To describe and compare the health status between vulnerable population participating in a program to tackle energy poverty (Energía, la justa) and the non-energy poor Barcelona (Spain) population and to analyse among participants the effect of energy poverty intensity on health.
MethodCross-sectional study based on data from program participants obtained before the intervention. Participants (1799 women and 671 men) were compared to non-energy poor population of Barcelona (1393 women and 1215 men) sampled from the Barcelona Public Health Survey (2016). Standardized prevalence and prevalence ratios of self-perceived poor health, asthma, chronic bronchitis, and depression and/or anxiety were estimated, and among participants the association between health status and energy poverty intensity was estimated with multivariate models.
ResultsThe probability of poor self-perceived physical and mental health ranged from 2.2 to 5.3 times greater in the program participants than non-energy poor Barcelona population. Among program participants, those most affected were found to be the most likely to report poor health outcomes, regardless of other sociodemographic factors.
ConclusionsThe prevalence of poor physical and mental health was considerably higher among women and men participating in the programme compared to the non-energy poor population and was even worse among those who were more severely affected. Public policies that tackle energy poverty and its consequences are urgently needed in Spain.
Describir y comparar el estado de salud entre la población vulnerable que participa en un programa de lucha contra la pobreza energética (Energía, la justa) y la población sin pobreza energética de Barcelona (España), y analizar entre las personas participantes el efecto de la intensidad de la pobreza energética en la salud.
MétodoEstudio transversal basado en datos de los/las participantes en el programa obtenidos antes de la intervención. Se compararon los/las participantes (1799 mujeres y 671 hombres) con población sin pobreza energética de Barcelona (1393 mujeres y 1215 hombres) seleccionada de la Encuesta de Salud Pública de Barcelona (2016). Se estimaron la prevalencia estandarizada y las razones de prevalencia de mala salud, asma, bronquitis crónica y depresión o ansiedad autopercibida. Entre los/las participantes se estimó la asociación entre el estado de salud y la intensidad de la pobreza energética con modelos multivariantes.
ResultadosLos/las participantes presentaron entre 2,2 y 5,3 veces peores resultados en salud que la población sin pobreza energética. Entre los/las participantes se encontró que las personas más afectadas eran las que tenían más probabilidades de reportar peores resultados de salud, independientemente de otros factores sociodemográficos.
ConclusionesLa prevalencia de mala salud física y mental era considerablemente mayor en las mujeres y los hombres que participaron en el programa en comparación con la población sin pobreza energética, y era aún peor entre los/las más severamente afectados. En España se necesitan con urgencia políticas públicas que aborden la pobreza energética y sus consecuencias.
Energy poverty is a significant social problem in the European Union (EU) being the Eastern and Southern EU countries the most affected.1 This problem has become more evident in the Southern EU countries after the bursting of the housing market bubble in 2008, the subsequent Great Recession and the concomitant austerity policies,2 as exemplified in Greece3 and Spain.4 Energy poverty is a dynamic, multidimensional phenomenon that can be defined as a household's inability to ensure socially and materially required levels of domestic energy services.5 There is widespread recognition that the interaction of three drivers constitutes the critical determinant of energy poverty: the socioeconomic situation of the household, the energy performance of the dwelling, and the energy prices.6 These drivers are, in turn, influenced by more structural determinants such as energy, housing and labour policies and markets, economic policies, and welfare states.7
Southern European regions despite having a warmer climate are among the most vulnerable to energy poverty. Two distinctive structural determinants account for this high vulnerability.2,7,8 First, the social protection system within the welfare state regime, which is described as fragmented and poor developed, has revealed less ability to counteract unfair living conditions when primary social networks, mainly the family, are unable to assist individuals.9 Second, the lack of adequate heating systems and the poor quality of dwellings contribute to the higher prevalence in the southern European region.1 Such a situation is attributable to the interaction between deficient housing policies and the market-oriented housing production that prioritises its exchange-value over its use-value. The latter negatively affects people's right to affordable, adequate, and quality housing.
There are two widely recognised approaches to measuring energy poverty: household income/expenditure-based indicators and survey-based consensual indicators with a binary logic according to household self-assessment about the presence or absence of energy poverty drivers.10 The consensual approach can capture more comprehensive elements of energy poverty, such as social exclusion and material deprivation. In contrast, it is less accurate in capturing severity and persistence of energy poverty, since it may differ from household to household depending on the affected dimensions such as access, affordability and needs, among other factors.5 Furthermore, the energy poverty does not occur as an isolated problem. It is frequently experienced in combination with other housing problems or insecurities in other vital areas as work/employment and food.11 For example, people at risk of poverty experience day-to-day difficulties in fulfilling their essential needs like food, housing, utilities, and health costs.12 As a result of their limited opportunities and challenges in balancing reduced household budgets, they are likely to suffer adverse health consequences, an issue that needs to further exploration.
Energy poverty has severe health and health inequality implications.13,14 The critical pathways of energy poverty to ill-health are the poor thermal and humidity conditions, inadequate dwelling quality, and the unaffordability of domestic energy services.13 These conditions have been associated with higher excess winter mortality and morbidity due to respiratory15–17 and cardiovascular diseases;18 poor mental health and well-being;19 and the exacerbation of existing health conditions.13,14 These adverse health effects are unequally distributed among different population groups. Children, the elderly, women, immigrants, and the lower-class population are more vulnerable to energy poverty, widening health inequalities.14,20 In contrast, the evidence for the southern EU regions is scarce and mostly based on European comparative studies.2,21–23 Hence, there is a lack of evidence on health inequalities between social groups. For example, low-income women, such as single-parent families, are at a disproportionate risk of poverty and are more susceptible to energy poverty.24 Also, the responsibility for the care and household tasks still falls mainly on women, often making them responsible for managing energy debts or requesting subsidies. Women's health could be more adversely affected because gender patterns expose them to spending more time at home with harmful indoor environments and the stress or feelings of helplessness associated with the energy poverty managing.25
Energía, la justa (EJUSTA) was a pilot programme to tackle energy poverty conducted in Barcelona in 2016. It was implemented by the city council and local non-governmental organisations. EJUSTA aimed to reduce inadequate and unaffordable household energy and to improve health targeting vulnerable populations attended by the city social services. An opportunity was provided to evaluate this program, both its effectiveness and the experience perceived by the participants, and this paper presents the baseline study with the following aims: to describe and compare the health status between vulnerable population participating in EJUSTA program and the non-energy poor Barcelona population and to analyse among participants the effect of energy poverty intensity on health.
MethodDesign, study population, and information sourcesA cross-sectional study of the vulnerable population affected by energy poverty in Barcelona city participant of EJUSTA program or the non-energy poor population of Barcelona (from now on BCN) to compare the health status.
Two sources of information were used: 1) the EJUSTA Survey database, contain the baseline information of the EJUSTA participants, those were recruited consecutively at public social service offices during the 5-months (March to July 2016) of the execution of the program, and 2) the database of the Barcelona Public Health Survey (BPHS) 2016 edition. BPHS provides information from a representative sample of non-institutionalised Barcelona population obtained with a multi-stage random sampling. The questionnaire used was adapted from the BPHS using the same validated items.26 So, identical health measures were included in both surveys along with demographic, socioeconomic, housing and energy poverty questions. Trained independent interviewers delivered the survey in both population face to face (only one member per household).
For the present study, EJUSTA participants that wished to receive free home energy counselling visits were also invited to participate in the research and their informed consent obtained. Individuals who declined to participate in the study also received the intervention. Inclusion criteria were ≥18 years, signed the informed consent and affected by energy poverty based on the consensual approach:21 inability to keep the home warm or inability to pay utility bills on time or presence of dampness and rot in the dwelling. Of 3094 participants, 2470 met the selection criteria (204 did not sign the informed consent; 248 were non-energy poor; 172 unknown energy-poor condition). The BCN individuals were sampled from the BPHS following the criteria of ≥18 years and people not affected by energy poverty using the same energy poverty measures but in the reverse sense. Therefore, individuals with one or more energy poverty indicator was excluded. Of the 4000, 2608 met the criteria (560 were <17 years, 799 reported at least one energy poverty measure, 33 unknown energy-poor condition).
The Clinical Research Ethics Committee has approved the study protocol of Parc de Salut Mar (Number 2016/6681/I).
Study variablesFour physical and mental health outcomes were analysed in this study. Self-reported health was measured using the question “How is your health in general?”, and the answer was categorised as good (excellent, very good, and good) and poor (fair, and poor). This has proven to be a good indicator of health status, health service utilisation and, mortality.27 Presence or absence of asthma, chronic bronchitis and depression and/or anxiety in the previous 12 months were measured. Among the self-reported morbidity indicators, respiratory morbidity and the mental health disorders stand out for the high concordance between the registers and the self-reported values.28,29
The main independent variable was energy poverty measured by three self-reported questions:21 “Could your household afford to keep the dwelling heated at an appropriate temperature during the winter months?”, “Has your household been in arrears on utility and community bills in the past 12 months?” and “Does your dwelling have any leaks, dampness on the walls, floors, ceilings or in the foundations, or rotten floors, windows or door frames?”. The answers were combined to create two variables: 1) “EP (de)composition”: a variable with seven categories based on all the combinations of the EP measures. 2) “EP intensity”: a 3-point categorical variable: “low EP” (yes in one measure); “moderate EP” (yes in two of them); and, “high EP” (yes in all).
Relevant covariables included were age, sex, place of birth (Spain and EU-15; outside the EU-15); household composition (one-person household; couple without children; couple with children; single parent; other); educational level (less than primary; primary; secondary or more); employment status (employed; unemployed; retirees and pensioners; permanent disability); and ability to face an unexpected financial expense of €750 or more (yes/no) that provide information about of individuals’ preparation against financial risks.30 Tenure status (owner; tenant; social housing) was also measured because of its relationship with dwelling conditions.
Statistical analysisA descriptive analysis of all the variables in EJUSTA and BCN samples was conducted. Pearson's χ2 test tested the significance of the differences between the groups. The prevalence of age-standardised health outcomes was calculated for both groups using the direct method, with the age distribution of the EJUSTA sample as a reference in both populations. Next, the prevalence ratios (PR) and their 95% confidence intervals (95%CI) for all health outcomes were estimated using Poisson regression models with robust variance adjusted by age.
As a sensitivity analysis, all the analyses were repeated, selecting non-energy poor manual class adult population from BPHS. Social class was measured using the Spanish Society of Epidemiology's classification,31 which is based on the current or last occupation. Then, the responses were classified as a non-manual class and manual class. We sampled the manual class population without any energy poverty measures. Results can be found in Table I in online Appendix.
Among the EJUSTA sample, a descriptive analysis of the energy poverty measures was performed. Then, the prevalence of age-standardised health outcomes by energy poverty intensity level we calculated. The association between poor health outcomes and energy poverty intensity was analysed by estimating the PR and their 95%CI for all health outcomes by using Poisson regression models with robust variance. The included explanatory variables were all covariables, except the inability to face an unexpected expense of €750 or more, because of collinearity with energy poverty intensity. Orthogonal polynomial contrasts were used to test the gradient association between poor health outcomes and energy poverty intensity.
All the analysis was carried out stratifying by gender, using the statistical software STATA13.
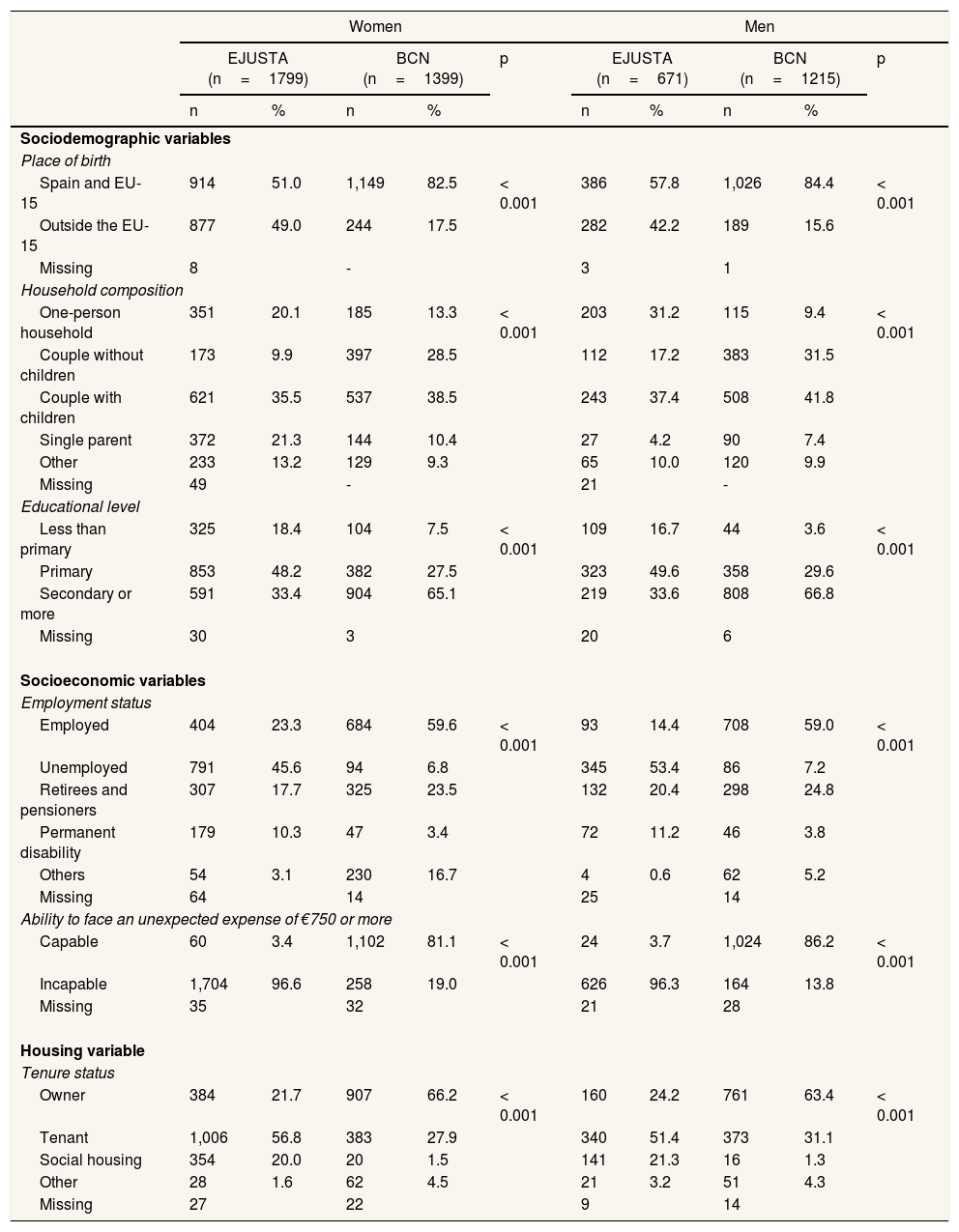
ResultsTable 1 shows substantial differences in the demographic, socioeconomic and housing characteristics between the EJUSTA participants and the BCN. For example, the number of people born outside the EU-15 was close to half in the EJUSTA (women, 49.0%; men, 42.2%), but was much lower in the BCN (women, 17.5%; men, 15.6%). Single mothers among the EJUSTA doubled that of the BCN (21.3% versus 10.4%, respectively). Both educational attainment and socioeconomic position were lower in the EJUSTA than in the BCN, and most participants in the EJUSTA were tenants (women, 76.8%; men 72.7%), while most of BCN were owners (women, 66.2%; men 63.4%).
Sociodemographic, socio-economic, and housing characteristics of the EJUSTA participants and the Barcelona non-energy poor population, stratified by sex. Barcelona, 2016.
| Women | Men | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| EJUSTA (n=1799) | BCN (n=1399) | p | EJUSTA (n=671) | BCN (n=1215) | p | |||||
| n | % | n | % | n | % | n | % | |||
| Sociodemographic variables | ||||||||||
| Place of birth | ||||||||||
| Spain and EU-15 | 914 | 51.0 | 1,149 | 82.5 | < 0.001 | 386 | 57.8 | 1,026 | 84.4 | < 0.001 |
| Outside the EU-15 | 877 | 49.0 | 244 | 17.5 | 282 | 42.2 | 189 | 15.6 | ||
| Missing | 8 | - | 3 | 1 | ||||||
| Household composition | ||||||||||
| One-person household | 351 | 20.1 | 185 | 13.3 | < 0.001 | 203 | 31.2 | 115 | 9.4 | < 0.001 |
| Couple without children | 173 | 9.9 | 397 | 28.5 | 112 | 17.2 | 383 | 31.5 | ||
| Couple with children | 621 | 35.5 | 537 | 38.5 | 243 | 37.4 | 508 | 41.8 | ||
| Single parent | 372 | 21.3 | 144 | 10.4 | 27 | 4.2 | 90 | 7.4 | ||
| Other | 233 | 13.2 | 129 | 9.3 | 65 | 10.0 | 120 | 9.9 | ||
| Missing | 49 | - | 21 | - | ||||||
| Educational level | ||||||||||
| Less than primary | 325 | 18.4 | 104 | 7.5 | < 0.001 | 109 | 16.7 | 44 | 3.6 | < 0.001 |
| Primary | 853 | 48.2 | 382 | 27.5 | 323 | 49.6 | 358 | 29.6 | ||
| Secondary or more | 591 | 33.4 | 904 | 65.1 | 219 | 33.6 | 808 | 66.8 | ||
| Missing | 30 | 3 | 20 | 6 | ||||||
| Socioeconomic variables | ||||||||||
| Employment status | ||||||||||
| Employed | 404 | 23.3 | 684 | 59.6 | < 0.001 | 93 | 14.4 | 708 | 59.0 | < 0.001 |
| Unemployed | 791 | 45.6 | 94 | 6.8 | 345 | 53.4 | 86 | 7.2 | ||
| Retirees and pensioners | 307 | 17.7 | 325 | 23.5 | 132 | 20.4 | 298 | 24.8 | ||
| Permanent disability | 179 | 10.3 | 47 | 3.4 | 72 | 11.2 | 46 | 3.8 | ||
| Others | 54 | 3.1 | 230 | 16.7 | 4 | 0.6 | 62 | 5.2 | ||
| Missing | 64 | 14 | 25 | 14 | ||||||
| Ability to face an unexpected expense of €750 or more | ||||||||||
| Capable | 60 | 3.4 | 1,102 | 81.1 | < 0.001 | 24 | 3.7 | 1,024 | 86.2 | < 0.001 |
| Incapable | 1,704 | 96.6 | 258 | 19.0 | 626 | 96.3 | 164 | 13.8 | ||
| Missing | 35 | 32 | 21 | 28 | ||||||
| Housing variable | ||||||||||
| Tenure status | ||||||||||
| Owner | 384 | 21.7 | 907 | 66.2 | < 0.001 | 160 | 24.2 | 761 | 63.4 | < 0.001 |
| Tenant | 1,006 | 56.8 | 383 | 27.9 | 340 | 51.4 | 373 | 31.1 | ||
| Social housing | 354 | 20.0 | 20 | 1.5 | 141 | 21.3 | 16 | 1.3 | ||
| Other | 28 | 1.6 | 62 | 4.5 | 21 | 3.2 | 51 | 4.3 | ||
| Missing | 27 | 22 | 9 | 14 | ||||||
EJUSTA participants: participants in Energia, la justa program affected by energy poverty; BCN: Barcelona non-energy-poor population.
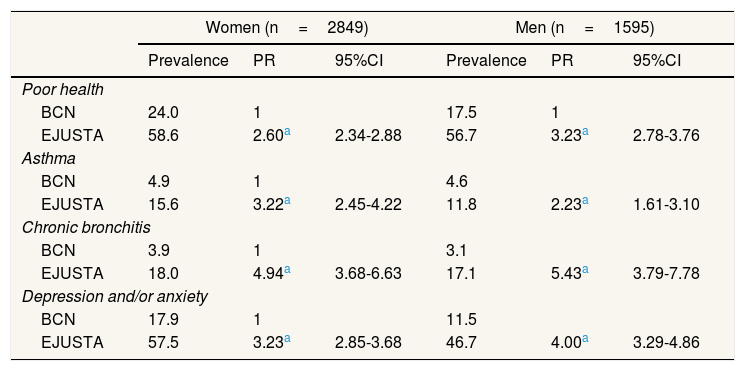
The EJUSTA reported worse health conditions than the BCN in all physical and mental health outcomes (Table 2). Women reported a higher prevalence in all health outcomes in both populations, although we did not observe gender-differentiated association patterns. The probability of experiencing poor health was several times higher in the EJUSTA sample than in the BCN sample. The strongest associations were found in chronic bronchitis and depression and/or anxiety. The corresponding PRs were 4.94 (95%CI: 3.68–6.63) for women and 5.43 (95%CI: 3.79–7.78) for men in the case of chronic bronchitis and PR 3.23 (95%CI: 2.85–3.68) for women and 4.00 (95%CI: 3.29–4.86) for men in the case of depression and/or anxiety. The sensitivity analysis performed using a subsample of BCN manual social class revealed similar association patterns (Table I in online Appendix). The most noteworthy associations were again found in chronic bronchitis and depression and/or anxiety.
Age-standardised prevalence (%) and adjusted prevalence ratio (PR) of physical and mental health in the EJUSTA participants compared with the Barcelona non-energy poor population, stratified by sex. Barcelona, 2016.
| Women (n=2849) | Men (n=1595) | |||||
|---|---|---|---|---|---|---|
| Prevalence | PR | 95%CI | Prevalence | PR | 95%CI | |
| Poor health | ||||||
| BCN | 24.0 | 1 | 17.5 | 1 | ||
| EJUSTA | 58.6 | 2.60a | 2.34-2.88 | 56.7 | 3.23a | 2.78-3.76 |
| Asthma | ||||||
| BCN | 4.9 | 1 | 4.6 | |||
| EJUSTA | 15.6 | 3.22a | 2.45-4.22 | 11.8 | 2.23a | 1.61-3.10 |
| Chronic bronchitis | ||||||
| BCN | 3.9 | 1 | 3.1 | |||
| EJUSTA | 18.0 | 4.94a | 3.68-6.63 | 17.1 | 5.43a | 3.79-7.78 |
| Depression and/or anxiety | ||||||
| BCN | 17.9 | 1 | 11.5 | |||
| EJUSTA | 57.5 | 3.23a | 2.85-3.68 | 46.7 | 4.00a | 3.29-4.86 |
EJUSTA: participants in Energía, la justa program affected by energy poverty; BCN: Barcelona non-energy-poor population. 95%CI: 95% confidence interval; PR: prevalence ratio.
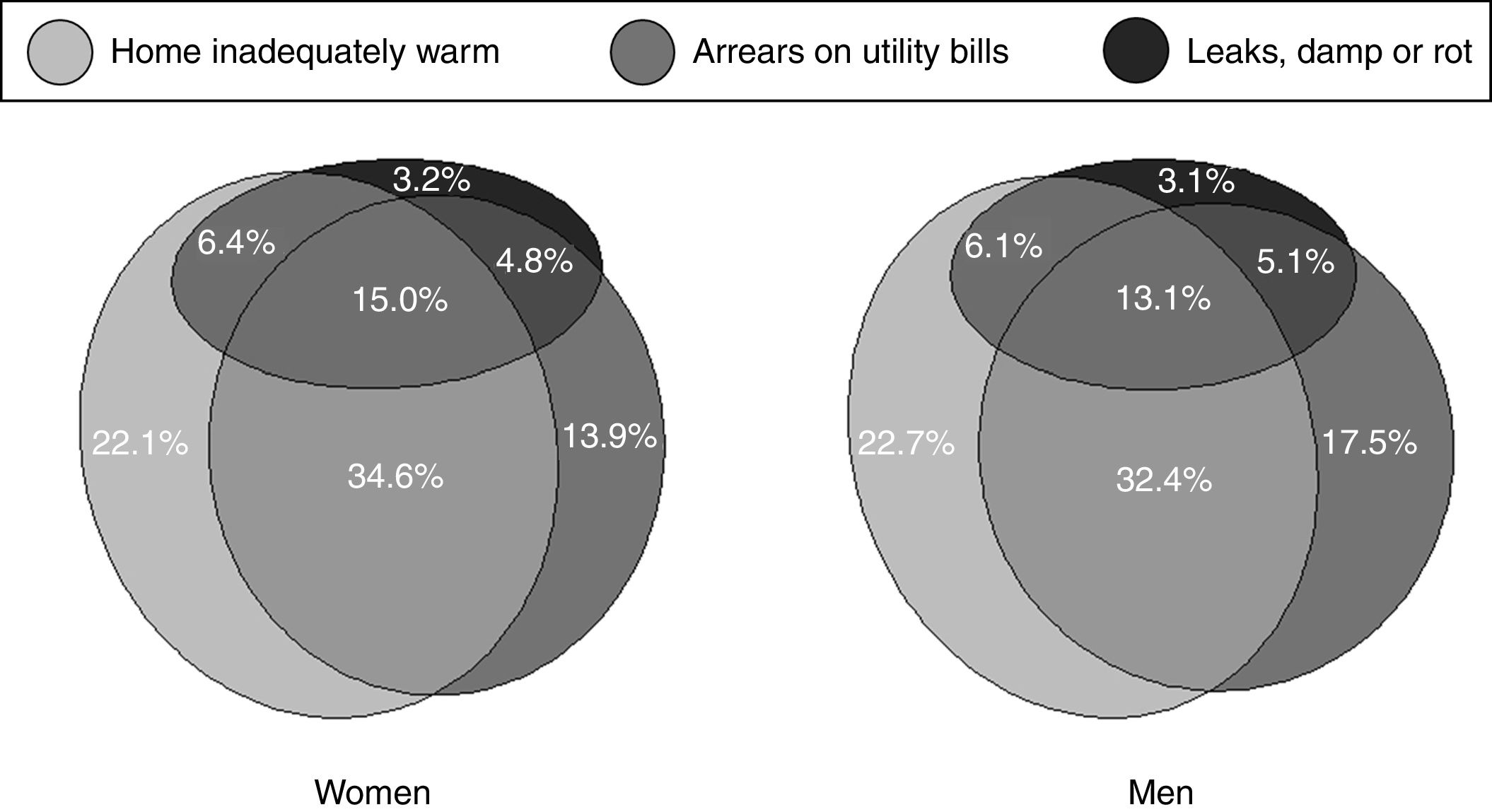
A high proportion of EJUSTA participants reported that they could not afford to keep their households adequately warm (women, 78.0%; men, 74.8%) and a high proportion of them had arrears on utility bills (women, 68.3%; men, 68.1%). The leaks, damp or rot indicator was less frequently reported (women, 29.5%; men, 27.4%). The Euler diagram in Figure 1 shows the impact according to the measured dimensions of energy poverty, displaying a substantial but not homogeneous overlap.
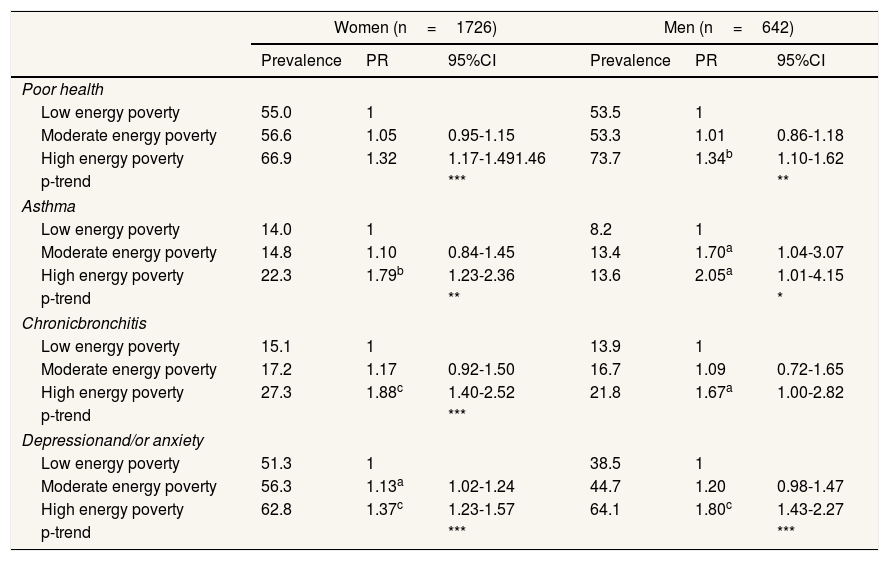
Table 3 shows the association between energy poverty intensity and health status among the EJUSTA sample. For most health variables, point estimates of PRs were indicative of a gradient association. The linear trend test confirmed them, except for chronic bronchitis in men. For all health indicators, there were significant differences in poor health between low energy poverty and high energy poverty. Depression and/or anxiety in women and asthma in men were statistically significant at all energy poverty intensity levels.
Prevalence (%) and adjusted prevalence ratio of physical and mental health by energy poverty intensity in the EJUSTA participants, stratified by sex. Barcelona, 2016.
| Women (n=1726) | Men (n=642) | |||||
|---|---|---|---|---|---|---|
| Prevalence | PR | 95%CI | Prevalence | PR | 95%CI | |
| Poor health | ||||||
| Low energy poverty | 55.0 | 1 | 53.5 | 1 | ||
| Moderate energy poverty | 56.6 | 1.05 | 0.95-1.15 | 53.3 | 1.01 | 0.86-1.18 |
| High energy poverty | 66.9 | 1.32 | 1.17-1.491.46 | 73.7 | 1.34b | 1.10-1.62 |
| p-trend | *** | ** | ||||
| Asthma | ||||||
| Low energy poverty | 14.0 | 1 | 8.2 | 1 | ||
| Moderate energy poverty | 14.8 | 1.10 | 0.84-1.45 | 13.4 | 1.70a | 1.04-3.07 |
| High energy poverty | 22.3 | 1.79b | 1.23-2.36 | 13.6 | 2.05a | 1.01-4.15 |
| p-trend | ** | * | ||||
| Chronicbronchitis | ||||||
| Low energy poverty | 15.1 | 1 | 13.9 | 1 | ||
| Moderate energy poverty | 17.2 | 1.17 | 0.92-1.50 | 16.7 | 1.09 | 0.72-1.65 |
| High energy poverty | 27.3 | 1.88c | 1.40-2.52 | 21.8 | 1.67a | 1.00-2.82 |
| p-trend | *** | |||||
| Depressionand/or anxiety | ||||||
| Low energy poverty | 51.3 | 1 | 38.5 | 1 | ||
| Moderate energy poverty | 56.3 | 1.13a | 1.02-1.24 | 44.7 | 1.20 | 0.98-1.47 |
| High energy poverty | 62.8 | 1.37c | 1.23-1.57 | 64.1 | 1.80c | 1.43-2.27 |
| p-trend | *** | *** | ||||
95%CI: 95% confidence interval; PR: prevalence ratio.
Note: All prevalence ratios were adjusted by age, place of birth, household, employment status, education level and tenure status.
a p < 0.05.
b p < 0.01.
c p < 0.001.
p-trend: orthogonal polynomial linear contrast.
ap-trend <0.05.
bp-trend <0.01.
cp-trend <0.001.
Note: Energy poverty intensity: “low energy poverty” (one energy poverty indicator); “moderate energy poverty” (two energy poverty indicators); and “high energy poverty” (all energy poverty indicators).
This study shows that the vulnerable population affected by energy poverty in a southern European city was disproportionately women, immigrants, people with low levels of education, unemployed and tenants. These population suffered a strikingly higher prevalence of poor self-perceived health, respiratory and mental morbidity compared to the non-energy poor population. Moreover, among those suffering from energy poverty, the most severely affected were found to be the most likely to report poor health outcomes, regardless of other sociodemographic factors.
Health status among EJUSTA and non-energy poor populationThe vulnerable populations studied reported severe adverse physical, and mental health outcomes compared to the non-energy poor population. The results support the findings of previous studies showing that low-income people, particularly women,24 lower social classes, immigrants, and tenants, are more exposed to the structural determinants of energy poverty and its health consequences.14,20 As previously noted, the household's inability to ensure the required levels of domestic energy services tends to coexist with other problems,11,12 like financial difficulties, unemployment, and residential insecurity. The population studied was a socially disadvantaged subpopulation whose health is likely to worsen as more and more social problems coexist. There is abundant evidence of the association between health and socioeconomic status.32 However, this does not fully explain the association found between energy poverty and poor physical and mental health. The sensitivity analysis performed, as well as the energy poverty assessment by intensity level, confirmed this association. Both results support the conception of energy poverty as a condition related, but different from other socioeconomic vulnerabilities.33 These results were consistent with the evidence found in previous studies related to asthma,15,17 chronic bronchitis,16 and poor self-perceived health and mental health problems,14,19 suggesting the problem goes beyond the mere existence of economic poverty or material deprivation.
Association between energy poverty intensity and health status among EJUSTAAmong the EJUSTA population, the self-reported energy poverty indicators showed a pervasive but uneven overlap in their dimensions. It was noted that the higher the energy poverty intensity, the higher the prevalence in almost all health problems studied. However, the energy poverty affects health through different pathways. For example, respiratory problems have been related to poor dwelling conditions.17 In contrast, mental health problems have been more closely linked to worry about debt and affordability, thermal discomfort and concern about its health consequences.19 Such a suggestive pattern merits further exploration, not only about energy poverty intensity patterns suggested but also how the different pathways combined affect people's health. In future research, this approach should also address the inability to keep the home cool in summer, a problem that may become relevant in coming years given the climate change but remains relatively under-explored within EU.34
Limitations and strengthsThe main limitation was the existence of multiple confounding factors between the target and comparison populations, threatening its external validity. Although extrapolation of the health burden related to energy poverty should be done with caution, the evidence gathered from the analysis of the energy poverty intensity suggests an unequivocal and consistent relationship with several health outcomes. The sample was useful and a good first approach, but the comparison group far from ideal. Another limitation is the reliability and accuracy of the self-perceived energy poverty measures used due to possible reporting bias. For example, households that would be empirically identified as energy-poor with other metrics, may not identify themselves as energy-poor or may deny their circumstances.33 In any case, the measures were asked identically in both populations. Lastly, this study may show a selection bias due to the non-random sample used among EJUSTA participants. For example, the sample did not include people in extreme socioeconomic circumstances affected by energy poverty who were not social service users (e.g. illegal immigrants, squatters, or people in extreme poverty). If these population groups had been included, the health outcomes would probably have been worse and the health associations even more substantial.
Despite these limitations, this is the first study analysing the association between energy poverty intensity and health in the context of Southern Europe. The advantages of a composite indicator that compares energy poverty level across households its ability to capture a multidimensional concept that often is appraised on separate components.35 and poorly studied in relation with health status. This composite indicator, although “rudimentary”, has allowed revealing how the energy poverty level was associated in gradient-shaped with different health outcomes. This approach may offer to policymakers the opportunity to design programmes according to the level of energy poverty, considering its possible associated health consequences.
ConclusionThis study highlights the shocking health inequalities among the vulnerable population adversely affected by the energy poverty in an urban context in the south of the EU. In Southern European regions tailored programmes to reduce energy poverty are urgently needed because energy poverty is more likely to change in the short term than income poverty, as factors other than income can be addressed to alleviate energy poverty. Such an approach should, at the same time, also be tackled as a matter of social justice. Therefore, targeted policies and programmes to alleviate energy poverty should coexist with broader structural policies aimed at improving living, working, and housing conditions. Both strategies combined would reduce health effects and health inequalities in populations affected by multiple social deprivations.
Energy poverty is a severe problem in Eastern and Southern European countries. Living in energy poverty is associated with poor physical and mental health. However, most of the evidence was gathered in other European contexts, which display differences both in climatic conditions and economic and political structural determinants.
What does this study add to the literature?Vulnerable populations affected by energy poverty in a Southern European city showed high prevalence of poor self-perceived health, respiratory and mental morbidity. Moreover, the higher the energy poverty experienced, the greater the probability of physical and mental health problems.
Carlos Álvarez-Dardet.
Transparency declarationThe corresponding author on behalf of the other authors guarantee the accuracy, transparency and honesty of the data and information contained in the study, that no relevant information has been omitted and that all discrepancies between authors have been adequately resolved and described.
Authorship contributionsStudy conception, planning, analysis, interpretation, and writing: J. Carrere. Study conception, insights for the analysis, and interpretation and writing: A. Peralta, L. Oliveras, M.J. López, M. Marí-Dell’Olmo, J. Benach and A.M. Novoa. All authors gave final approval and agree to be accountable for all aspects ensuring the integrity and accuracy of the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. This article forms part of the doctoral dissertations of J. Carrere, at Universitat Pompeu Fabra, Barcelona.
FundingThe study was partly funded by a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain), awarded on the 2015 call under the Health Strategy Action 2013-2016, within the National Research Programme oriented to Societal Challenges, within the Technical, Scientific and Innovation Research National Plan 2013-2016, with reference PI15/02006, co-funded with European Union ERDF funds (European Regional Development Fund).
Conflicts of interestNone.
The authors thank the Associació Benestar i Desenvolupament and the Associació Ecoserveis for their support, particularly to Mònica Plana Izquierdo. Joan Benach gratefully acknowledges the financial support by ICREA under the ICREA Acadèmia programme.