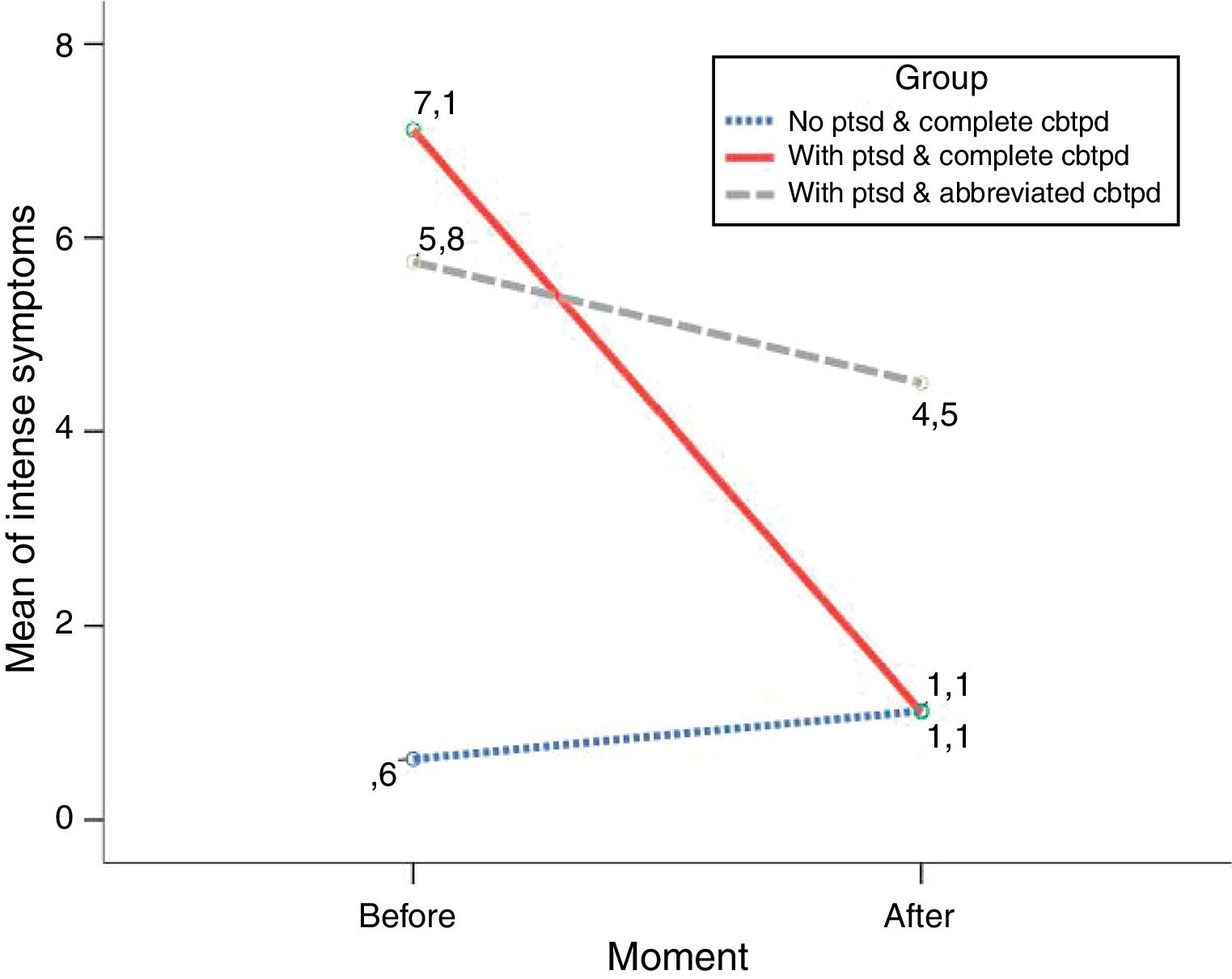
ResultsInitially, the means of severe symptoms of PTSD before applying the CBT-PD were 0.6 for the group “no ptsd & complete cbtpd” (SD=1.8), 7.1 for “with ptsd & complete cbtpd” (SD=2.2) and 5.8 for “with ptsd & abbreviated cbtpd” (SD=2.2). In turn, the means of severe symptoms of PTSD after applying the treatment were 1.1 (SD=1.4), 1.1 (SD=1.2) and 4.5 (SD=3.4) for groups “no ptsd & complete cbtpd”, “with ptsd & complete cbtpd” and “with ptsd & abbreviated cbtpd”, respectively.
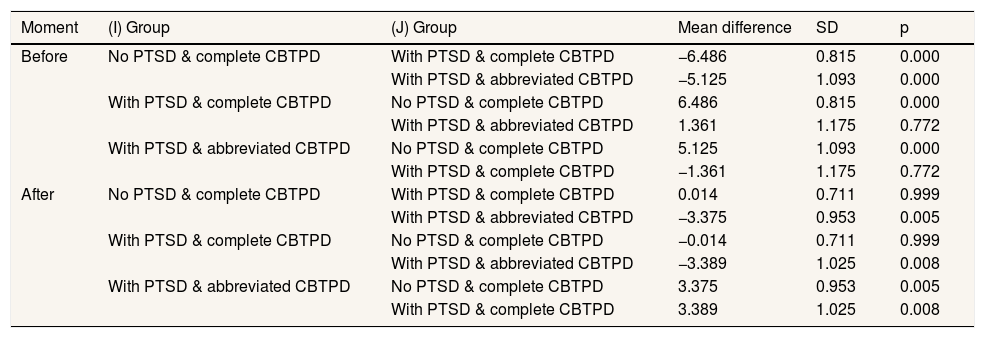
Regarding the ANOVA-RM-AB, the results indicate that the mean of intense symptoms of PTSD after CBT-PD was significantly lower than the mean of intense symptoms before therapy in both groups. Both, classic F and IGA statistics, agree on the existence of differences for the within-subjects factor “moment” (FB=27.757, p<0.01; IGAB=23.1457, p<0.01) and for the interaction between “group” and “moment” factors (FAB=31.556, p<0.01; IGAAB=31.556, p<0.01). Additionally, the statistical effect size and power for both are also high, with an effect for within-subjects factor (η2=0.516, 1–β=0.999) and an interaction effect (η2=0.709, 1–β=0.999). Specifically, the differences before and after were presented only in the “with ptsd & complete cbtpd” group (mean difference I–J=6, SD=0.656, 95%CI: 0.21-2.01, p<0.01). That is, only one of the nine participants in the quasi-experimental group did not respond to treatment. The differences noted above and plotted in Figure 1 are complemented by the multiple comparisons in Table 2. These comparisons identify differences between groups within each level of factor “moment”.
Multiple comparisons between means of each group, before and after treatment.
| Moment | (I) Group | (J) Group | Mean difference | SD | p |
|---|---|---|---|---|---|
| Before | No PTSD & complete CBTPD | With PTSD & complete CBTPD | −6.486 | 0.815 | 0.000 |
| With PTSD & abbreviated CBTPD | −5.125 | 1.093 | 0.000 | ||
| With PTSD & complete CBTPD | No PTSD & complete CBTPD | 6.486 | 0.815 | 0.000 | |
| With PTSD & abbreviated CBTPD | 1.361 | 1.175 | 0.772 | ||
| With PTSD & abbreviated CBTPD | No PTSD & complete CBTPD | 5.125 | 1.093 | 0.000 | |
| With PTSD & complete CBTPD | −1.361 | 1.175 | 0.772 | ||
| After | No PTSD & complete CBTPD | With PTSD & complete CBTPD | 0.014 | 0.711 | 0.999 |
| With PTSD & abbreviated CBTPD | −3.375 | 0.953 | 0.005 | ||
| With PTSD & complete CBTPD | No PTSD & complete CBTPD | −0.014 | 0.711 | 0.999 | |
| With PTSD & abbreviated CBTPD | −3.389 | 1.025 | 0.008 | ||
| With PTSD & abbreviated CBTPD | No PTSD & complete CBTPD | 3.375 | 0.953 | 0.005 | |
| With PTSD & complete CBTPD | 3.389 | 1.025 | 0.008 |
CBTPD: cognitive-behavioral therapy for post-disaster stress; PTSD: posttraumatic stress disorder; SD: standard deviation.
In addition, the Levene test indicates that the variance of four groups at time “before” is homogeneous (F=1.035, p>0.05), which does not occur with the variance of groups at the time “after” (F=4.359, p<0.05). Also, Box statistic (M=12,422, p>0.05) indicates that the variance-covariance matrices between the two measurement times are the same in all three populations defined by the factor “group”.
DiscussionThe results regarding the effect of CBT-PD show a significant reduction of PTSD in the group with severe symptoms and who received the original. The “with ptsd & complete cbtpd” group fell 6 points, achieving a score close to 1 at the end of therapy, almost two points below the limit considered by the “rule of 3/7”. This significant decrease is clarified when compared with the behavior of the other two groups. Both groups, the one that did not have severe symptoms of PTSD (with full treatment) and the one that did have symptoms (with abbreviated treatment), did not experience significant changes in the number of symptoms after treatment.
Therefore, it is possible to say that participants with more than three severe symptoms of PTSD that received the full course of CBT-PD benefited from it, decreasing their symptoms below the dangerous levels. However, other cause that explains this decline is the passage of time.35–37 In fact, 52% of the variance of PTSD symptoms was explained only by time. Of course, without the treatment, the explained variance would not have been 71% for the interaction between the passage of time and the treatment, which only decreased the symptoms of the quasi-experimental group. Given these results, there is evidence of the effectiveness of CBT-PD.
The theory that supports CBT-PD can explain the effectiveness of the treatment and the role of clients (patients) and therapists. From the theoretical point of view, CBT-PD is based on the cognitive behavioral model. In this model, the emphasis is on the creation of associations between symptoms with new ideas and rational thought to replace irrational beliefs about the traumatic event. These new associations require that the client gradually include new information to challenge these thoughts. Based on these principles, the therapy sessions are organized to give general information regarding the expected reactions after trauma until the cognitive restructuring necessary for processing the trauma. This whole process was accompanied by a change in symptoms, unpleasant feelings, behavior, and unpleasant reactions that were facilitated by breathing retraining and behavioral activation. In this way, the cognitive-behavioral psychotherapeutic model has proved to be very effective for the treatment of phobias, anxiety, quality of life and depression;38–40 this, regardless whether the therapy is administered face to face or on-line.40–42
On the other hand, as a therapeutic group process, clients could affect other members of the group. In that sense, the social support that the therapeutic group provides serves as a modulator of the stressful event.43–45 In other words, social support reduces stress for each client and allows them to better learn breathing techniques and cognitive restructuring.
Moreover, in the CBT-PD, clients are active agents in their recovery and therapists are coaches and facilitators of the recovery process. In fact, for sessions of CBT-PD patients and therapists require two different manuals specifically designed for each.46–48 The patient's manual contains, session by session, the explanation of the therapeutic processes and activities that will be carried out both at home and in therapy sessions. On the other hand, the therapist's manual explains in detail each session both conceptually and procedurally, giving recommendations about what and how to do each session based on theory and others’ experiences.
Although findings are consistent with CBT-PD theory, since participants were not randomly assigned to groups, we do not rule out the existence of alternative explanations for the efficacy of treatment. For example, the motivation of the participants to complete the therapeutic procedure and tasks could increase the effectiveness of a procedure in which patients voluntarily attend. In addition, aforementioned social support was not a controlled factor at all in the therapeutic procedure. This support is evident, at least in the form of the therapy group and the fact that groups were not only attended by people with a diagnosis of PTSD. However, the results obtained in relation to the abbreviated CBT-PD model applied to the quasi-control group are an argument for the effectiveness of the full procedure. Probably the longer duration of sessions and the little time to do homework made participants more fatigued and they learned less.
Regardless of the CBT-PD effectiveness, an important feature of this study is that this is the first time that the procedure created by Hamblen47 is tested in a sample outside the USA, where it was originally developed. It is also the first time that it has been tested in cases of PTSD after an earthquake and tsunami. This reinforces the evidence accumulated and reflected in the meta-analysis on the effectiveness of cognitive-behavioral therapies in treating PTSD. Second, it also reinforces the idea that symptoms can be decreased in a similar therapeutic procedure beyond the traumatic event. In fact, in this particular case, the therapist and client manuals were only adapted to include examples and information about earthquakes and tsunamis, mainly in the psycho-education session.
About the limitations of this study, these are related to the samples of people tested and the number of measurements. In respect to the samples, although the differences suggest that these samples were enough, it is true that the groups “no ptsd & complete cbtpd” and “with ptsd & complete cbtpd” were (respectively) four times and twice the size of the group “with ptsd & abbreviated cbtpd” (the quasi-control group). Unfortunately, the availability of participants who wanted to finish the therapeutic process played against the balance of the groups. However, since it satisfies the assumption of homogeneity of variances and the sphericity is not applicable in this case (only two steps are repeated), the failure to have balanced groups should not be a problem for testing the robustness.33 On the other hand, it would be interesting to compare other people from different populations, for example, people belonging to an at-risk group or people affected by the F-27.18,49 In relation to the number of measurements, it is important to make new ones and more after treatment. This to determine if the effects of therapy are maintained or not after months and even years. However, the evidence found in other quasi-experiments show that the decreasing tendency of PTSD symptoms is maintained after 4 months,27 therefore we did not find convincing arguments that the opposite will happen here.
Finally, it is important to keep in mind for future therapeutic applications of this type, the importance of measuring the effects of treatments in populations affected by mental health problems in general and effects of traumatic events in particular. It is important to remember that not all therapeutic procedures are appropriate in all cases and may even be harmful,23 to illustrate, after the F-27 earthquake and tsunami, the psychosocial interventions were not coordinated and did not measure their effects.8,50 For these reasons, it is a public health matter to have action plans that integrate effective mental health treatment procedures.
In this regard, if the primary care network has effective therapeutic procedures it could treat the psychological consequences of disasters such as the F-27.18 In fact, because CBT-PD is a group therapy, it allows one psychologist to assist several people per hour, which does not occur with individual psychotherapeutic models. Given the results presented here, the potential of CBT-PD cannot be ignored by our primary care network and health authorities.
Editor in chargeClara Bermúdez-Tamayo.
Authorship contributionsM. Leiva-Bianchi contributed with conception and design, analysis and interpretation of data, drafting the article, and final approval of the version to be published. F. Cornejo contributed with analysis and interpretation of data, drafting the article and revising it critically for important intellectual content. A. Fresno contributed drafting the article and revising it critically for important intellectual content. Finally, C. Rojas and C. Serrano contributed with acquisition of data and drafting the article.
AcknowledgementsOur acknowledgements to “U. Talca Psychosocial Impact Teamwork” and “U. Talca Cognitive-Behavioral Therapy Team” for their participation in data collection and psychotherapy performance respectively.
FundingThis research was supported by the Quality of Life and Healthy Environments Research Program of University of Talca (grant: VAC 600426); Young Researchers Program of University of Talca (grant: VAC 600535); Regular FONDECYT project (grant: 1160301).
Conflicts of interestsNone.